Biportal Endoscopic Posterior Cervical Foraminotomy for Adjacent 2-Level Foraminal Lesions Using a Single Approach (Sliding Technique)
Article information
Abstract
Objective
Endoscopic posterior cervical foraminotomy (PCF) using uniportal or biportal endoscopic approach has been performed for cervical foraminal stenosis or foraminal disc herniation. Two-level PCF is possible using a single biportal endoscopic approach. The purpose of this study was to present a technique of biportal endoscopic PCF for contiguous 2-level foraminal lesions using a single approach and its clinical results.
Methods
Patients who received 2-level PCF using a single biportal endoscopic approach were enrolled in this study. We analyzed their clinical data including age, sex, complications, and Neck Disability Index (NDI), and visual analogue scale (VAS) of neck and arm. Postoperative magnetic resonance image was taken on the first postoperative day to determine whether there was sufficient decompression.
Results
We successfully performed biportal endoscopic PCF for adjacent 2-level foraminal lesions using a single approach (sliding technique) in all 12 patients. There were cervical foraminal disc herniation with foraminal stenosis (5 cases) and 2-level foraminal stenosis (7 cases). Preoperative mean NDI and VAS of arm and neck significantly decreased at 12 months after surgery. Postoperative clinical outcomes were excellent in 5 patients, good in 6 patients, and fair in 1 patient. There was no major complication.
Conclusion
Two-level PCF could be performed using a single approach biportal endoscopic surgery with only 2 skin incisions. Clinical outcomes are favorable. This sliding PCF technique using biportal endoscopic approach might be an alternative surgical treatment for contiguous 2-level cervical foraminal pathologic lesions.
INTRODUCTION
Posterior cervical foraminotomy (PCF) is a good surgical treatment option for cervical radiculopathy such as cervical foraminal stenosis and foraminal disc herniation. Minimal invasiveness, familiar surgical anatomy of posterior cervical approach, and motion preservation are advantages of PCF or discectomy. Recently, endoscopic PCF using uniportal or biportal endoscopic approaches have been attempted instead of microscopic PCF using tubular retractor systems [1-3]. Early recovery after surgery and minimal invasiveness are advantages of full endoscopic or biportal endoscopic PCF [4,5].
Compared with lumbar vertebrae, cervical vertebrae have a shorter interval between adjacent 2 segments (Fig. 1). A small dissection of multifidus muscle allows easy access to adjacent cervical segments without making an additional portal. Cervical lordotic curve also facilitates access to the adjacent cervical level. Therefore, 2-level PCF can be performed by a single endoscopic approach [6]. Even in the biportal endoscopic cervical approach, 2-level PCF is possible using a single biportal endoscopic approach with only 2 skin incisions [6]. Since a slight movement of the 2 portals allows direct access to adjacent foraminal lesion, PCF of 2 adjacent foraminal lesions with a single endoscopic approach is also called a “sliding technique” of PCF [6].
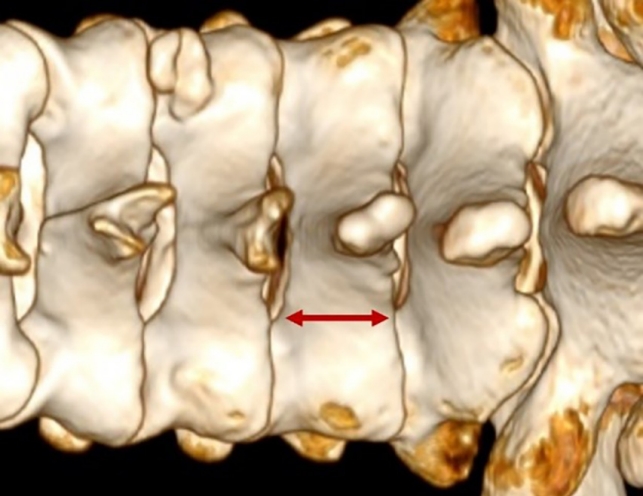
The distance between the interlaminar space of 2 adjacent levels in the cervical spine is shorter than that of the thoracolumbar area (arrow).
