Effectiveness of the Endplate Reduction Technique Combined With Bone Grafting for the Treatment of Thoracolumbar Fractures by Using Posterior Short-Segment Fixation
Article information
Abstract
Objective
This study aimed to examine the effect of the endplate reduction (EPR) technique combined with bone grafting for treating thoracolumbar burst fractures using posterior short-segmental fixation.
Methods
Patients with thoracolumbar fractures admitted between January 2018 and October 2021 were retrospectively analyzed, and those meeting the criteria were assigned to the EPR group and the intermediate screws (IS) group. The vertebral wedge angle (VWA), Cobb angle (CA), anterior vertebral body height (AVBH), middle vertebral body height (MVBH), upper endplate line (UEPL), upper intervertebral angle (UIVA), and upper intervertebral disc height (UIDH) indices were examined and compared preoperatively, first day postoperatively, as well as at 12 months postoperatively.
Results
The result indicated that the EPR group achieved better MVBH reduction (p<0.001), UEPL reduction (p<0.001), vertebral body fracture healing (p=0.006), as well as implant breakage (p=0.04) than the IS group; VWA (p<0.001), CA (p=0.005), AVBH (p<0.001), MVBH (p<0.001), UEPL (p<0.001), and UIDH (p<0.001) were lost after reduction less than those in the IS group. There was no significant difference in operative time (p=0.315) and intraoperative bleeding (p=0.274) between the 2 groups.
Conclusion
The EPR group achieved better results in repositioning and maintaining MVBH and endplate morphology, with less correction loss after the reduction of the VWA, CA, AVBH, and endplate morphology. The EPR group exhibited a better healing pattern after vertebral fracture and disc degeneration was better relieved.
INTRODUCTION
Fractures of the thoracolumbar are more common in spinal trauma for their structural characteristics [1]. Treatment options for unstable thoracolumbar fractures without neurological damage have been controversial [2]. Some scholars have suggested that conservative treatment can be cost-effective and provide effective long-term results, whereas it can leave a legacy of deformity. As research has been leaping forward, increasing scholars have suggested that surgery is capable of correcting the deformity and achieving a better long-term outcome, thus revealing that unstable thoracolumbar fractures should be treated surgically.
There have been many surgical approaches to the thoracolumbar, with options for anterior fixation, posterior fixation, or combined anterior and posterior fixation [3-5]. Anterior fixation is relatively more damaging and bleeds more, with a loss of some mobility [6]. Posterior fixation, on the other hand, is less invasive, and simple, and is widely used in clinical practice. Posterior fixation is divided into single-segment fixation, short-segment fixation, and long-segment fixation [7]. Short-segment fixation is simple, less invasive, and more reliable [8-10]. However, since the anterior column of the thoracolumbar instability fracture is severely damaged, the use of short-segment fixation causes concentrated stress, thus easily resulting in failure of reduction and implant breakage, resulting in surgical failure. Furthermore, the posterior short-segment fixation technique refers to an indirect repositioning technique that does not effectively restore the height of the anterior column of the vertebral body due to poor repositioning of the central endplate collapse. To reduce the failure rate of surgery and effectively restore the collapse of the central endplate [11], the methods currently applied comprise the placement of pedicle screws in the injured vertebral body or posterior vertebral body kyphoplasty in the injured vertebral body to reduce the stress concentration and restore the injured vertebral body, thus reducing the failure rate of surgery [12-14].
This study suggests that good reduction, effective support, and early healing of vertebral fractures are the keys to the successful treatment of short-segment thoracolumbar fractures. By repositioning the endplate and disc as a whole, the endplate can effectively restore the normal space of the disc and reduce further disc degeneration, while effectively repositioning the vertebral body to facilitate the maintenance of fracture repositioning and correction of the kyphosis deformity and reduce the occurrence of recurrent kyphosis deformity. Based on the above concept, direct prying of the repositioned endplate was proposed to restore normal disc and vertebral body height, followed by implantation of allograft bone via the pedicle to fill the repositioned cavity to maintain the repositioning and promote fracture healing.
