Incidence of Chronic Periscapular Pain After Adult Thoracolumbar Deformity Correction and Impact on Outcomes
Article information
Abstract
Objective
Extension of the posterior upper-most instrumented vertebra (UIV) into the upper thoracic (UT) spine allows for greater deformity correction and reduced incidence of proximal junction kyphosis (PJK) in adult spinal deformity (ASD) patients. However, it may be associated with chronic postoperative scapular pain (POSP). The goal of this study was to assess the relationship between UT UIV and persistent POSP, describe the pain, and assess its impact on patient disability.
Methods
ASD patients who underwent multilevel posterior fusion were retrospectively identified then administered a survey regarding scapular pain and the Oswestry Disability Index (ODI), by telephone. Univariate and multivariate analysis were utilized.
Results
A total of 74 ASD patients were included in the study: 37 patients with chronic POSP and 37 without scapular pain. The mean age was 70.5 years, and 63.9% were women. There were no significant differences in clinical characteristics, including mechanical complications (PJK, pseudarthrosis, and rod fracture) or reoperation between groups. Patients with persistent POSP were more likely to have a UT than a lower thoracic UIV (p=0.018). UT UIV was independently associated with chronic POSP on multivariate analysis (p=0.022). ODI score was significantly higher in patients with scapular pain (p=0.001). Chronic POSP (p=0.001) and prior spine surgery (p=0.037) were independently associated with ODI on multivariate analysis.
Conclusion
A UT UIV is independently associated with increased odds of chronic POSP, and this pain is associated with significant increases in patient disability. It is a significant clinical problem despite solid radiographic fusion and the absence of PJK.
INTRODUCTION
Up to one-third of the general population [1-3], including 68% of the population over the age of 60, is affected by adult spinal deformity (ASD) [4]. ASD can cause severe back and leg pain as well as neurologic deficits as a result of compression of the neural elements [5]. This symptomology can lead to significant disability and declines in health-related quality of life (HRQoL) measures; deformity severity, as measured by radiographic spinal alignment measures, is directly related to worse disability [6-13]. Surgery plays an important role in the management of ASD patients that fail conservative therapy. Surgical correction of sagittal and spinopelvic malalignment can result in significant decreases in pain and disability and improved appearance [13-16].
The correction of thoracolumbar ASD frequently requires the use of long constructs from the sacrum or ilium to the thoracic spine in order to adequately correct spinal deformity. Where to place the upper-most instrumented vertebrae (UIV) of a construct is influenced by a variety of factors, including the degree of correction required, magnitude of thoracic kyphosis, bone quality, and location of the deformity [17,18]. UIV placement in the upper thoracic (UT) spine (T1–6) has been associated with an increased degree of correction and reduced rates of proximal junctional kyphosis (PJK) relative to those in the lower thoracic (LT) spine (T7–12) [18,19]. However, UT UIVs are also associated with longer operative times and increased operative blood loss [17,18]. Long-term HRQoL measures are not significantly different in patients with UIVs in the UT vs. those in the LT [18]. Anecdotally, however, many patients with UT UIV complain of chronic scapular pain following surgery.
Numerous studies have described persistent local axial pain following posterior cervical spine surgery, including incidence, predictors, impact on quality of life, and preventative measures [20-25]. Nevertheless, there is a paucity of similar research investigating scapular pain following placement of a UIV in the UT spine, despite the commonality of this pain in the clinic. Sakaura et al. [26] investigated the relationship of thoracic spine surgery and persistent local pain in 29 patients, and suggested the pain may result from dissection of muscle insertions at the cervicothoracic junction. Therefore, the goal of this study was to formally describe the potential relationship between UIV in the UT spine and development of chronic scapular pain, when accounting for other potential confounders, as well as the impact of this pain on self-reported Oswestry Disability Index (ODI) scores. The characteristics of the pain, how it limits patients, and pain-specific treatment methods are also described.