The purpose of this study was to present the technique of biportal endoscopic PCF for adjacent 2-level foraminal lesions using a single approach and clinical results of this technique.
MATERIALS AND METHODS
1. Patients and Clinical Data Analysis
Patients who received 2-level PCF using a single biportal endoscopic approach (sliding technique) were enrolled in this study. All enrolled patients were followed up for more than 12 months after surgery. Prospectively collected data were retrospectively reviewed. The study design of this study is a retrospective review.
This investigation was performed in accordance with Institutional Review Board of Wiltse memorial hospital, No. W-2022-RA3).
Indications of this sliding technique of biportal endoscopic PCF were unilateral symptomatic cervical radiculopathy due to 2-level cervical foraminal stenosis or foraminal disc herniation. Those with ossification of ligamentum flavum, cervical deformity, central canal stenosis, central disc herniation, segmental instability, or infectious disease were excluded.
Clinical data including age, sex, diagnosis, operation level, operation time, complications and estimated blood loss including postoperative blood drainage were analyzed. Analyses of clinical results were performed using Odom’s criteria (excellent, good, fair, and poor), Neck Disability Index (NDI), and visual analogue scale (VAS) of neck and arm. Blood samples were collected from patients before surgery and on the first day after surgery to measure C-reactive protein (CRP) and creatine phosphokinase (CPK) levels. Postoperative magnetic resonance imaging (MRI) was taken on the first postoperative day to confirm whether there was sufficient decompression or disc removal at symptomatic cervical foraminal area. Cervical flexion/extension dynamic x-rays were taken at 6 months and 12 months after surgery for evaluating instability at operation segments. Blood samples were collected from patients before surgery and on the first day after surgery to measure CRP and CPK levels to evaluate muscle injury of the operation area. CPK and CRP blood tests were also performed before and on the first day after surgery for single-level biportal endoscopic PCF patients who underwent surgery at the same time. Degrees of CPK and CRP elevation after surgery were compared between single-level PCF patients and 2-level PCF patients using the sliding technique. Since patient sample was small, nonparametric statistics were used. Statistical analysis was performed using Wilcoxon signed rank test, and Kruskal-Wallis test. Difference with a p < 0.05 was considered to be statistically significant. R 4.2.2 (R Foundation for Statistical Computing, Vienna, Austria)was used for all statistical analyses.
2. Surgical Technique
1) Surgical instruments
A working sheath was needed to maintain the patency of continuous irrigation saline (Fig. 2B). Smooth drainage of irrigation can maintain a good endoscope view and prevent the rise of epidural pressure during a biportal endoscopic surgery [7]. Radiofrequency probes were necessary for bleeding control and soft tissue dissection [7,8]. Waterproof diamond drill was used for foraminotomy. We recommend the use of smaller size hooks or dissectors in biportal endoscopic cervical posterior approach when comparing instruments of lumbar surgery.
2) Making 2 portals
Two channels including an endoscopic portal and a working portal should be created under fluoroscopic C-arm view (Figs. 2, 3) [3,4]. When performing 2-level PCF at C5-6-7, 2 portals were made at C5 and C7 pedicle levels (Fig. 3). In anteroposterior x-ray view, 2 portals were lateral border of pedicle of C5 and C7. Usually, an endoscopic portal was made for the nondominant hand and a working portal was made for the dominant hand. Small stab skin incision was made about 10 mm in length for the working portal [8]. We put in serial dilators under C-arm fluoroscopic monitoring. Finally, the working sheath with an optimal length was inserted at the working portal. An addition stab skin incision of 5 to 7 mm in length was made to create an endoscopic portal. A trocar of endoscopy was inserted for making an endoscopic portal under x-ray fluoroscopic monitoring. Two portals should contact over the facet joint. Continuous saline must be well drained from the endoscopic portal to the working portal.
