 |
 |
- Search
| Neurospine > Volume 15(3); 2018 > Article |
|
|
Abstract
Background/Aims
The Dynesys-Transition-Optima (DTO) hybrid system was designed to achieve arthrodesis and stabilization in patients with lumbar degeneration. Satisfactory outcomes were demonstrated previously. However, no study has evaluated the effects of using the DTO system in patients with lumbar spondylolisthesis or stenosis.
Methods
This retrospective study included 35 consecutive patients with multilevel lumbar degeneration with or without spondylolisthesis who underwent surgery using the DTO system. Imaging studies included pre- and postoperative radiography, magnetic resonance imaging, and computed tomography. The clinical outcomes were measured by Japanese Orthopedic Association (JOA) scores, Oswestry Disability Index (ODI) scores, and a visual analogue scale (VAS) for back and leg pain.
Results
Thirty patients (85.7%) with a mean age of 61.9 years completed the follow-up, with a mean duration of 35.1 months. There were 21 patients in the spondylolisthesis group and 9 in the stenosis group. The spondylolisthesis group had worse functional scores than the stenosis group preoperatively. After DTO surgery, all patients showed significant improvements in clinical outcomes, including VAS for back and leg pain, ODI, and JOA scores (p < 0.05). There were no significant differences in clinical outcomes between the 2 groups. At a 2-year follow-up, lumbar alignment was well maintained in both groups (p = 0.116). There were no significant differences in lumbar alignment between the 2 groups.
Instrumented spinal fusion surgery has been thought as the standard treatment for patients with degenerative disc disease or instability caused by severe lumbar spondylosis refractory to conservative treatment. Various approaches of surgical intervention, including anterior, posterior, transforaminal, and lateral lumbar interbody fusion techniques, have demonstrated satisfactory surgical outcomes in patients with degenerative spondylolisthesis, spinal stenosis with instability, facet joint arthropathy, degenerative disc disease, or recurrent lumbar disc herniation [1-7]. Although there are still issues with this surgical treatment, spinal arthrodesis with instrumentation has been a popular choice of surgical management for various lumbar spondylosis [8-12].
In recent decades, there has been an emerging option of instrumentation for lumbar spondylosis with preservation of spinal segmental motion. The Dynesys dynamic stabilization system (Zimmer Spine, Minneapolis, MN, USA) consists of a pedicle screw-based device for motion preservation and stabilization for the lumbar spine. The Dynesys was designed to unload the intervertebral disc and to shift axial loading to the elastic spacers of the system. Thus, unloading or rehydration of the degenerative discs might be expected in selected patients [13]. The concerns of this nonfusion instrumentation are durability, though several reports have demonstrated promising outcomes without significant adverse effects of Dynesys [13-18]. However, some patients with severe spondylosis may need not only dynamic stabilization but also fixation for more than 2 disc levels. The Dynesys-Transition-Optima (DTO) (Zimmer Spine) hybrid stabilization and fusion system allows the dynamic stabilization to be performed in the adjacent level to fusion. In the previous literature, Maserati et al. [19] followed 22 patients who underwent DTO stabilization and fusion for a midterm period in 2009. Their results demonstrated satisfactory outcomes with significant improvements. However, the radiographic and clinical outcomes of DTO in long-term follow-ups are still not definitive.
The purpose of the current study was to address the results of DTO, using radiographic and clinical outcomes, in a long-term follow-up. All of the patients experienced spondylolisthesis or stenosis and were followed-up for more than 2 years. This is the first report focused on radiographic evaluations after DTO and its clinical impacts.
Consecutive patients with symptomatic lumbar spondylolisthesis or stenosis who underwent posterior decompression and DTO hybrid dynamic stabilization and fusion system in Taipei Veterans’ General Hospital, Taiwan between 2011 and 2013 were reviewed retrospectively. The clinical presentations of patients in the series included mechanical low back pain, focal radiculopathy, or neurogenic claudication. The pathologies included spinal stenosis with spondylolisthesis, foraminal stenosis, hypertrophy of yellow ligament, sagittal imbalance with segmental scoliosis, and degenerative disc disease. Patients were excluded if there was a severe medical condition, coronary artery disease, cerebral vascular accident, or malignancy. Moreover, those patients who were lost to follow-up or did not complete evaluations at each time point were also excluded from data analysis. This study was approved by the institutional ethics committee in Taipei Veterans General Hospital (VGH#IRB 201012024IC). Every patient freely signed an informed consent form.
The patient was placed in a prone position with adequate or acquired lumbar lordosis (LL) under general anesthesia. A floor-mounted surgical table with Wilson frames was adjusted and applied accordingly. A midline skin incision was made for standard decompression, with total laminectomy and discectomy in selected levels. The narrow lateral recesses with hypertrophic ligamentum flavum were decompressed with Kerrison’s rongeur and probed through to ensure that the nerve roots were free from compression. The facet joints were preserved without violation at dynamic stabilization levels, except that the medial one-third of the facets were resected in selected cases to achieve adequate decompression. After decompression, the junctions of the transverse process and lateral facet joint were exposed for pedicle screws. The DTO pedicle screws were then placed in selected levels with standard techniques. Intraoperative fluoroscopy was then applied for confirmation. The interbody fusion cage was then placed after discectomy at selected level.