MATERIALS AND METHODS
1. Patient Population
ASD patients over the age of 18 who underwent a multilevel posterior fusion of either 7–12 segments or greater than 13 segments were retrospectively identified from 2012 to 2019 using the electronic medical record. This study was formally approved by the Institutional Review Board of University of California, San Francisco (No. 18-26789). Exclusion criteria included constructs that were extended into the cervical spine and patient self-reported construct extensions at outside institutions. Patients were initially grouped based on the location of the UIV (UT vs. LT). UT levels were defined as T1–6. LT levels were defined as T7–12. All patients had constructs ending in the lumbar spine or pelvis.
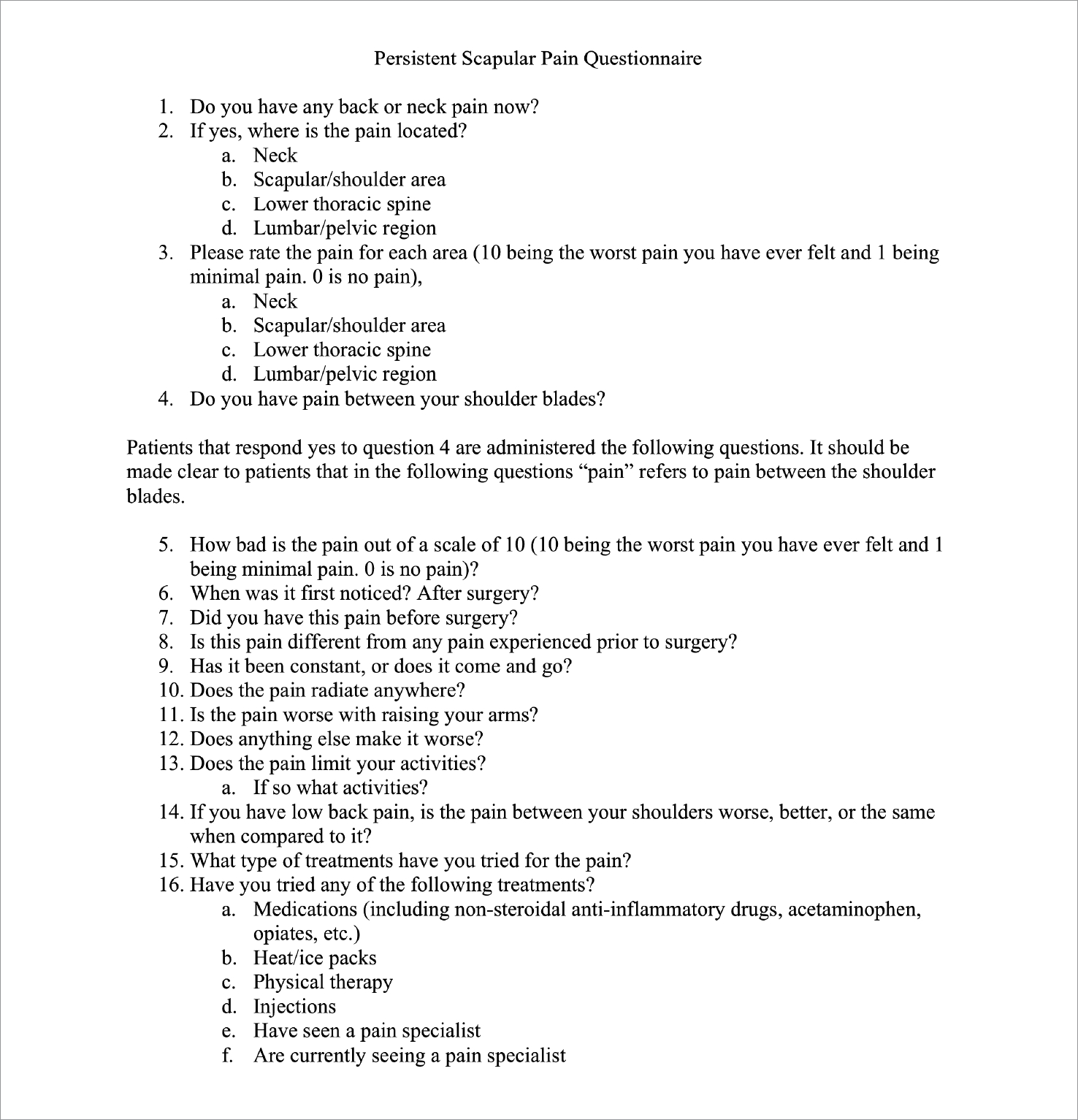
2. Clinical Data
Patient demographics, surgical characteristics, and clinical outcomes were retrospectively collected and reviewed, including age, sex, history of prior spinal surgery, surgical indication, UIV, lower-most instrumented vertebrae, the need for reoperation, and mechanical complications such as PJK, pseudarthrosis, and rod fracture. Patients were subsequently administered a standard telephone survey regarding scapular pain (Fig. 1), as well as the ODI [27]. Verbal consent was obtained for each patient prior to administering the surveys. The scapular pain survey (Fig. 1) administered to patients assessed the presence and characteristics of persistent scapular pain, including the time of onset, pain score, the timing of pain, pain radiation, aggravators, limitations caused by the pain, and treatments attempted. Survey administrators were not blinded to the clinical characteristics of patients, but all patients were administered standard questions read from the survey in Fig. 1.