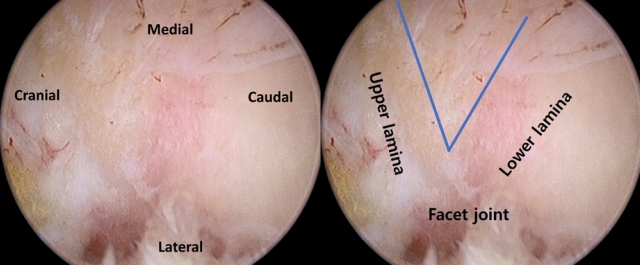
3) Lamino-foraminotomy of first level (Supplementary video clip 1)
In many cases, the cranial lesion was easier to check the level. Thus, cranial lesion was operated first. However, this depends on the preference of the operator. Ipsilateral upper and lower laminae and facet joint were dissected and partially exposed using dissectors and radiofrequency (RF) probes. First, a surgical landmark of V-point consisted of inferior border of upper lamina and superior border of lower lamina (Fig. 4) [2]. After finding the V-point, laminotomy was performed using a drill and small sizes of Kerrison punches (1 or 2 mm). First, the lamina was thinned with a diamond drill. The lamina was then removed with a Kerrison rongeur. A sufficient foraminotomy was performed by medial facetectomy (removal of lateral mass). Medial facetectomy was done with a diamond drill and a Kerrison rongeur. After bone work, ligamentum flavum was exposed. If ligamentum flavum was partially removed, nerve root and dura were seen. If a patient had foraminal disc herniation, ruptured disc particles were removed through axilla area. A cervical nerve root of cranial level was completely decompressed (Fig. 5). After bleeding control, 2 portals were moved to the adjacent caudal level (Fig. 5).
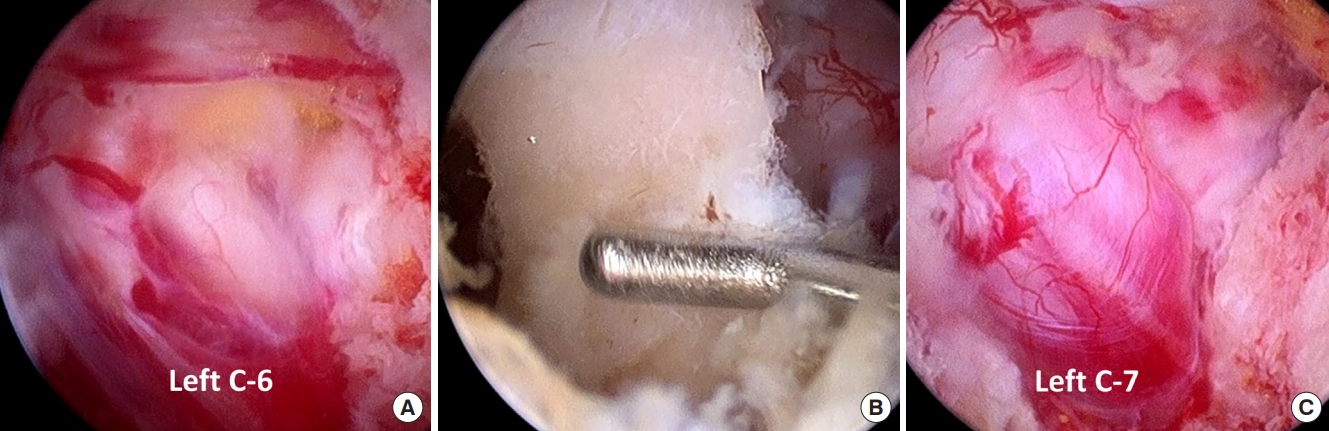
Intraoperative endoscopic images of biportal endoscopic posterior cervical foraminotomies at C5-6-7 left. (A) Left C6 nerve root was completely decompressed. (B) Intermediate laminae of C6 and 2 foraminotomy holes were seen while performing the sliding technique. (C) Left C7 nerve root was also fully decompressed after biportal endoscopic decompression using the sliding technique.
4) Sliding moving of 2 portals to adjacent level (Supplementary video clip 1)
Two portals (endoscopic portal and working portal) were tilted vertically to caudal adjacent segment for foraminotomy (Figs. 5, 6). Multifidus muscle of adjacent level was dissected and ablated using RF probes. Laminae of lower level was relatively easily exposed using RF probes. Firstly, the V-point of lower adjacent level was confirmed. The same posterior foraminotomy was done. A cervical nerve root of contiguous caudal level was completely decompressed (Figs. 5, 7). After bleeding was meticulously controlled, a drainage catheter was inserted. A drainage catheter and its bag were removed at one or 2 days after surgery.