The diameter and length of the titanium alloy screws were estimated by both computed tomography (CT) scans preoperatively and pedicle sounding probes intraoperatively. Due to the self-tapping design of the Dynesys screws, we avoided pulling back and reinserting the screws. After placement of all screws, we would adjust the height of Wilson’s frame to get the most appropriate LL for the patient. Subsequently, the polycarbonate urethane spacers of appropriate lengths were then assembled with the polyethylene-terephthalate (PET) cords. The PET cord was connected to a standard titanium rod for fixation and fusion at one end. The length of the elastic spacer was measured by the pedicle distraction gauge to ensure neutral lordosis in the indexed levels of the lumbar spine during extension. The tension cord inside the spacer aimed to provide controlled forward flexion movement. Theoretically, all patients were stabilized with an ideal neutral lordosis after DTO hybrid stabilization and fusion system.
Our database was built prospectively with scheduled clinical and radiological examinations for selected patients at each clinical visit. Standard pre- and postoperative questionnaires and clinical evaluations were aimed to be completed at 1.5, 3, 6, 12, and 24 months after surgery and with a 12-month interval thereafter. The functional evaluation included Japanese Orthopedic Association (JOA) scores and Oswestry Disability Index (ODI) scores. The pain scores included visual analogue scores (VAS) for back and leg pain, respectively. All the subjective questions were answered by patients themselves with assistance from our special study nurses. The objective assessment was performed by the 2 special study nurses under the supervision of the physicians.
All patients underwent preoperative standard anteroposterior and dynamic lateral radiographs, magnetic resonance imaging (MRI), and CT scans for evaluation. Postoperative follow-up included both plain and dynamic radiographs at 1.5, 3, 6, 12, and 24 months after surgery and every 12 months thereafter. Follow-up CT and MRI were undertaken at approximately 18 and 24 months after surgery.
The LL was measured by a standing lateral radiograph. The Cobb angle between upper endplate of L1 and S1 was defined as LL. All these image studies were reviewed through the Smart-Iris digital medical imaging system (Taiwan Electronic Data Processing Co., Taipei, Taiwan). Two radiologists and 2 neurosurgeons reviewed the images independently and the coauthors made the final decision if there was any ambiguity among interpretations.
All statistical analyses were performed using IBM SPSS ver. 18.0 (IBM Co., Armonk, NY, USA). Independent t-tests and paired t-tests were used for continuous variables, and the Fisher exact test was applied for categorical data. The chi-square test was used for 2 variables relation verification. A p-value of 0.05 was considered to be statistically significant.
Among the 35 consecutive patients who underwent DTO hybrid dynamic stabilization and fusion system in this series, 30 patients (85.7%) completed the clinical and radiological evaluations for more than 24-month postoperation. Their mean age was 61.9±12.9 years at the time of surgery; 13 (43.3%) were male and 17 (56.7%) were female patients (Table 1). The mean follow-up duration was 35.1±7.0 months. Three patients (10.0%) had the habit of smoking. Past health histories of diabetes, hypertension and osteoporosis were documented in 11 (36.7%), 16 (53.3%), and 10 patients (33.3%), respectively (Table 1).
Of the 30 patients analyzed, 15 (50.0%) underwent 2-disc-level, 10 (33.3%) underwent 3-disc-level, and 5 (16.7%) underwent 4-disc-level DTO after decompression. A total of 230 screws and 44 cages were inserted in this series. Twenty-one patients (70.0%) had lumbar spondylolisthesis and 9 (30.0%) had stenosis or herniated discs. The distribution of levels that underwent Dynesys dynamic stabilization varied from L2 through to S1, as demonstrated in Table 2.
The overall mean LL was 36.6° before surgery. The mean LL were 39.1° (p=0.053) and 42.6° (p=0.166) at postopeative 1- and 2-year follow-up. There were no significant differences of mean LL between pre- and postoperative follow-up. All the patients could maintain their LL at 2-year follow-up.
All patients in the present series had satisfactory improvement after surgery. The disability scores, which included JOA and ODI scores, improved significantly after surgery at 24-month postoperation when compared to preoperation. The JOA scores were 5.6±3.9 before and 13.6±1.7 after surgery (p<0.05). The ODI scores were 21.2±9.8 before and 2.7±3.9 after surgery (p<0.05).
In general, all patients had a significant decrease in pain scores (VAS of back and leg pain) after surgery at 24-month postoperation when compared to preoperation (Fig. 1). The VAS scores for back pain were 5.7±3.1 before and 0.4±1.1 after surgery (p<0.05). The VAS scores for leg pain were 5.0±3.1 before and 0.9±1.7 after surgery (p<0.05).
There were 21 patients in the spondylolisthesis group and 9 patients in the stenosis or herniated discs group. The distributions of age, habit of smoking, diabetes mellitus, hypertension, and osteoporosis were not different between the 2 groups (p=0.280, p=0.328, p=0.429, p=0.404, p=0.656, respectively) (Table 3). However, females were slightly predominant in the spondylolisthesis group (p=0.018). The mean LL between the 2 groups was not different before and after surgery (p=0.179 and p=0.181). Both groups could maintain their LL at 2-year follow-up.