The primary outcomes of interest were the presence of chronic postoperative scapular pain, disability, and a description of the scapular pain in patients with chronic postoperative scapular pain. Chronic postoperative scapular pain was defined as scapular pain that was not present prior to surgery or was significantly different from any preoperative pain. Disability was measured using an ODI survey administered over the phone. Descriptions of the scapular pain were collected using a standardized predetermined telephone survey.
3. Statistical Analysis
Chi-square test and Student t-test were used for categorical and continuous outcomes, respectively. A multivariate backward likelihood binary logistic regression model was used to further elucidate variables independently associated with chronic scapular pain, including UIV location. Variables initially included in the model included: patient age, UIV location, patient sex, history of prior spine surgery, rod fracture, pseudarthrosis, and PJK. A multivariate backward likelihood linear regression model was also used to identify variables independently associated with ODI score. Variables initially included in the model included: patient age, persistent scapular pain, patient sex, history of prior spine surgery, rod fracture, pseudarthrosis, and PJK. A p-value of less than 0.05 was used as the threshold of statistical significance. All statistical analysis was performed using IBM SPSS Statistics ver. 26.0 (IBM Co., Armonk, NY, USA).
RESULTS
1. Overall Patient Demographics
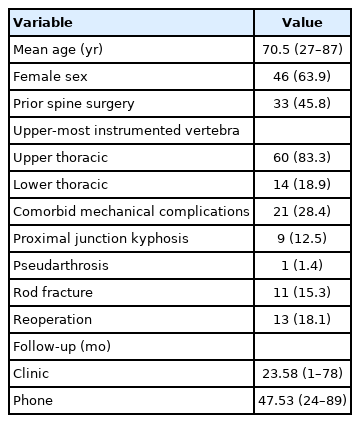
A total of ASD 265 patients were identified for possible inclusion: 173 UT patients and 92 LT patients as a control group. Following the removal of patients who met exclusion criteria, 161 UT patients and 83 LT patients were called. Successful administration of the telephone surveys was accomplished in 60 of 161 (37.2%) and 15 of 83 (18.0%) of UT and LT patients, respectively. One patient was excluded from the LT group following the identification of a previous cervical spine surgery during the phone call (Fig. 2).
Schematic showing the number of patients per group, including patients who were excluded, called, and successfully administered the scapular pain and Oswestry Disability Index surveys. UT, upper thoracic; LT, lower thoracic.
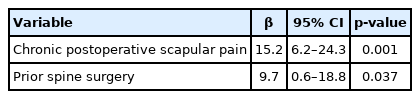
Overall patient demographics and clinical outcomes can be seen in Table 1. A total of 74 patients were included in the study with a minimum follow-up to survey administration of 23 months. The cohort was 63.9% women with an average age of 70.5 years. Almost half of the patients had had prior spine surgery (45.8%). Most patients had a UIV in the UT (83.3% UT vs. 18.9% LT). A minority of patients required a reoperation (18.1%) or had a mechanical complication, including PJK (12.5%), pseudarthrosis (1.4%), rod fracture (15.3%). The average length of follow-up was 22.6 and 47.5 months with regards to clinic and phone follow-ups, respectively. The minimum phone follow-up for all patients was 24 months.