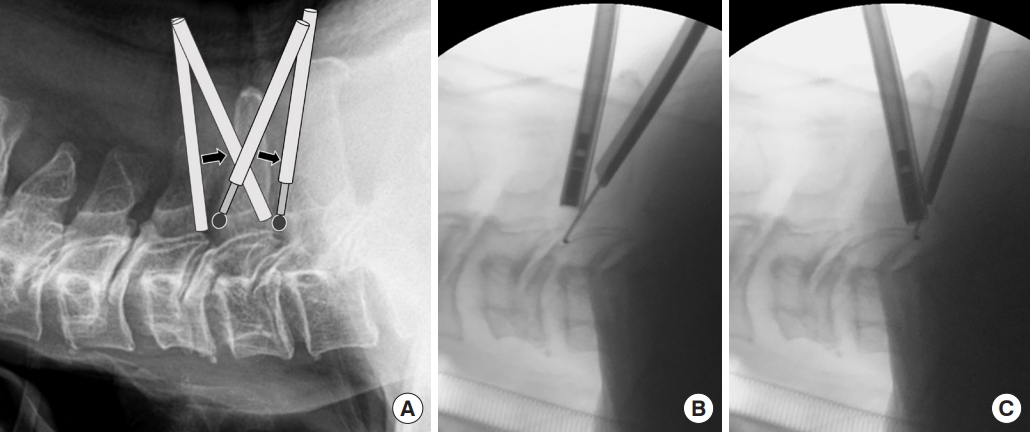
(A) Schematic drawing of the sliding technique. Two contiguous levels of posterior cervical foraminotomy can be achieved using a biportal endoscopic single approach. (B, C) Two-level posterior cervical foraminotomy was available by shifting 2 portals without making any additional portals.
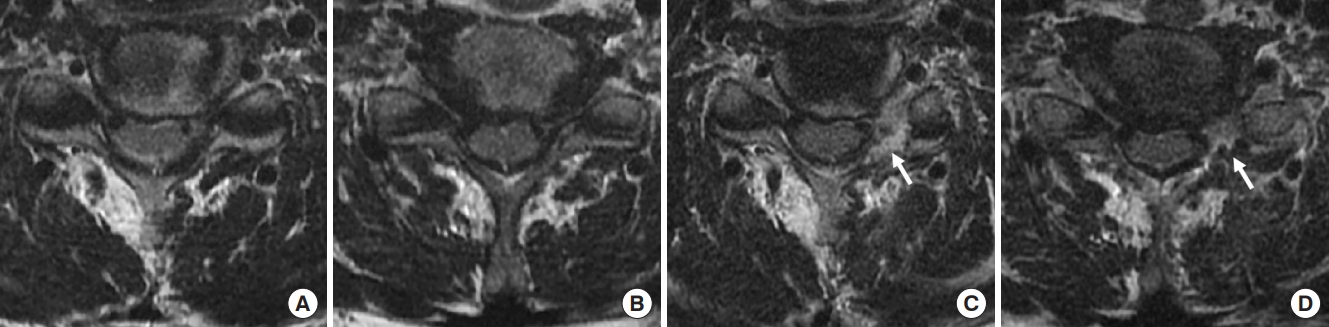
A 71-year-old male patient presented with radiating left arm pain. (A, B) Preoperative magnetic resonance (MR) images showed left-sided foraminal stenosis at C5-6-7. We performed left-side biportal endoscopic posterior cervical foraminotomy using a single sliding approach. After surgery, the patient’s radiating pain was significantly improved. (C, D) Postoperative MR images revealed full decompression of left foraminal stenosis at C5-6-7 (white arrows).