MATERIALS AND METHODS
1. Patient Population
We conducted a retrospective analysis of patients admitted with thoracolumbar fractures between January 2018 and October 2021. This study was approved by the ethics committee of Hebei Medical University (2018206314). Informed consent was obtained from all individual participants included in the study. Inclusion criteria were as follows: (1) type A3,4 and B1 single-segment thoracolumbar (T11-L2) burst fracture according to AO classification, with fracture involving only the upper endplate or involving the lower endplate without displacement; (2) aged 18–60 years; (3) no symptoms of neurological injury; (4) posterior short-segment fixation using endplate prying and repositioning combined with bone grafting techniques or fixation using intermediate screws (IS) in the injured vertebra; (5) follow-up of not less than 1 year. Exclusion criteria: (1) patients with osteoporosis; (2) multiple vertebral fractures; (3) pathological fractures; (4) history of lumbar spine surgery; (5) removal of internal fixation within 1 year. The collected patients were divided into an endplate reduction (EPR) group and an IS group according to the numerical randomization method.
Patients were assigned to types A and B in accordance with AO fracture classification [15], as well as to type I, type II, and type III based on endplate injury classification [16]. Patients are classified as type I, II, III, and IV, which type I and II are considered well healed, and type III and IV were considered poorly healed [17]. A load-sharing classification (LSC) score was performed following the extent of vertebral injury, displacement of fracture fragments, and correction of kyphosis as observed on computed tomography (CT) [18]. Implant breakage was recorded.
2. Surgical Technique
General anesthesia was routinely used. The patient was placed prone on the operating table with the chest and pelvis elevated. The paravertebral muscles were dissected on both sides of the spinous process to expose the fractured vertebral body and the small articular joints adjacent to the superior and inferior vertebral bodies. The Universal Spine System from synthes was adopted to fix the fracture, and 4 Schanz screws were placed in the adjacent superior and inferior vertebral bodies at the fractured segment. The above steps were the same for both groups.
1) EPR group
The emphasis was placed on endplate repositioning and the fractured vertebral endplate is repositioned directly by prying, restoring vertebral height and disc space, and implanting allograft bone to maintain repositioning and facilitating fracture healing. After the same steps were completed, the connecting rod was fitted, the ipsilateral screw was held open using a spreader and the Schanz screw was adjusted in position to indirectly reposition the fractured vertebral body by ligamentous distraction. After satisfactory repositioning, the connecting rod and screw were locked, and the screw was cut to fit. The small articular joints of the fractured vertebra were exposed on both sides of the fractured vertebra, and a fluoroscopically guided pedicle opener (4 mm) was placed at the lowest point of endplate collapse on the vertebral body to pry and reposition the collapsed endplate, followed by screwing in the Schanz screw (6.2 mm) via the pedicle to further pry and reposition. Alternating prying was performed on both sides till the collapsed endplate was satisfactorily repositioned, and the Schanz screw was removed. In the process of prying and repositioning the end plate, attention should be paid to gentle movements, avoiding violent prying and repositioning, and the reduction process should be completed under the supervision of the x-ray fluoroscopy. The prying tool should be no less than 5 mm away from the lowest point of the prying and repositioning to reduce further damage to the end plate. A bone graft funnel was placed through the screw channel, and allograft bone was inserted to fill in the bone defect formed after prying. The anterior aspect of the implant funnel is placed at the posterior edge of the middle third of the vertebral body to reduce the risk of intrusion of the implant material into the spinal canal (Figs. 1, 2).
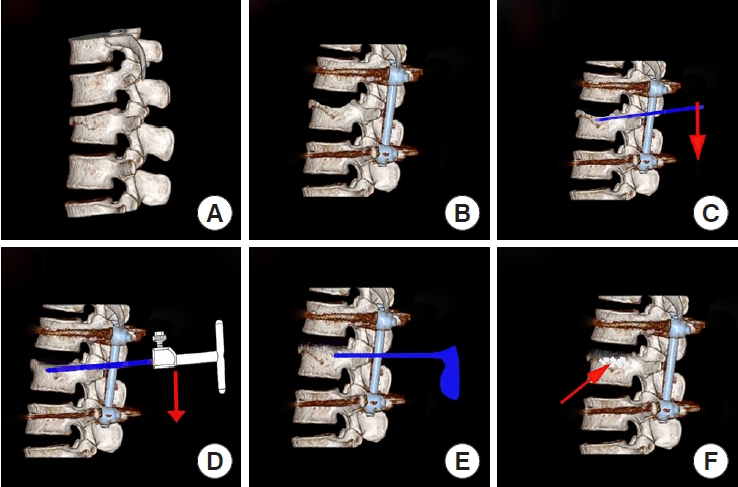
Endplate repositioning and bone grafting procedure. (A) Model of L2 vertebral fracture. (B) Poor recovery of middle vertebral height after ligamentous retraction, poor morphology of the upper endplate. (C) Prying and repositioning of the endplate under fluoroscopy with an opener via the pedicle. (D) Further prying and repositioning of the endplate with Schanz screws. (E) Placement of a bone graft funnel. (F) Placement of allograft bone.