The JOA and ODI scores were worse in the spondylolisthesis group than the stenosis group before surgery. The JOA scores were 3.6 vs. 8.0 (p=0.011) and ODI scores were 35.1 vs. 17.0 (p=0.019). The postoperative JOA scores were 12.4 vs. 13.0 (p=0.631) and ODI scores were 4.4 vs. 2.9 (p=0.547). There was no difference between the 2 groups. Both groups had significant improvement in the disability scores after DTO surgery.
The VAS pain scores for back and leg pain were similar in the 2 groups before surgery. The VAS for back pain was 6.5 vs. 5.1 (p=0.350) and VAS for leg pain was 5.0 vs. 5.1 (p=0.900). The postoperative VAS for back pain was 1.3 vs. 0.9 (p=0.686) and VAS for leg pain was 0.9 vs. 0.8 (p=0.928). There was no significant difference between the 2 groups. Both groups had significant improvement in VAS pain scores after hybrid dynamic stabilization and fusion system (Table 3, Fig. 2).
During follow-up, 2 female patients (6.7%) with L3–4–5 spondylolisthesis in the series had symptomatic screw loosening and underwent reoperation to revise the implants in the first years after the DTO surgery [14,15]. One was 45 years old and the other was 60 years old. These 2 patients remained free of symptoms related to spinal stenosis and had satisfactory outcomes up to 36 months of follow-up. No other secondary surgery, including infection, revision to spinal fusion, pseudoarthrosis, or decompression for adjacent segment disease, was performed during the follow-up period.
The current study analyzed 30 patients with lumbar spinal stenosis who underwent decompression and the DTO hybrid system. A total of 80 disc levels were treated with stabilization or fusion. The overall mean lordosis was 36.6° before surgery and 39.1° (p=0.053) and 42.6° (p=0.166) at postoperative 1- and 2-year follow-up. There were no significant differences of mean LL between pre- and postoperative follow-ups. All of the patients with or without spondylolisthesis could maintain LL at 2-year follow-up. The intergroup difference at each time point was not significant. The overall segmental range of motion (ROM) in pre- and postoperative were demonstrated in Table 4.
The clinical outcomes for all patients were also satisfactory. The JOA scores were 5.6 before and 13.6 after surgery (p<0.05). The ODI scores were 21.2 before and 2.7 after surgery (p<0.05). The VAS scores for back pain were 5.7 before and 0.4 after surgery (p<0.05). The VAS scores for leg pain were 5.0 before and 0.9 after surgery (p<0.05). The patients with spondylolisthesis had worse disability scores before surgery. The mean age of this group was not significantly older than the stenosis group (63.9 vs. 57.4, p=0.280). This represented spondylolisthesis having a more adverse impact on the patient’s functions. However, the disability and pain scores were not different between the 2 groups after DTO surgery. Both the patients with and without spondylolisthesis had satisfactory outcomes at 2-year follow-up.
The DTO system was designed to be used in a patient with multilevel lumbar spondylosis, in which some levels needed fusion and some levels needed stabilization only. Maserati et al. [19] conducted a study of 24 patients with multilevel lumbar spondylosis who underwent DTO hybrid stabilization and fusion in a single institute in 2010. These patients demonstrated improvement in mean VAS pain scores from 8.8 to 5.3 (p-value not shown). He then concluded the promising application of DTO in multilevel spondylosis patients. Our current study demonstrated overall significant improvement in both disability scores and pain scores after surgery (p<0.05). Hereby, we could conclude that DTO was effective in patients with multilevel lumbar spondylosis.
In an aging society there could be an increasing number of patients with multilevel lumbar spondylosis. Lee et al. [20] compared 15 patients who underwent DTO hybrid surgery and 10 patients who underwent fusion only surgery in 2015. All the patients had 2-level surgery. These patients demonstrated slight improvement in global lordosis (T12–S1) from -32.3° before to -31.5° after surgery (p=0.86). Their DTO hybrid group also demonstrated significant clinical improvement after surgery. In our study, we studied more patients with more severe lumbar spondylosis. Fifteen of all of the patients (50%) had 3- or 4-level lumbar degenerative disease. Our global LL also demonstrated a trend to increase the lordosis, although the differences were not significant. We also concluded that the patients with 2- or multilevel lumbar spondylosis could at least maintain an ideal and neutral LL 2 years after surgery. The clinical outcomes were also satisfactory in patients with 2 or more levels of lumbar degeneration.
In 2016, Kashkoush et al. [21] conducted a study of 66 patients with 2-level lumbar spondylosis who underwent DTO surgery. For 52 of them (78.8%) it was the first time to receive surgery, and 14 (21.2%) were from failed back syndrome. Ten patients (15.2%) needed fusion surgery and underwent revision of stabilized segments. The clinical outcomes were not mentioned. In comparison to our study, the revision rate was slightly higher (6.7%). In one published study of our group in Taipei Veterans’ General Hospital, the revision rate was 1.4% (1 of 70 patients) [22]. The complication was operation-site infection with osteomyelitis. The patient finally underwent surgery to remove all the implants. The study is the first to mention the overall facet arthrodesis rate of 54.3%. All of the patients had satisfactory clinical outcomes.
