 |
 |
- Search
| Neurospine > Volume 19(3); 2022 > Article |
|
|
Abstract
Objective
We compared the midterm clinical and radiological outcomes between 2 types of full endoscopic posterior cervical foraminotomy, including conventional posterior endoscopic cervical foraminotomy (PECF) and modified inclined technique for PECF.
Methods
One of the 2 types of PECF surgery was performed for defined cervical foraminal stenosis. The foraminal expansion ratio and facet resection rate and foraminal stenosis grade were measured using magnetic resonance imaging. Visual analogue scale (VAS) scores for neck and arm pain, neck disability index, MacNab criteria, operation time, hospital stay, and complications, including postoperative dysesthesia, were assessed. Clinical and radiological parameters were compared between the 2 surgical groups.
Results
There were 49 and 46 patients in the PECF and modified-PECF groups, respectively. The modified-PECF group showed significantly higher expansion of distal foraminal diameter and foraminal height, and a lower facet resection rate compared to PECF group (in all, p<0.001). The modified-PECF group displayed significantly lower VAS score for neck pain at 1 day and 1 week after surgery and lower arm pain VAS score after 6-month follow-up (p=0.002, p=0.001, p=0.002, respectively).
Conclusion
Compared with the PECF, the modified inclined technique has radiologic benefits, including enhanced facet joint preservation, restoration of the natural course of nerve roots, and prevention of restenosis by expanding the superior articular process base, especially in grade 2 foraminal stenosis. Furthermore, the modified inclined technique significantly improved the postoperative VAS score for neck pain within the 1-week follow-up and that of arm pain after 6-month follow-up.
Cervical radiculopathy is a degenerative spinal disease that leads to neck and arm pain, a typical symptom of nerve root compression caused by foraminal stenosis or intervertebral disc herniation [1,2]. When conservative treatment fails, surgical treatments, such as posterior cervical foraminotomy (PCF), anterior cervical discectomy with fusion, or disc replacement are considered [1,3]. With the development of minimally invasive surgery, PCF has been performed using a tubular retractor or endoscopic system and has shown favorable clinical outcomes with the benefit of blood loss, operating time, and hospital stay compared to open PCF surgery [4-6].
Full endoscopic PCF has shown good clinical and radiologic outcomes [7-10]. Endoscopic systems offer a multiaxial viewing angle and a magnified clear endoscopic view that enable detailed bone decompression using various approaches [9,11]. A recent comparative study by Kim et al. [12] revealed that endoscopic PCF offered enhanced facet joint preservation and improved midterm clinical results compared to microscopic PCF. Furthermore, full endoscopy offers a safe surgical route for ventral foraminal decompression via partial pediculotomy or partial vertebrotomy, and it shows good surgical outcomes [13]. We performed a full endoscopic PCF to treat osseous cervical foraminal stenosis using both pedicular-vertebrotomy techniques for ventral foraminal decompression and an inclined surgical route for improved facet joint preservation. Therefore, the objective of this retrospective study was to compare the clinical and radiological outcomes of full endoscopic PCF and modified inclined approach.
This study was a retrospective analysis of patients who underwent 2 types of posterior endoscopic cervical foraminotomy (PECF) using a full endoscopic system to treat radiculopathy due to osseous foraminal stenosis between January 2020 and June 2021 at Wiltse Memorial Hospital. All the procedures were performed by 2 experienced spine surgeons, according to each surgeon’s preferences. One surgeon with 10 years of experience in PECF performed the foraminotomy with or without minimal pediculotomy. Another surgeon with 7 years of experience in PECF performed the foraminotomy using a modified inclined technique. All consecutive patients who met the inclusion criteria were included in this study. Physicians collected clinical and radiologic data during the follow-up period. We included all consecutive patients who met the following criteria:
(1) Presence of radiculopathy symptoms in the neck, back, and arm with more than 6 weeks of failed conservative treatment.
(2) Osseous foraminal stenosis was confirmed with magnetic resonance imaging (MRI) and computed tomography (CT) and was consistent with the symptoms of radiculopathy.
(3) One of 2 types of PECF surgery was performed for defined foraminal stenosis at the unilateral side of a single cervical level.
(4) If the operating patients had other asymptomatic foraminal lesion or had previously undergone different levels of PCF, we included
We excluded patients if they met any of the following criteria:
(1) Foraminal soft herniated disc was the primary pathology than osseous stenosis.