2) IS group
Endplate repositioning was completed through screws placed in the fractured vertebral body, without bone grafting. After completing the same surgical procedure, 2 screws 5 mm shorter than the adjacent fractured vertebral screw were inserted through the pedicle into the fractured vertebral body. After the fitting of the connecting rod, distraction repositioning was performed between the adjacent screws on the ipsilateral side. When the repositioning was satisfactory, the connecting rod and screws were locked, and then the screws were cut to fit [12].
3. Postoperative Management
Antibiotics were administered according to the principles, the wound drain was removed 48 hours after surgery, the wound was changed every 3 days, the stitches were removed 14 days after surgery and a thoracolumbar brace was required for 2 months after surgery.
4. Radiological Evaluation
Preoperative and first postoperative day lumbar anteroposterior and lateral views, lumbar CT, and lumbar magnetic resonance imaging were taken in all patients. Monthly outpatient follow-ups were performed for 3 months after surgery, with the respective lumbar anteroposterior and lateral radiographs being taken. After 3 months postoperatively, the lumbar spine was reviewed every 3 months, with anteroposterior and lateral lumbar spine views taken as required. At the 12-month postoperative review, anteroposterior and lateral spine views and CT of the lumbar spine were taken in preparation to remove the internal fixation. The vertebral wedge angle (VWA), Cobb angle (CA), anterior vertebral body height (AVBH), middle vertebral body height (MVBH), upper endplate line (UEPL) of the fractured vertebra, upper intervertebral angle (UIVA), upper Intervertebral disc height (UIDH), and loss of postoperative correction were examined preoperatively, on the first postoperative day, and at 12 months postoperatively, respectively. The VWA refers to the angle formed by the line of the upper and lower endplates of the fractured vertebral body. The CA measurement is based on the line between the upper endplate of the upper vertebral body of the fractured vertebra and the lower endplate of the lower vertebral body of the fractured vertebra [19]. The AVBH refers to the percentage of the anterior height of the fractured vertebral body to the average of the anterior heights of the upper and lower vertebral bodies of the fractured vertebral body. The MVBH refers to the percentage of the middle height of the fractured vertebral body to the average of the middle height of the upper and lower vertebral bodies of the fractured vertebral body [20]. The UEPL represents is the length of the UEPL of the fractured vertebra as a percentage of the mean length of the UEPLs of the upper and lower vertebrae of the fractured vertebra, thus indicating the morphology of the endplate [21]. The UIVA was the angle between the upper endplate of the fractured vertebra and the lower endplate of the vertebra above the fractured vertebra [22], and the UIDH is the average of the anterior and posterior disc heights above the injured vertebra [23]. Changes in the UIVA and disc height reflected changes in the intervertebral disc space (Fig. 3). Postoperative loss of correction, the difference between the index examined at 12 months postoperatively and the postoperative index, reflected the maintenance of postoperative repositioning. All the above indicators were examined on lateral lumbar radiographs, by a senior radiologist independent of the study, and each set of data was averaged and recorded after 3 measurements.
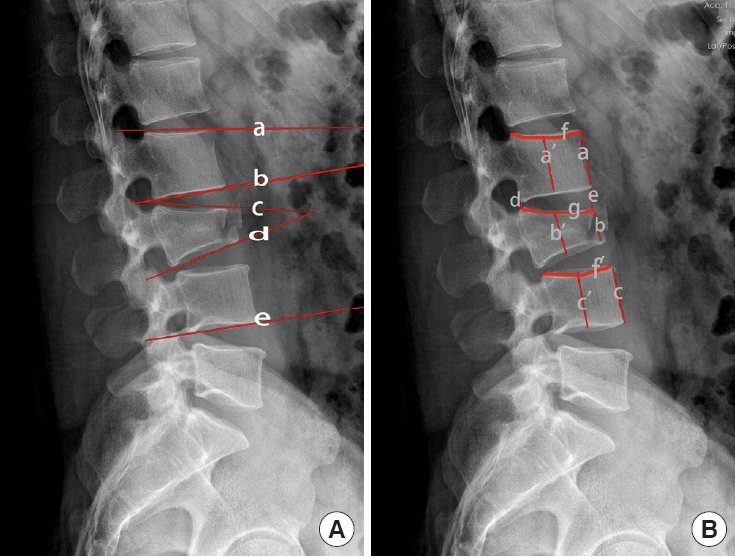
Measurement of radiographic parameters on lateral xray of the lumbar spine. (A) Vertebral wedge angle, the angle formed by the lines c and d; Cobb angle, the angle formed by lines a and e; upper intervertebral angle, the angle formed by the lines b and c. (B) Anterior vertebral body height=2 b/(a+c) ×100%; middle vertebral body height=2 b’/(a’+c’)×100%; upper endplate line=2 g/(f+f ’)×100%; upper intervertebral disc height=(d+e)/2.