Spine fusion surgery is still the treatment of choice for patients with symptomatic spondylosis refractory to conservative treatment [8-12]. However, in selected patients with mixed conditions of degeneration, hybrid dynamic stabilization and fusion would be more suitable. One of our patients, a 34-year-old male, had L4–5–S1 spondylosis. Two levels of disc were desiccated with protrusion or migration. Microdiscectomy without fusion could be applied at L4–5. Due to bilateral spondylolysis, discectomy and interbody fusion would be applied at L5–S1. Before the period of the DTO hybrid system, the selection of treatment would be 1 or 2 levels fusion surgery. We would have been concerned about the adjacent segmental disease if we chose fusion at L5–S1. On the other hand, we would have been concerned about the more extensive surgery if we picked 2-level interbody fusion. The current study demonstrated that the DTO hybrid system was a more appropriate treatment for the young adult (Fig. 3). Finally, we chose the dynamic stabilization and fusion system. The patient then could have solid fusion at L5–S1 and stabilization at L4–5 simultaneously. The clinical and radiographic outcomes were both satisfactory.
Another patient, 66 years old, with L1–2–3–4 degeneration underwent DTO surgery in our institute. She had symptomatic disc degenerative disease at L1–2–3 and spondylolisthesis at L3–4. The 3 discs were all desiccated with variable degrees of herniation. Solid fusion at L3–4 would lead to proximal segmental degeneration. Interbody fusion at all 3 levels would be feasible but a longer operation time and much estimated blood loss were inevitable. After discussion with the patient and her family, they decided to receive the DTO system. The surgeon then chose dynamic stabilization at L1–2–3 and fusion at L3–4 (Fig. 4). A shorter operation time and less blood loss than standard 3-level lumbar interbody fusion were noted (data not shown). Also, the LL was well maintained by dynamic stabilization. Both the disability and pain scores improved significantly. The pre- and post-X-rays and MRIs were demonstrated to compare segmental ROM and disc condition (Figs. 5, 6).
The dynamic stabilization was designed to unload the intradisc pressure. To prove this, our research team conducted a study in 2013. The index discs were measured by signal intensity of MRI called calibrated disc signal (CDS). Pre- and postoperative MRI images were compared, focusing on the condition of the bridged discs The CDS of bridged discs was found to be higher after Dynesys surgery in younger patients. The improved CDS was thought to correlate with rehydration of the disc [13].
In consideration of performing stabilization or fusion, we made decisions by the degree of degeneration at each level. The choices were dependent on the morphological changes on preoperative MRI. If the target level demonstrated simple herniation with physiological motion, we preferred dynamic stabilization. In contrast, if the target level demonstrated hard disc formation, marked instability (e.g., more or equal to Meyerding grade II spondylolisthesis), limited ROM (<3°), or collapsed disc, we opted to perform fusion for the more degenerated level. The facet joints were preserved without violation at dynamic stabilization levels. In contrast, the facet joints or foramens would be resected more for cage insertions without neural structure injury [15,16,22-26].
Regarding the issue of adjacent-segment degeneration (ASD), our group previously published a study to address ASD and found that the dynamic stabilization would lead to a lower chance of adjacent disc degeneration in comparison with interbody fusion [27]. The paper concluded that the clinical improvements after Dynesys were similar to those following fusion for L4–5 Meyerding grade I degenerative spondylolisthesis at 3-year postoperation. According to radiological evaluations, there was a lower chance of disc degeneration in the adjacent levels of the patients who had undergone Dynesys dynamic stabilization. However, other radiological signs of ASD, including instability, endplate degeneration, and ROM, were similar between the 2 groups. Although none of the patients in the series required secondary surgery, a longer follow-up and a larger number of patients would be necessary to corroborate the protective effect of Dynesys against ASD. We believe the rate of ASD would be very similar to the previous study. The issue of ASD is beyond our current study and future investigations of larger scale and longer follow-up are needed to address the issue.
The current study demonstrated the safety and effect of the DTO hybrid system. The prevention effect of adjacent segmental disease was still unclear, though the bridged levels showed image evidence of disc rehydration. The impact on adjacent segmental disease needs further study to confirm.
During the follow-up of more than 2 years, the patients with lumbar spondylolisthesis or stenosis had well maintained lordosis after DTO hybrid system, compared to the preoperative period. Patients with spondylolisthesis had worse disability scores than these with stenosis before stabilization. However, both groups had significant improvements and similar results in disability and pain scores after DTO hybrid stabilization and fusion surgery. Further evaluations are needed to evaluate more radiographic differences.
Fig. 1.
All of the patients’ clinical evaluations before and after surgery. (A) JOA scores, (B) ODI scores, (C) VAS for back pain, and (D) VAS for leg pain. All the disability and pain scores improved significantly after surgery. JOA, Japanese Orthopedic Association; ODI, Oswestry Disability Index; VAS, visual analogue score. *p < 0.05, statistically significant difference.