RESULTS
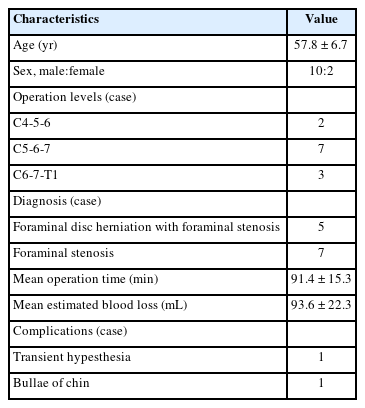
A total of 19 patients have been treated by this biportal endoscopic sliding technique from October 2019. After excluding 7 patients from this study due to a short follow-up period, 12 patients were treated with this technique. There were 2 females and 10 males. Their mean age was 57.8 ± 6.7 years. The mean follow-up period was 13.6 ± 1.9 months. We successfully performed biportal endoscopic PCF for adjacent 2-level foraminal lesions using the single approach (sliding technique) in all enrolled patients (n = 12). Postoperative MRI revealed well decompression of foraminal lesions after surgery (Fig. 7). Diagnoses included cervical foraminal disc herniation with foraminal stenosis (5 cases) and 2-level foraminal stenosis (7 cases). Operation levels involved C4-5-6 (2 cases), C5-6-7 (7 cases), and C6-7-T1 (3 cases). The average operation time was 91.4 ± 15.3 minutes. The mean postoperative estimated blood loss was 93.6 ± 22.3 mL (Table 1).
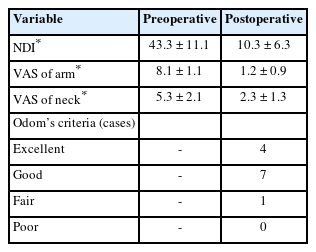
Preoperative mean NDI significantly decreased from 43.3 ± 11.1 to 10.3 ± 6.3 at 12 months after surgery (p < 0.05) (Table 2). Preoperative arm pain (VAS of arm) decreased significantly from 8.1 ± 1.1 to 1.2 ± 0.9 at 12 months (p < 0.05). Preoperative VAS of neck decreased significantly from 5.3 ± 2.1 to 2.3 ± 1.3 at 12 months after surgery (p < 0.05) (Table 2). According to Odom’s criteria, postoperative clinical outcomes were excellent in 4 patients, good in 7 patients, and fair in 1 patient. Epidural injection was performed at 3 months after surgery in the patient with a fair outcome after surgery. There were 2 minor complications. One patient complained of temporary numbness of forearm, but recovered spontaneously. One patient developed small bullae on the chin area after surgery. It might be caused by a problem associated with the surgical position. However, it healed well without scarring. No instability was found on dynamic x-ray taken at 1 year after surgery. No patient underwent reoperation in this study. Preoperative and postoperative CPK and CRP blood levels were checked for 12 patients with 2-level PCF surgery and 18 patients with 1-level PCF surgery. Mean preoperative CPK blood level (normal range, 32–294 IU/L) increased from 113.3 ± 38.3 to 140.1 ± 50 IU/L postoperatively in patients with 1 level PCF, and from 122.9 ± 30.0 to 170.8 ± 4.1 IU/L postoperatively in patients with 2-level PCF. Mean preoperative CRP blood level (normal range, 0.5 mg/dL) increased from 0.02 ± 0.02 to 0.28 ± 0.17 mg/dL postoperatively in patients with one level PCF and from 0.11 ± 0.24 to 0.37 ± 0.37 mg/dL in patients with 2-level PCF. There was no significant difference in CPK or CPR blood level elevation between the 2 groups (p > 0.05).
DISCUSSION
Biportal endoscopic PCF has been attempted for cervical unilateral radiculopathy caused by foraminal stenosis or disc herniations. The biportal endoscopic cervical approach can minimize injury to musculoligamentous structures with a clean, magnified surgical field. Contiguous 2-level cervical foraminal lesions could be treated using only 2 portals in the biportal endoscopic posterior cervical approach. The pivoting of 2 portals could provide access to 2 contiguous levels of cervical foraminal pathologic lesions. Even if the endoscopic surgical corridor to the surgical site is incorrectly created, it can be easily corrected to an appropriate surgical level without making a new skin incision under fluoroscopic guidance. Two-level PCF can be operated using a single endoscopic approach, including biportal or uniportal endoscopic surgeries [6].