5. Statistical Analysis
Data processing was performed using IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA). Data were expressed as mean± standard deviation using the 2 independent samples ttest for normally distributed continuous variables and the MannWhitney U-test for those that did not conform to a normal distribution. The Pearson chi-square test and Fisher exact test were used for categorical data. Probability values less than 0.05 indicate statistically significant differences.
RESULTS
1. General Information
A total of 63 patients were collected in the EPR group, including 45 males, and 18 females, with a mean age of 45.0±11.5 years, mean body mass index (BMI) of 23.3± 3.0 kg/m2; mechanism of injury: 45 high fall injuries, 12 traffic accidents, 6 other injuries; fracture sites: 5 cases of T12 vertebral fractures, 33 cases of L1 vertebral fractures, as well as 25 cases of L2 vertebral fractures. The mean LSC score was 7.8± 0.9; 45 fractures healed well (type I, 23; type II, 22) (71.4%) (Fig. 4) and 18 fractures healed poorly (18.6%) (type III, 16; type IV, 2); no implant breakage occurred. A total of 65 patients were collected in the IS group, 46 males, and 19 females, with a mean age of 45.0± 9.8 years, mean BMI of 23.4± 4.1 kg/m2; mechanism of injury: 52 high fall injuries, 8 traffic accidents, 5 other injuries; fracture sites: 6 cases of T 12 vertebral fractures, 35 cases of L1 vertebral fractures, 24 cases of L2 vertebral fractures. The mean LSC score was 7.5 ± 1.0; 31 (type I, 8; type II, 23) fractures healed well (47.7%) and 34 fractures (52.3%) healed poorly (type III, 30; type IV, 4) (Figs. 5, 6); 6 cases had implant breakage. No differences with statistical significance were identified