2. Comparison of Patients With and Without Chronic Postoperative Scapular Pain
There were 37 patients in each group (Table 2). There were no significant differences in mean patient age (69.9 years vs. 71.0 years, p=0.689), patient sex (73.0% vs. 54.1%, p=0.091), or history of prior spine surgery (45.9% vs. 45.9%, p=1.000). Similarly, there was no difference in incidence of mechanical complications between the groups (32.4% vs. 21.6%, p=0.295), including PJK (16.2% vs. 8.1%, p=0.479), pseudarthrosis (2.7% vs. 0.0%, p=0.314), and rod fracture (16.2% vs. 13.5%, p=0.744). However, patients with chronic postoperative scapular pain were more likely to have a UT UIV than those without pain (34 of 37 [91.9%] vs. 26 of 37 [74.3%], p=0.018). Only 3 of 14 patients (21.4%) with an LT UIV developed postoperative scapular pain versus 34 of 60 patients (56.7%) with a UT UIV. Patients with scapular pain also had significantly higher ODI scores, indicating more severe disability, that those without scapular pain (41.2% vs. 25.4%, p=0.001) (Fig. 3).
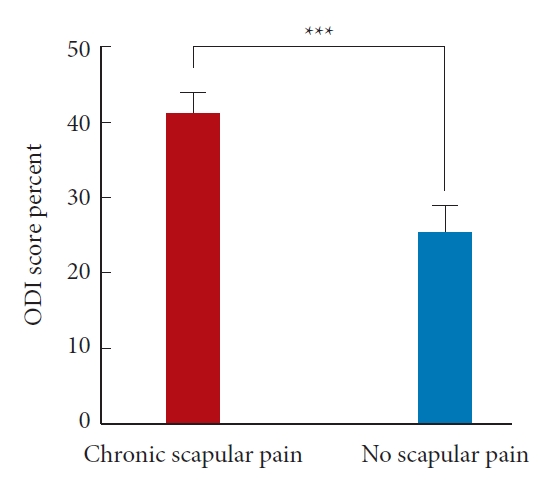
Bar graph highlighting a significantly higher mean Oswestry Disability Index (ODI) score in patients with chronic scapular pain (***p = 0.001).
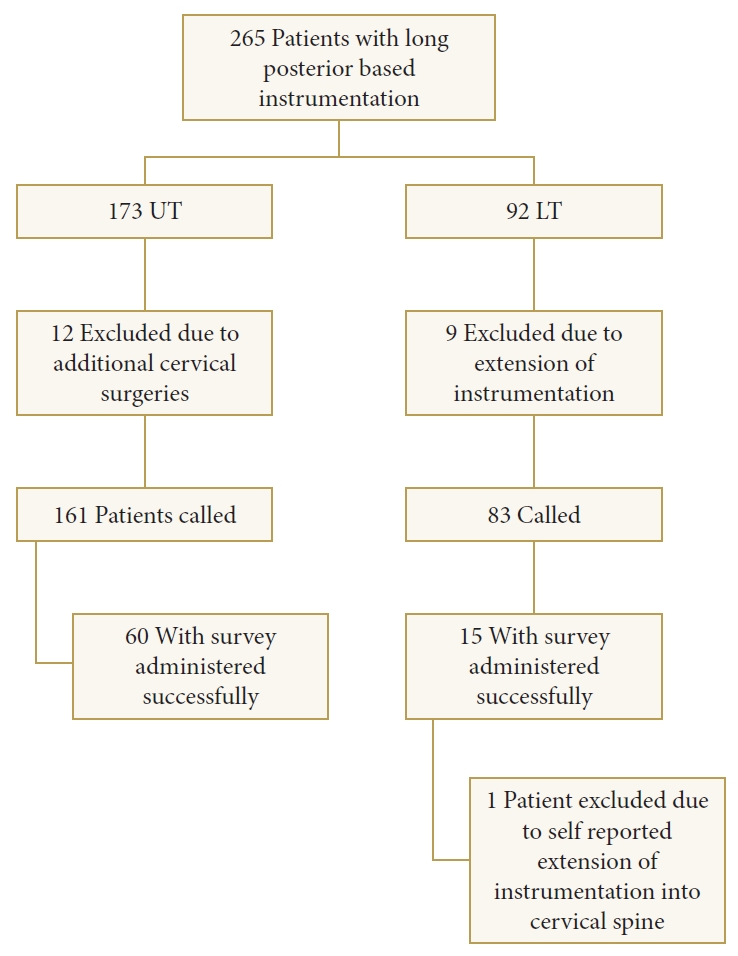
A multivariate logistic regression model demonstrated the significant independent association of UT UIV with the development of chronic postoperative scapular pain (OR, 5.0; 95% confidence interval [CI], 1.3–19.8, p=0.022) (Table 3). A backward likelihood ratio linear regression model showed both chronic postoperative scapular pain (β=15.2%; 95% CI, 6.2–24.3; p=0.001) and prior spine surgery (β=9.7%; 95% CI, 0.6–16.8; p=0.037) to be independently associated with increased ODI scores (Table 4). There was no difference in ODI scores between LT and UT patients (24.5% vs. 35.0%, p=0.105).