Indications for biportal endoscopic PCF were similar to those for conventional open PCF or minimally invasive approach with tubular retractor systems. Cervical foraminal stenosis and foraminal disc herniations were indications for using a biportal endoscopic approach [3]. Adjacent 2-level lesions could be treated using this sliding biportal endoscopic cervical approach (Fig. 7) [6]. Preoperative instability and tumor lesions were contraindications of this approach. This sliding technique can be used to perform adjacent 2-level PCF with or without discectomy. Usually, 3-level foraminotomies cannot be achieved using this sliding single biportal endoscopic approach. Cervical myelopathy cannot be treated by this approach.
The epidural vein was the main bleeding focus. Epidural vein bleeding must be prevented and controlled using RF probes. To prevent postoperative instability, it is recommended not to remove more than 1/2 of the lateral mass (the facet joint). Cervical nerve roots frequently consist of dual nerve roots including motor and sensory nerve roots [9]. The possibility of dual cervical nerve roots should always be kept in mind to prevent motor nerve root injury. When finding or removing ruptured disc particles around the nerve root, it is strongly recommended to minimize nerve root retraction and manipulation as much as possible [4]. If the axillary area of the cervical nerve root is very narrow, partial removal of the pedicle (pediculotomy) can make enough axillary space for disc exploration or removal. If dura tear or bleeding control is difficult, switching to microsurgery without delay is recommended. A face pillow must be used to avoid unnecessary pressure on the face, including eyeballs. If patients have a central disc herniation, an anterior cervical approach should be considered rather than a posterior endoscopic approach. Cervical myelopathy cannot be treated using this biportal endoscopic posterior foraminotomy. To create portals at the correct surgical site and avoid wrong-level surgery, intraoperative C-arm fluoroscope monitoring should be performed [4]. If 2-level PCF is difficult with a single sliding approach using only 2 portals, making an additional portal should be considered. If 2-level PCF is difficult to perform with only 2 portals, it might be necessary to create an additional portal for complete decompression. If bleeding control is difficult and the surgical field is blurred, it might be necessary to switch from biportal endoscopy to conventional microsurgery. Three-level PCF is difficult to perform using only a 2-portal biportal endoscopic approach.
According to a systematic review paper, when PCF was compared with anterior cervical discectomy and fusion (ACDF), there was no significant difference in clinical outcome, complication rate, or reoperation rate. Compared to ACDF, PCF has advantages in that the cost is lower and the increase in ROM in the adjacent part is smaller. However, indication of PCF is narrower than that of ACDF. In this study, we did not experience revision surgery or major complications.
This study design was a retrospective review of cases series and not a randomized controlled trial. A small number of patients were enrolled in this study. Also, the follow-up period was as short as 12 months. To accurately analyze clinical results and advantages of this surgical technique, a large number of patients and a case control study are needed in the future. And, a long-term follow-up study of more than 2 years are required.
CONCLUSION
We successfully performed 2-level PCF using a single approach biportal endoscopic surgery with only 2 skin incisions. Two-level PCF can be sufficiently performed using 2 channels. The degree of muscle damage may be small. A 2-level biportal endoscopic PCF using a single approach might reduce skin wound size, number of portals, and operation time. This sliding PCF technique might be an alternative surgical treatment for contiguous 2-level cervical foraminal pathologic lesions. However, a randomized controlled trial should be required for accurate clinical research of this technique.
SUPPLEMENTARY MATERIALS
Supplementary video clip 1 can be found via https://doi.org/10.14245/ns.2346144.072.
Video clip of the sliding technique of 2-level posterior cervical foraminotomy. We performed a left-sided 2-level posterior cervical foraminotomy using the sliding technique in a patient with left-sided foraminal stenosis of C 5-6-7.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: DHH, JSH, JWJ; Data curation: DHH; Formal analysis: DHH; Methodology: DHH, JSH, JWJ; Visualization: DHH; Writing - original draft: DHH, JSH; Writing - review & editing: JWJ.