between the EPR group and the IS group in gender, age, BMI, mechanism of injury, fracture site, AO classification, endplate injury classification, as well as LSC score. The rate of good fracture healing reached 71.4% in the EPR group compared with 48.7% in the IS group, thus marking a statistically significant difference between the 2 groups (p= 0.006). The risk of implant breakage achieved statistical significance in the EPR group compared with the IS group (p= 0.04), and the risk of implant breakage was lower in the EPR group (0) compared with the IS group (9.2%) (Table 1).
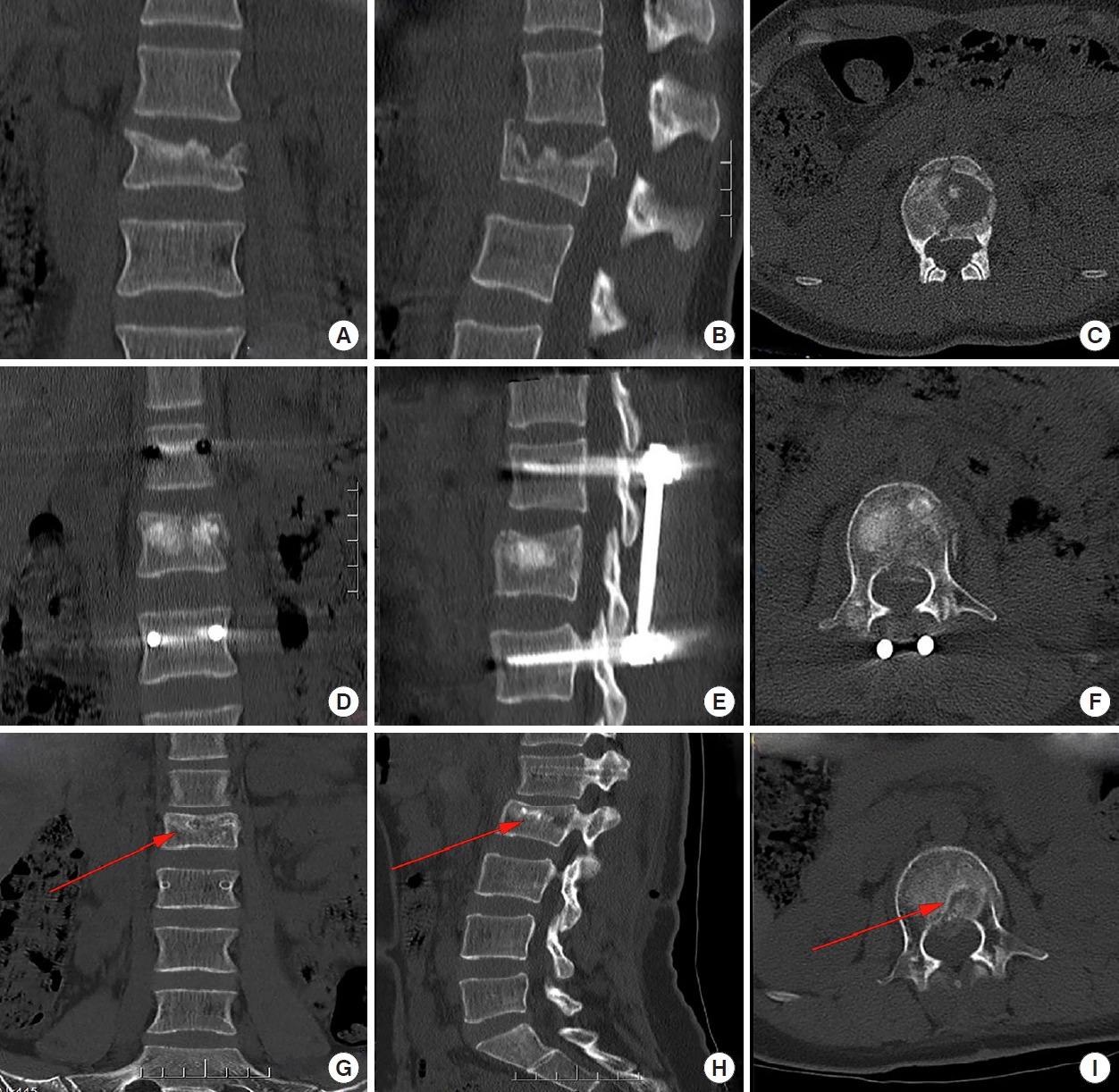
Male, 57 years old, fall from height, L2 vertebral fracture treated with the method of endplate reduction group. Preoperative fracture on computed tomography (CT) scan (A-C), postoperative repositioning and allograft bone filling on CT scan (D-F), fracture healing at 12 months follow-up on CT scan (G-I). The red arrows mark good healing of the vertebra after bone grafting.

Female, 24 years old, L2 vertebral fracture, posteriorly fixed with the method of intermediate screws group. Computed tomography (CT) scan shows poor healing. (A-C) Coronal, sagittal, and axial CT scan. The red arrows mark poor vertebral healing with significant cavities.
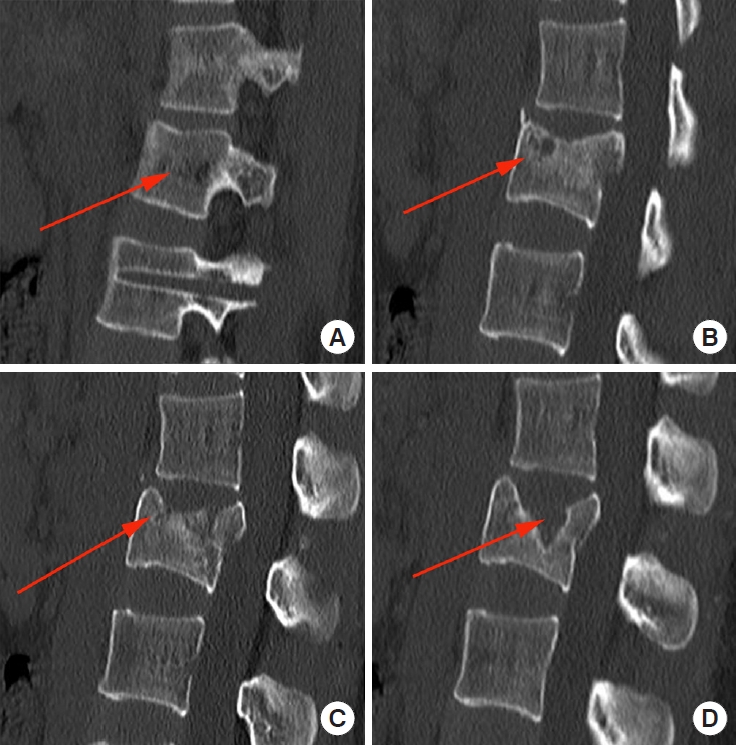
Vertebral fracture healing type: (A) type I, heals well without significant cavity; (B) type II, heals well with a small residual cavity not involving the endplate; (C) type III, heals poorly with a large residual cavity involving a small part of the endplate; (D) type IV, heals poorly with a large residual cavity involving most of the endplate on one side. The red arrows mark the different patterns of vertebral healing.