Fig. 2.
The comparison between the spondylolisthesis group and the stenosis group. (A) JOA scores, (B) ODI scores, (C) VAS for back pain, and (D) VAS for leg pain. (A, B) The disability scores were worse in the spondylolisthesis group before surgery. Both groups had significant improvements in the disability and pain scores after surgery. JOA, Japanese Orthopedic Association; ODI, Oswestry Disability Index; VAS, visual analogue score. *p < 0.05, statistically significant difference.
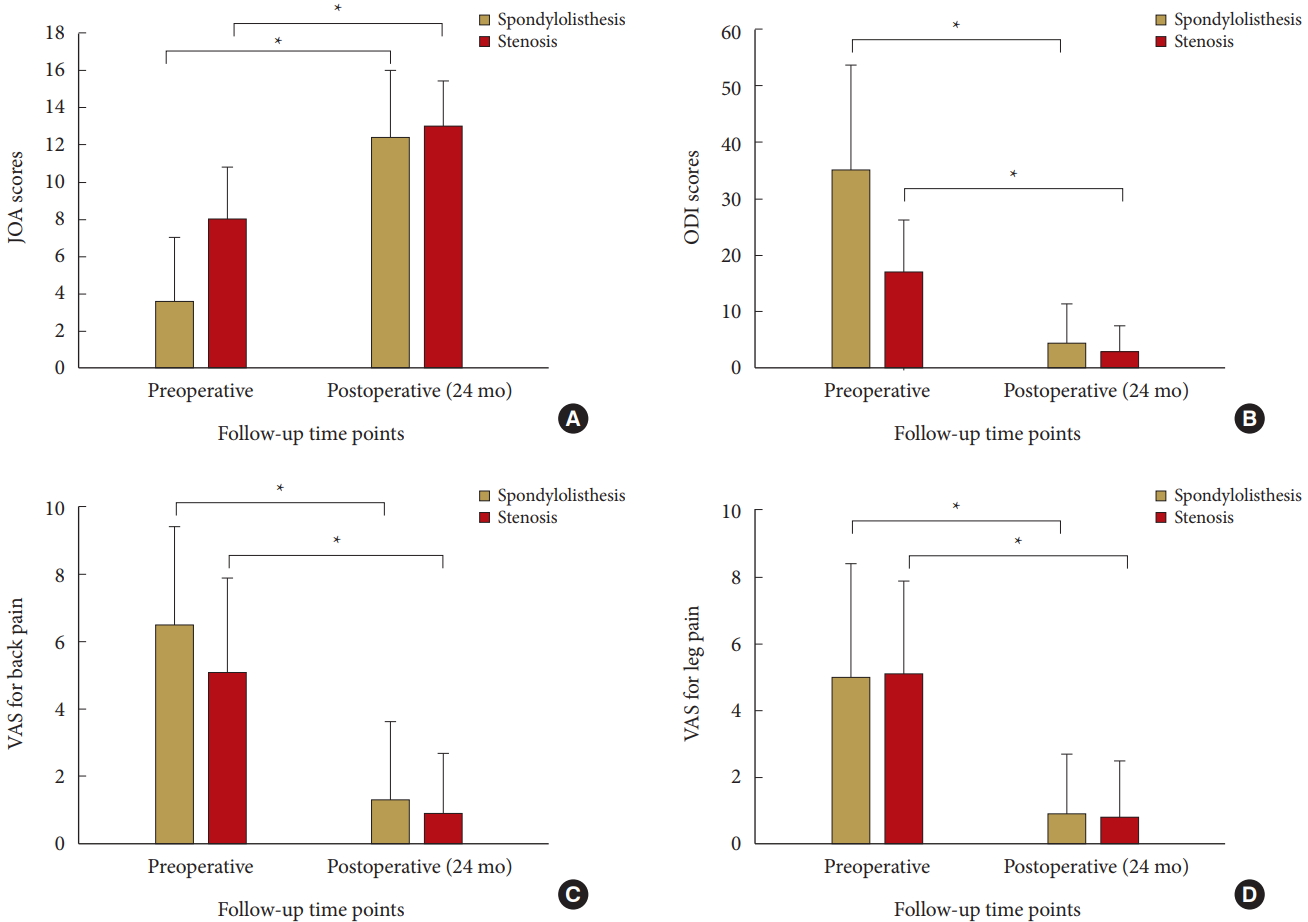
Fig. 3.
The images of a 34-year-old male patient. (A) Preoperative magnetic resonance imaging T2-weighted image sagittal view showed herniated and migration of intervertebral disc at L4–5–S1. (B) Preoperative computed tomography scan sagittal reconstruction view showed bilateral spondylolysis at L5–S1. Arrowhead: Spondylolysis. Arrow: normal pars interarticularis. Preoperative (C) and postoperative (D) radiographies demonstrated well-maintained lumbar lordosis.
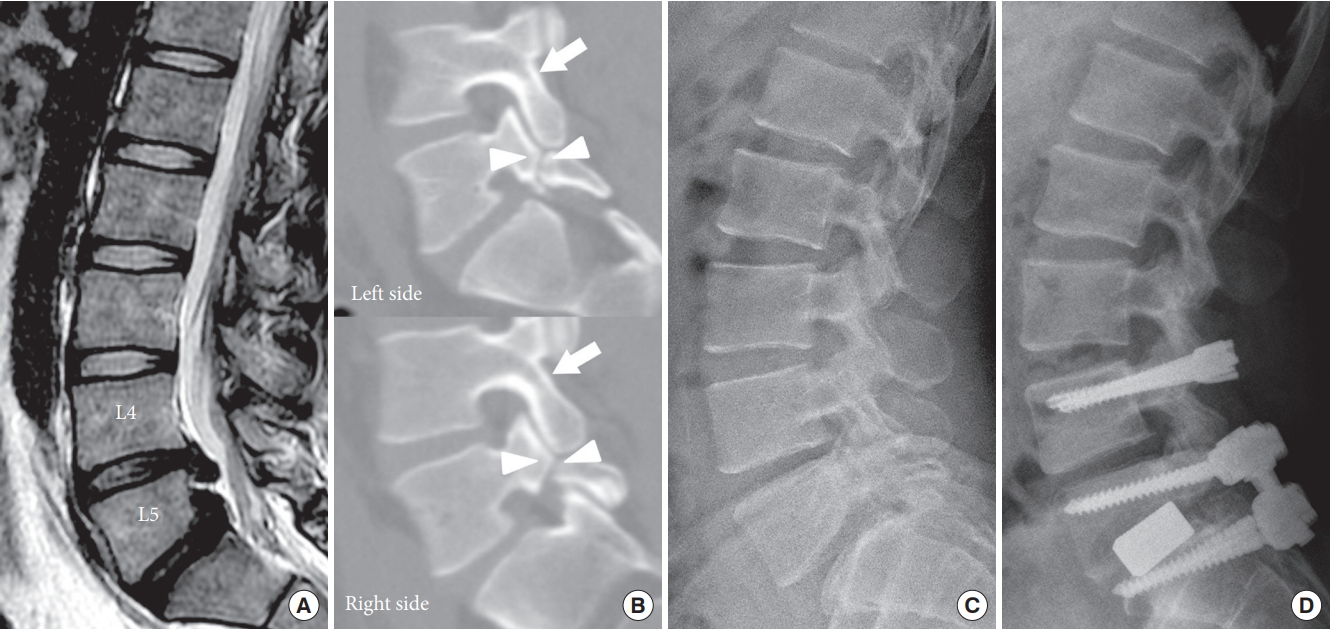
Fig. 4.
The images of a 66-year-old female patient. (A) Preoperative magnetic resonance imaging T2-weighted image sagittal view showed herniated and migration of intervertebral disc at L1–2–3–4. Spondylolisthesis was noted at L3–4. Preoperative (B) and postoperative (C) radiographies demonstrated well-maintained lumbar lordosis.