3. Description of Chronic Postoperative Scapular Pain
Table 5 presents pain characteristics and treatments attempted in patients who described chronic postoperative scapular pain. The mean pain score associated with the scapular pain was 6.2. The majority of patients first noticed the pain immediately after surgery (83.3%), described it as waxing and waning (73.0%), and stated it was either worse (48.6%) or the same (24.3%) as their low back pain. Almost one-half of the patients (43.4%) described the pain as radiating outside of the scapular region. Common aggravators of the pain included the raising of the arms above the head (45.9%), sitting (16.2%), standing/walking (10.8%), lifting objects (10.8%), or another activity (32.4%). Scapular pain limited the activities of most patients (75.7%). Modalities used by patients to reduce the pain included medication (86.5%), heat/ice (70.3%), physical therapy (78.4%), and epidural steroid injections (32.4%). Most patients had seen a pain specialist for the pain (54.1%), and 11 of 37 (29.7%) were currently seeing a pain specialist at the time of the interview (Table 5).
DISCUSSION
Constructs with extension into the UT spine have been associated with greater amounts of spinal alignment correction and reduced rates of PJK in ASD patients [18,19]. A common postoperative complaint among patients with a UT UIV is the presence of persistent scapular pain. While studies exist investigating persistent local pain following cervical spine surgery [20-25], there is a lack of similar studies investigating chronic scapular pain following the extension of long constructs into the UT spine. Therefore, the present study sought to describe the chronic postoperative scapular pain, assess patient demographics and clinical variables associated with the onset of the pain, and evaluate the impact of the pain on patient disability (ODI scores).