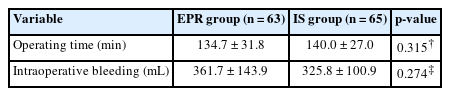
2. Intraoperative Indicators
The mean operative time was 134.7± 31.8 minutes and the mean intraoperative bleeding was 361.7± 143.9 mL in the EPR group; the mean operative time was 140.0± 27.0 minutes and the mean intraoperative bleeding was 325.8± 100.9 mL in the IS group. The differences in operative time (p= 0.315) and intraoperative bleeding (p= 0.274) between the 2 groups were not statistically significant (Table 2).
3. Radiographic Outcomes
The preoperative VWA reached 16.3°± 6.0° in the EPR group and 17.3°± 4.1° in the IS group, while no differences with statistical significance were identified between the 2 groups (p=0.139). The postoperative VWA was corrected to 5.0°± 3.3° in the EPR group and 4.5°± 8.7° in the IS group. At 12 months postoperatively, the VWA was lower in the EPR group at 6.8°±3.2° as compared with that in the IS group at 7.8°± 10.6°, whereas the above data were no differences with statistical significance. At 12 months postoperatively, the loss of correction in the EPR group was 1.9° ± 1.6° compared with 3.3°± 1.9° in the IS group, which were differences with statistical significance (p< 0.001).
The preoperative CA was 18.0°± 9.4° in the EPR compared with 15.1°± 6.2° in the IS group, but there were no differences with statistical significance between the 2 groups (p = 0.123). The CA was corrected to 4.9°± 5.1° in the EPR and 4.8°± 4.3° in the IS group, with no differences with statistical significance between the 2 groups (p = 0.664). At 12-month postoperative follow-up, the CA was maintained at 7.5°± 5.0° in the EPR compared with 8.2° ± 5.1° in the IS group, whereas there were no differences with statistical significance (p= 0.31).
The AVBH in the EPR was corrected from 63.4%± 12.3% preoperatively to 96.2% ± 2.5% postoperatively, and it was maintained at 94.2% ± 2.6% at 12-month postoperative follow-up. The AVBH in the IS group was corrected from 61.0%± 10.1% preoperatively to 95.8%± 5.1% postoperatively, and it was maintained at 92.1% ± 5.7% at 12-month postoperative follow-up. The differences in preoperative (p = 0.222) and postoperative AVBH (p= 0.173) did not achieve statistical significance compared with the 2 groups. The AVBH in the EPR at 12-month postoperative follow-up was 94.2%± 2.6% greater than that in the IS group at 92.1% ± 5.7%, and differences with statistical significance existed between the 2 groups (p< 0.001). The loss of correction in the EPR was 2.0%± 1.2% less than that in the IS group at 3.7%± 2.5%, thus marking differences with statistical significance between the 2 groups (p< 0.001).
The preoperative MVBH was 69.4%± 10.8% in the EPR and 67.2%± 13.5% in the IS group, with no differences with statistical significance between the 2 groups (p = 0.495). In the EPR group, the postoperative MVBH was corrected to 95.2%± 3.9% and maintained at 93.4%± 2.9% at 12-month postoperative follow-up, with a correction loss of 1.8%± 2.6% all better than the postoperative corrected height of 92.9%± 4.6% in the IS group, with a follow-up height of 89.4%± 4.4% and a correction loss of 3.5%±2.7%, with differences with statistical significance between the 2 groups (p< 0.001).
The preoperative UEPL was 114.4%± 7.0% in the EPR group and 114.8%± 6.3% in the IS group, with no differences with statistical significance between the 2 groups (p= 0.905). The EPR group corrected the UEPL to 103.1%± 2.6% postoperatively and maintained it at 104.3%± 3.5% at 12-month postoperative follow-up, with a correction loss of 1.2%± 2.6%, which was better than the postoperative correction of 105.2% ± 3.3% in the IS group, and 108.1%± 4.4% at follow-up, with a correction loss of 2.9%± 2.5%, with differences with statistical significance between the 2 groups (p< 0.001) (Table 3).