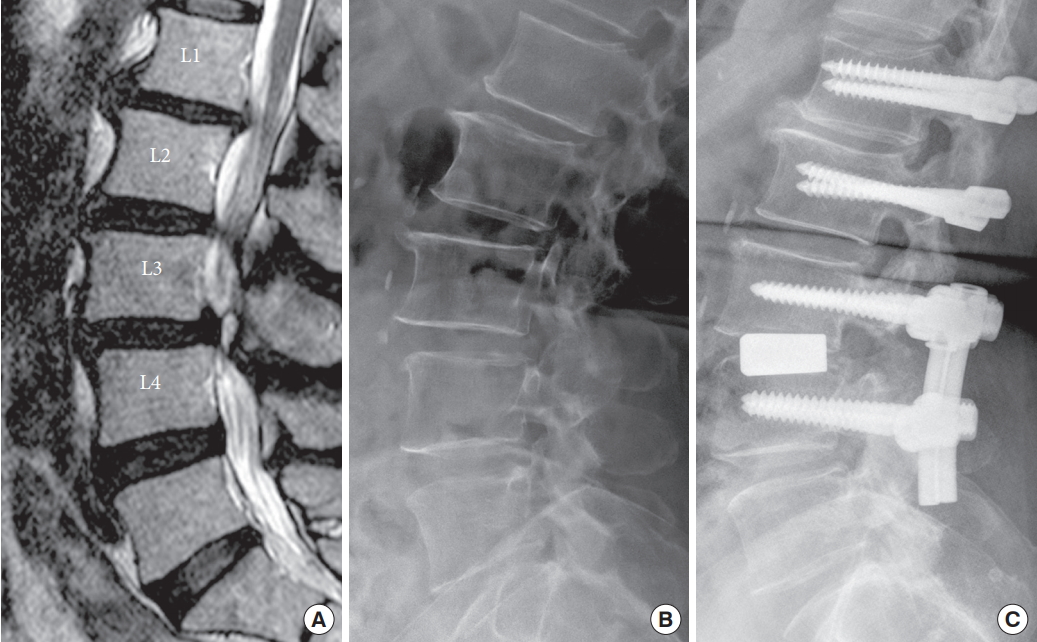
Fig. 5.
The pre- and postoperative X-rays of the 66-year-old female patient. (A, B) Preoperative flexion and extension. (C, D) Postoperative flexion and extension. The while lines represent the Cobb angle of the index levels. The range of motion (ROM) is the difference of Cobb angles in flexion and extension. The preoperative ROM of L1–2–3 is 14°. The postoperative ROM of that is 4°.
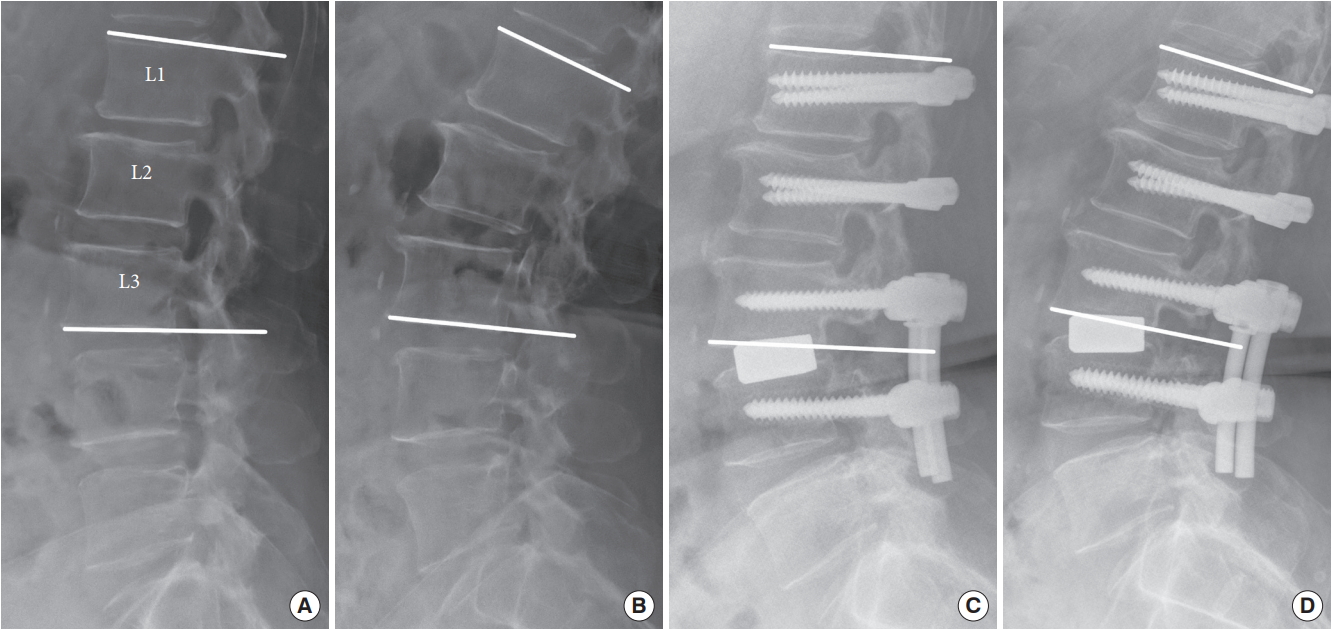
Fig. 6.
The pre- and postoperative magnetic resonance imagings (MRIs) of the 66-year-old female patient. (A) Preoperative sagittal T2-weighted image (T2WI). (B) Two-year postoperative sagittal T2WI. The postoperative MRI demonstrate good decompression and alignment of the lumbar spine. Arrow: regression of herniated disc at L1–2. Diamond: rehydration and increased signal intensity of bridged disc at L2–3. Double arrows: the reduced and well-maintained alignment at L3–4.
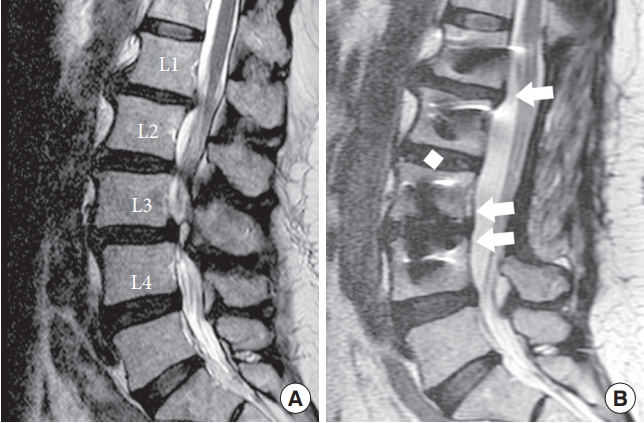
Table 1.
Clinical and demographic characteristics (n=30)
Table 2.
Distribution of operation levels
| Disc level | Value |
|---|---|
| Two disc levels | 15 |
| L3–4–5 | 10 (66.7) |
| L4–5–S1 | 5 (33.3) |
| Three disc levels | 10 |
| L1–2–3–4 | 1 (10.0) |
| L2–3–4–5 | 2 (20.0) |
| L3–4–5–S1 | 7 (70.0) |