The first goal was to identify patient demographics and clinical characteristics associated with the development of persistent postoperative scapular pain. Previous studies in the cervical spine literature have assessed risk factors for the development of local axial pain following cervical spine surgery. In a systematic review of 33 studies relating to postoperative axial pain after posterior cervical spine surgery, Wang et al. [20] identify many potential risk factors including surgical technique; less invasive surgical techniques and reconstruction of neck musculature appear to be associated with less postoperative axial pain in some studies. However, they conclude that there is a paucity of highquality evidence supporting any particular risk factor, and that further research is needed. The development of chronic postoperative scapular pain in thoracic spine surgery patients has had minimal investigation relative to postoperative pain in cervical patients. Sakaura et al. [26] investigate the relationship of thoracic spine surgery and persistent local pain in 29 patients undergoing posterior-based thoracic spine surgery. They suggest that the pain is caused by dissection of muscle insertions into the cervicothoracic junction, as 5 of 7 patients with muscle dissection into the cervicothoracic junction (C6–T1) developed postoperative pain as compared to 1 of 22 patients with mid-lower thoracic surgeries (T2 and lower). Their study was limited, however, by the heterogeneous population included in the study (20 patients had instrumentation and 9 did not) and the failure to assess other variables associated with the development of persistent pain, such as age and presence of instrumentation on univariate or multivariate analysis. The present study showed a similar trend as Sakaura et al. [26] as patients with a UT UIV were more likely to have postoperative scapular pain on univariate analysis. We also accounted for additional patient demographics and clinical variables with the potential to impact chronic scapular pain, including age, reoperation, and mechanical complications on multivariate analysis, and demonstrated the independent association of UT UIV with the development of postoperative pain. Unlike Sakaura et al. [26], however, all of the patients in the present study had long posterior spinal instrumentation. As a result, it is possible that the scapular pain seen in UT patients is as a result of their spinal instrumentation, which has been demonstrated to elicit back pain in previous studies [28-30]. Anecdotally, it has been observed that some patients demonstrate an improvement in their scapular pain following instrumentation removal. Indeed, the cause of the scapular pain in UT patients is unclear and could have multiple potential etiologies. Additional research is required to fully define the cause of the chronic postoperative scapular pain in UT patients, and whether it is related to muscle dissection, instrumentation, changes in alignment, or another cause. Future studies involving larger patient cohorts and measuring pain outcomes following instrumentation removal are warranted.
After assessing the relationship between UT UIV and persistent postoperative scapular pain, the impact of the pain on patient disability through the ODI was evaluated. Previous literature in the cervical spine has demonstrated a reduction in HRQoL outcomes in patients with persistent axial pain following cervical spine surgery. In a study of 162 postoperative cervical spine patients, Kimura et al. [24] demonstrated significant reductions in multiple HRQoL outcomes, including the Japanese Orthopaedic Association score, the EuroQol 5 Dimension Questionnaire, and the 36-item Short Form Health Survey, in patients with postoperative axial pain following cervical laminoplasty. The results of the present study show a similar impact on quality of life in patients with chronic postoperative scapular pain. In fact, the majority of patients described their scapular pain as significantly limiting their daily activities (Table 5). In addition, there was a significant increase in ODI score, a validated measure of patient disability that can be reliably administered over the phone [27], in patients with chronic postoperative scapular pain relative to those without (Table 2), indicating worse disability. On multivariate analysis, persistent postoperative scapular pain, as well as prior spine surgery were independently associated with increases in ODI (Table 4). This corresponds with the findings of Kimura et al. [23] regarding axial pain following cervical spine surgery. To our knowledge, no previous studies have evaluated the relationship between postoperative scapular pain following UT spine surgery and ODI score outcome. The findings demonstrate the significant impact of chronic interscapular pain on patient disability and highlight the need for better prevention and treatment methods.
Given the paucity of literature surrounding postoperative scapular pain following UT spine surgery, no previous studies have evaluated potential treatment strategies. In the current study, patients with postoperative scapular pain described a variety of treatment strategies, including medications, heat/ice, physical therapy, epidural injections, and seeing a pain specialist (Table 5); these treatments align with common treatments for back pain [31]. While the response to specific treatments was not specifically evaluated, the continued pain and increased ODI in the patients with scapular pain suggest that the modalities attempted by patients provided limited benefit. Given the potential contribution of the instrumentation itself to the development of postoperative scapular pain, its removal could be another potential treatment in some cases. As previously mentioned, there is anecdotal evidence of reduced scapular pain following instrumentation removal. While studies evaluating implant removal following spine surgery for indications, such as thoracolumbar spine fractures, have shown improved patient quality life and demonstrated adequate safety [28-30,32,33], there remains a paucity of literature surrounding instrumentation removal in ASD patients. Available studies, however, suggest it should be approached with significant caution. In a study of 116 patients with long posterior instrumented fusions, Deckey et al. [34] found that 4/14 patients experienced increased pain, loss of sagittal plane correction, and spinal collapse following implant removal despite intraoperative confirmation of solid fusion, highlighting the risk of instrumentation removal in these patients. Studies within adolescent deformity have also demonstrated the risk of deformity progression with instrumentation removal [35,36]. As a result, the possibility of instrumentation removal should be approached with caution, especially in ASD patients. Future studies should fully evaluate the response of postoperative scapular pain to various conservative treatment modalities using validated pain measures. The risks and benefits of implant removal in ASD patients require additional investigation before consideration as a treatment modality outside of severe, debilitating cases.