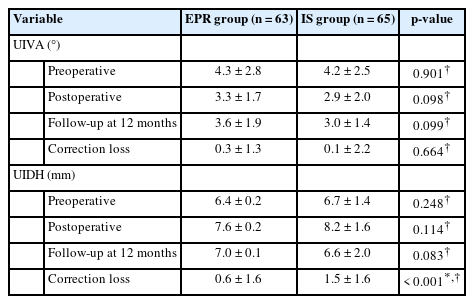
The EPR group had a preoperative UIVA of 4.3°± 2.8°, corrected to 3.3°± 1.7° postoperatively and maintained at 3.6°± 1.9° at 12-month follow-up, with a corrected loss of 0.27°± 1.30° versus 4.2°± 2.5° preoperatively, 2.9°± 2.0° postoperatively and 3.0° ± 1.4° at follow-up in the IS group, with a corrected loss of 0.12° ± 2.19°. The differences between the 2 groups were not statistically significant. In the EPR group, the UIDH was 6.4± 0.2 mm preoperatively, 7.6± 0.2 mm postoperatively, and 7.0± 0.1 mm at the 12-month postoperative follow-up; in the IS group, it was 6.7± 1.4 mm preoperatively, 8.2± 1.6 mm postoperatively and 6.6± 2.0 mm at the follow-up, with no differences with statistical significance between the 2 groups. However, the loss of disc height in the EPR group was 0.6± 1.6 mm less than the loss of 1.5± 1.6 mm in the IS group, and the difference between the 2 groups was statistically significant (p< 0.001) (Table 4).
DISCUSSION
The technique in EPR group is suitable for thoracolumbar fractures without symptoms of neurological injury, with symptoms of neurological injury, often requiring spinal canal decompression, and poor stability with 4-screw fixation alone. This technique is particularly useful for patients with thoracolumbar fractures with severe central endplate injuries. The LSC score was previously often used to determine whether to perform anterior surgery, and the risk of failure with posterior fixation was higher with an LSC score > 7. The LSC score is used as a reference and is no longer strictly standard for posterior fixation alone [18,24]. In our study, the ERP group was used to directly pry and reposition the endplate and implant allograft bone to fill the bone defect, maintaining endplate repositioning and achieving reconstruction of the anterior and middle columns of the vertebral body. Some studies demonstrated that the strength of the 4-screw fixation using a short posterior approach across the injured vertebral body was adequate compared to the 6-screw fixation method of IS group by repositioning the endplate and effectively filling the bone defect, consistent with the results of this study [25-27].
The EPR group and the IS group were compared in this study, focusing on the assessment of radiological indices. The result indicated that the EPR group had no significant advantage over the IS group in resetting the VWA, CA, and AVBH, whereas it maintained the resetting better with less postoperative correction loss. The EPR group provided better repositioning of the MVBH and UEPL than the IS group, with better postoperative maintenance and less postoperative loss.
Good EPR is capable of allowing for the repositioning of the vertebral body and intervertebral disc, thus leading to better maintenance of the repositioning effect, reducing the risk of internal fixation fracture, and reducing the incidence of recurrent kyphosis [27,28].
In recent years, the importance of EPR has begun to attract the attention of orthopedic surgeons [12,25,29]. EPR is important, but indirect repositioning methods that rely solely on ligamentous distraction are not effective in restoring the collapse of the central endplate injury [22,25,26], which directly affects the change in the vertebral space and increases the risk of recurrent kyphosis and chronic low back pain [30].