| Four disc levels | 5 |
| L2–3–4–5–S1 | 5 (100) |
Table 3.
Comparison between spondylolisthesis and disc disease
| Characteristic | Overall | Spondylolisthesis | Stenosis or herniated disc | p-value |
|---|---|---|---|---|
| Age (yr) | 61.9 ± 12.9 | 63.9 ± 11.6 | 57.4 ± 15.4 | 0.280 |
| Smoking | 3 | 3 | 0 | 0.328 |
| Diabetes mellitus | 11 | 7 | 4 | 0.429 |
| Hypertension | 16 | 12 | 4 | 0.404 |
| Osteoporosis | 10 | 7 | 3 | 0.656 |
| Operation disc levels | 2.7 ± 0.8 | 2.7 ± 0.8 | 2.6 ± 0.5 | 0.539 |
| Sex | 0.018* | |||
| Male | 13 | 6 | 7 | |
| Female | 17 | 15 | 2 | |
| JOA | ||||
| Preoperative | 5.6 ± 3.9 | 3.6 ± 3.4 | 8.0 ± 2.8 | 0.011* |
| Postoperative (24 mo) | 13.6 ± 1.7 | 12.4 ± 3.6 | 13.0 ± 2.4 | 0.631 |
| ODI | ||||
| Preoperative | 21.2 ± 9.8 | 35.1 ± 18.5 | 17.0 ± 9.3 | 0.019* |
| Postoperative (24 mo) | 2.7 ± 3.9 | 4.4 ± 6.9 | 2.9 ± 4.5 | 0.547 |
| VAS back pain | ||||
| Preoperative | 5.7 ± 3.1 | 6.5 ± 2.9 | 5.1 ± 2.8 | 0.350 |
| Postoperative (24 mo) | 0.4 ± 1.1 | 1.3 ± 2.3 | 0.9 ± 1.8 | 0.686 |
| VAS leg pain | ||||
| Preoperative | 5.0 ± 3.1 | 5.0 ± 3.4 | 5.1 ± 2.8 | 0.900 |
| Postoperative (24 mo) | 0.9 ± 1.7 | 0.9 ± 1.8 | 0.8 ± 1.7 | 0.928 |
REFERENCES
1. Bassewitz H, Herkowitz H. Lumbar stenosis with spondylolisthesis: current concepts of surgical treatment. Clin Orthop Relat Res 2001 54-60.