The limitations of our study mainly relate to its limited sample size, with a total of 74 patients and 37 per group. While there were strongly significant findings despite the relatively small sample size, it is possible that the low number of patients in each group limited our ability to identify more granular differences between them. The use of a telephone survey to collect information also potentially introduces bias, including nonresponse bias. Nonresponse bias could potentially decrease the reported incidence of postoperative scapular pain as these patients may be unsatisfied with their care and unwilling to participate in a telephone survey. However, only 4 patients out of the 244 called refused to participate in the survey; all other nonresponders were unable to be reached due to not answering the telephone or a disconnected phone number. Similarly, patients without a telephone or with limited access to a telephone were unable to participate in our survey, although this would impact both groups equally. All patients were called at least twice to maximize patient responses and reduce nonresponse bias. Similarly, all known phone numbers for a patient were used to, including cell phone, work, and home numbers, to further reduce any potential bias. Previous research on telephone surveys has also indicated that response rate is a poor predictor of bias [37]. A number of political polling methodologies have response rates below 10%, but still provide valuable information on population trends [38]. Other survey-based studies with lower response rates have also been published (20%, 25%, and 31%) in the spine literature [39]. Another limitation of the study is its retrospective design; this may introduce bias for specific survey questions, such as if patients had postoperative pain immediately following surgery, as some patients had surgery over 5 years ago. The present study also lacks information regarding the efficacy of specific treatments for the scapular pain. Finally, cervical pathology may also impact the findings of this study. However, we attempted to account for this by: (1) specifically asking patients about pain between the shoulder blades, which we believe is less likely to be related to the cervical spine, (2) excluding patients with additional surgeries in the cervical spine (self-reported or noted in the medical record). A large prospectively collected study to assess postoperative scapular pain at interval time points, as well as the efficacy of treatments, would help to eliminate these many of these limitations and is warranted. This would allow for the monitoring of the pain over time and additional insight into the best treatment practices. In addition, while the ODI is a validated HRQoL measure that has been validated for telephone use in spinal deformity patients [27], the scapular pain questionnaire utilized was unvalidated. Thus, the development of a validated measure of scapular pain may also aid in future research into this topic. Studies into the prevention of postoperative scapular pain are also needed. As minimally invasive spine surgery (MIS) limits muscle dissection, the incidence of postoperative scapular pain in patients with UT UIV who underwent MIS surgery [40] may provide additional insight into the contribution of muscle dissection in the development of the pain.
Nevertheless, the present study is the only one, to our knowledge, to evaluate the relationship between UT UIV and the development of chronic scapular pain in a homogenous population of ASD patients with long posterior constructs, while accounting for reoperations and mechanical complications. In addition, we provide a detailed description of the pain and highlight its significant impact on patient activities and disability. Therefore, we believe persistent postoperative scapular pain is a significant long-term complication of instrumentation extending into the UT spine and requires additional investigation into the incidence, treatment, and prevention. We hope that this study aids with patient counseling regarding postoperative scapular pain following the placement of an UT UIV and also spurs additional investigation into this important clinical phenomenon.
CONCLUSION
Posterior instrumentation extending into the UT spine is independently associated with the development of persistent postoperative scapular pain. The resulting scapular pain is subsequently associated with a significant increase in ODI scores, indicating greater disability in these patients. A majority of patients also describe the scapular pain as limiting their activities and the continuation of the pain despite attempting multiple treatment modalities. Despite the limitations associated with a retrospective study, we hope these findings will aid with preoperative discussions with patients and prompt additional research into postoperative scapular pain in ASD patients with UT UIVs. Larger, prospective studies further investigating the incidence, risk factors, and potential treatments of postoperative scapular pain in patients with UT spine instrumentation are needed. These studies will allow for improved future counseling and treatment of patients with posterior-based instrumentation extending into the UT spine.
Notes
The authors have nothing to disclose.