Endplate prying was employed in the EPR group, prying the endplate and disc as a whole to directly pry and reposition the endplate injury, by prying from a thinner pedicle opener (4 mm), thus increasing the flexibility of the prying and facilitating adjustment of the prying direction and positioning. Subsequently, the Schanz screw (6.2 mm) was adopted to increase the range and reliability of the pry repositioning, allowing satisfactory endplate repositioning to be achieved. Balloon-assisted reduction (percutaneous kyphoplasty) combined with posterior short-segment internal fixation refers to a common method of EPR. The above method comprises the placement of a balloon in the fractured vertebral body, controlled expansion of the balloon to reset a central endplate injury, and then the removal of the balloon followed by cement filling to maintain the reduction [13]. This method is effective in repositioning central endplate collapse [14], whereas it faces difficulty in positioning the balloon at the base of the collapsed endplate, which is not sufficiently fine. Besides, there exists inevitably some loss of repositioning of the endplate when the balloon is removed for cement filling [12]. Another disadvantage of the balloon-assisted system is that it is complex and costly to perform. Currently, IS have been more commonly used, where 2 pedicle screws are placed through the fractured vertebral body to assist in resetting the central endplate injury [10,17,31]. To be specific, 2 slightly shorter pedicle screws are placed underneath the collapsed central endplate, and pressure is applied to the pedicle screw and connecting rod to reposition the collapsed endplate. The above method is capable of facilitating repositioning of the central endplate, whereas the placement of the pedicle screw in the fractured vertebral body can cause further compression of the injured vertebral body, thus resulting in redisplacement of the fracture and risk of injury to the spinal cord [32]. Effective repositioning of the central endplate collapse is achieved by inserting the pedicle screw at the base of the endplate collapse and then using the appropriate movement of the screw to achieve precise repositioning of the endplate. The IS method is capable of only achieving rough repositioning of the central endplate injury by adjusting the length and orientation of the pedicle screws, while precise repositioning is difficult to achieve. Percutaneous screw fixation of thoracolumbar fractures is also widely used in clinical practice. This technique is less traumatic to the soft tissues and results in a faster recovery, shorter hospital stays, and a lower risk of infection. Both fourscrew and 6-screw fixation methods have been used in the application of this technique and have achieved good clinical results [33,34]. However, this technique relies on an indirect approach to repositioning vertebral fractures. The screws placed in the injured vertebral body are polyaxial screws, which do not adequately reposition the endplate of the injured vertebral body, and the soft tissue obstruction also has an impact on the operation of indirect repositioning [35,36]. The percutaneous screw technique is more suitable for patients with peripheral endplate injuries, where effective repositioning can be achieved by indirect repositioning, but satisfactory repositioning cannot be achieved for vertebrae with central endplate injuries.
The approach of the EPR group is effective in slowing disc degeneration and reducing loss of disc height (0.6± 1.6 mm vs. 1.5± 1.6 mm, p< 0.001). Effective endplate repositioning restores normal disc space and helps to slow disc degeneration, maintain normal disc space, and reduce recurrent kyphosis and chronic low back pain [23,27,37,38].
The EPR group resulted in better vertebral healing (71.4% vs. 47.7%, p= 0.006), the varying degree of a cavity remaining in the vertebral body after endplate repositioning can result in loss of fracture reduction and affect vertebral fracture healing, with considerable vertebral fractures still finding cavities when the internal fixation is removed, resulting in loss of vertebral reduction and recurrent kyphosis [17]. To better maintain the reduction and promote fracture healing, we use the allograft bone implant technique, which effectively promotes fracture healing and good postoperative resorption [25]. It is less traumatic, has fewer complications, and is more comfortable than the use of autogenous bone grafting [22]. In contrast, the use of bone cement implants to fill the cavity, has the potential for leakage of the bone cement into the intervertebral disc, muscle block, and venous system, with adverse consequences [39], though beneficial for filling the residual cavity after reduction and for maintenance of EPR [9]. Bone cement is also difficult to absorb within the vertebral body and prolonged retention within the vertebral body can have a detrimental effect on adjacent vertebrae and discs [26,40].
The risk of implant breakage was lower in the EPR group than in the IS group (0% vs. 9.2%, p= 0.04). In the analysis of this study, this was partly because the fracture was better repositioned and maintained in the EPR group and the fracture healed better, which effectively relieved the stresses on the implant; and partly because the 6-screw fixation in the IS group was more robust but had a greater concentration of stresses, whereas the 4-screw fixation in the EPR group retained some mobility above and below the fractured vertebral body, which stress concentrations are reduced.
However, there are still some limitations to the above approach. First, the sample size was relatively small, which may affect the authenticity of the results. Second, direct prying and repositioning of the endplate only apply to patients with upper endplate injuries, and prying and repositioning of the endplate were difficult to achieve with lower endplate injuries. Third, the degree of prying and repositioning and the amount of implantation of allogeneic bone are difficult to control precisely, which require monitoring and manipulation under an x-ray fluoroscope.
CONCLUSION
Both the EPR group and the IS group achieved good repositioning results based on the treatment of single vertebral burst fractures of the thoracolumbar, whereas the EPR group was more effective in repositioning and maintaining MVBH, as well as endplate morphology, which achieved good maintenance of VWA, CA, AVBH, and endplate morphology after repositioning and less correction loss. The EPR group exhibited a better healing pattern after vertebral fracture, provided better relief from disc degeneration, and achieved a lower risk of implant breakage.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: PW; Data curation: JH, YC; Formal analysis: JH; Methodology: SY; Project administration: DR, HW, PW; Visualization: LG; Writing - original draft: JH; Writing - review & editing: JH