2. Bridwell KH, Sedgewick TA, O’Brien MF, et al. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord 1993 6:461-72.


3. Glassman SD, Carreon LY, Djurasovic M, et al. Lumbar fusion outcomes stratified by specific diagnostic indication. Spine J 2009 9:13-21.


4. Vaccaro AR, Garfin SR. Internal fixation (pedicle screw fixation) for fusions of the lumbar spine. Spine (Phila Pa 1976) 1995 20(24 Suppl):157S-65S.


5. Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am 2009 91:1295-304.



6. Maeda T, Buchowski JM, Kim YJ, et al. Long adult spinal deformity fusion to the sacrum using rhBMP-2 versus autogenous iliac crest bone graft. Spine (Phila Pa 1976) 2009 34:2205-12.


7. Mannion RJ, Nowitzke AM, Wood MJ. Promoting fusion in minimally invasive lumbar interbody stabilization with lowdose bone morphogenic protein-2--but what is the cost? Spine J 2011 11:527-33.


8. Banwart JC, Asher MA, Hassanein RS. Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine (Phila Pa 1976) 1995 20:1055-60.


9. Fischgrund JS. The argument for instrumented decompressive posterolateral fusion for patients with degenerative spondylolisthesis and spinal stenosis. Spine (Phila Pa 1976) 2004 29:173-4.


10. Fritzell P, Hägg O, Nordwall A. Complications in lumbar fusion surgery for chronic low back pain: comparison of three surgical techniques used in a prospective randomized study. A report from the Swedish Lumbar Spine Study Group. Eur Spine J 2003 12:178-89.



11. Rahm MD, Hall BB. Adjacent-segment degeneration after lumbar fusion with instrumentation: a retrospective study. J Spinal Disord 1996 9:392-400.


12. Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine: a multi-center study of a novel non-fusion system. Eur Spine J 2002 11 Suppl 2:S170-8.


13. Fay LY, Wu JC, Tsai TY, et al. Intervertebral disc rehydration after lumbar dynamic stabilization: magnetic resonance image evaluation with a mean followup of four years. Adv Orthop 2013 2013:437570.




14. Fay LY, Wu JC, Tsai TY, et al. Dynamic stabilization for degenerative spondylolisthesis: evaluation of radiographic and clinical outcomes. Clin Neurol Neurosurg 2013 115:535-41.


15. Ko CC, Tsai HW, Huang WC, et al. Screw loosening in the Dynesys stabilization system: radiographic evidence and effect on outcomes. Neurosurg Focus 2010 28:E10.


16. Wu JC, Huang WC, Tsai HW, et al. Pedicle screw loosening in dynamic stabilization: incidence, risk, and outcome in 126 patients. Neurosurg Focus 2011 31:E9.

17. Schaeren S, Broger I, Jeanneret B. Minimum four-year follow-up of spinal stenosis with degenerative spondylolisthesis treated with decompression and dynamic stabilization. Spine (Phila Pa 1976) 2008 33:E636-42.


18. Schnake KJ, Schaeren S, Jeanneret B. Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine (Phila Pa 1976) 2006 31:442-9.


19. Maserati MB, Tormenti MJ, Panczykowski DM, et al. The use of a hybrid dynamic stabilization and fusion system in the lumbar spine: preliminary experience. Neurosurg Focus 2010 28:E2.

20. Lee SE, Jahng TA, Kim HJ. Hybrid surgery combined with Dynamic stabilization system and fusion for the multilevel degenerative disease of the lumbosacral spine. Int J Spine Surg 2015 9:45.



21. Kashkoush A, Agarwal N, Paschel E, et al. Evaluation of a hybrid dynamic stabilization and fusion system in the lumbar spine: a 10 year experience. Cureus 2016 8:e637.



22. Fay LY, Chang PY, Wu JC, et al. Dynesys dynamic stabilization-related facet arthrodesis. Neurosurg Focus 2016 40:E4.

23. Cheng YW, Chang PY, Wu JC, et al. Letter to the Editor: Pedicle screw-based dynamic stabilization and adjacent-segment disease. J Neurosurg Spine 2017 26:405-6.


24. Kuo CH, Chang PY, Tu TH, et al. The effect of lumbar lordosis on screw loosening in Dynesys dynamic stabilization: four-year follow-up with computed tomography. Biomed Res Int 2015 2015:152435.




25. Kuo CH, Chang PY, Wu JC, et al. Dynamic stabilization for L4-5 spondylolisthesis: comparison with minimally invasive transforaminal lumbar interbody fusion with more than 2 years of follow-up. Neurosurg Focus 2016 40:E3.

26. Yeh MY, Kuo CH, Wu JC, et al. Changes of facet joints after dynamic stabilization: continuous degeneration or slow fusion? World Neurosurg 2018 113:e45-50.


27. Kuo CH, Huang WC, Wu JC, et al. Radiological adjacentsegment degeneration in L4-5 spondylolisthesis: comparison between dynamic stabilization and minimally invasive transforaminal lumbar interbody fusion. J Neurosurg Spine 2018 Jun;1:1. -9. [Epub]. https://doi.org/10.3171/2018.1.SPINE17993.


- TOOLS



