(2) Operation history of fusion or artificial disc replacement in the cervical spinal levels.
(3) Other cervical operations (discectomy, multilevel foraminotomy, decompression laminectomy, fusion, and artificial disc replacement) were performed simultaneously at different levels.
(4) Accompanying segmental instability, symptomatic central stenosis, infectious disease, traumatic conditions, or musculoskeletal disorder.
We performed PECF for osseous foraminal stenosis using 2 different techniques for bone decompression using the full endoscopic system (Fig. 1A, B). All the surgeries were performed under general endotracheal anesthesia in the prone position on a chest bar, while the flexed neck was fixed using a skin tape (Fig. 1A, B).
The conventional PECF used the interlaminar endoscopic system with an endoscope with a 12° viewing angle, an 8.4-mm outer diameter, 5.7-mm diameter working channel, and a 120-mm long endoscope (Spine Endoscope, TECHCORD, Daejeon, Korea). A 1-cm skin incision was made over the uncovertebral joint line at the target level (Fig. 1C–E). After serial dilations, the working cannula was docked on the medial border of the facet joint under image intensification. After soft tissue dissection, laminotomy was performed using a 3.5-mm endoscopic drill until the proximal and distal ends of the ligamentum flavum were exposed. Bone drilling was extended laterally until medial part thinning of the superior articular process (SAP), and extended craniocaudally until the border of the upper- and lower-level pedicles were exposed. According to the surgeon’s preference, pediculotomy was not performed in most patients, except for incidental pedicle violation during facet drilling. The bony spur under the nerve root could not be removed. After confirming the decompressed nerve root, operation was finished.
The modified-PECF utilized the endoscope with a viewing angle of 30°, outer diameter of 7.3 mm, 4.7-mm working channel, and a total length of 251 mm (TESSYS, Joimax, Karlsruhe, Germany). A skin incision of 1 cm was made on the line, 1 cm medial to the uncovertebral joint line of the target level to obtain an inclined surgical route by undercutting the facet joint (Fig. 1C, D). On the lateral C-arm image, a skin incision was made on the lower endplate line of the involved disc space at a caudocranial approach angle (Fig. 1E). Docking of the working cannula, soft tissue dissection, and initial laminotomy was performed in the same manner as in the PECF (Fig. 2A). Broad bone drilling of the lower-level lamina and SAP was performed while anticipating the bone extent covering the exiting nerve root, cranial part of the lower-level pedicle, and lateral aspect of the dural sac. Bone drilling was continued until the inner cortical bone resembled a thin paper so that the contour of the pedicle and nerve root was confirmed (Fig. 2B). The thinned inner cortical bone was elevated and detached from the dura and nerve root, and the bone flap was removed with forceps (Fig. 2C). The exiting nerve root and the lateral border of the thecal sac were exposed, and thick peridural adhesions covered them (Fig. 2D). Subsequently, the thinned SAP was removed laterally using a 1-mm punch by undercutting the SAP along the exiting nerve root. The base of the SAP, where the SAP joins the pedicle, was removed using a punch to release the nerve root at the starting point that curves downward (Fig. 2E). The endoscope was tilted in the craniolateral direction and it accessed the ventral foraminal area through the space created by inclined laminotomy and pediculotomy. The bevel tip was docked in the nerve root axillary area and retracted the nerve root in an obliquely elevated pattern to prevent excessive neural retraction. Subsequently, oblique pedicular-vertebrotomy was performed to remove the bony spur and hypertrophied annulus with stepwise drilling (Fig. 2F, G). The natural downward course of the nerve root was restored through the space created by inclined pedicular-vertebrotomy (Fig. 2H). The severely collapsed intervertebral foramen is remarkably expanded, including foraminal height and lower foraminal area, without sacrificing the facet joint significantly (Fig. 2I, J). After the insertion of a closed drainage catheter, the skin was closed.
This study was approved by the Institutional Review Board (IRB) of Wiltse Memorial Hospital (NR-IRB 2022-W05). Patient characteristics including sex, age, and symptoms were recorded. The nature of the surgery, operation level, operating time, and hospital stay were also documented, as were any postoperative complications. The physicians collected clinical information preoperatively, postoperatively, and at 1 week, 1 and 6 months, and final follow-ups at the ward and an outpatient department. Clinical data at 1 week were collected to document the occurrence of postoperative dysesthesia due to nerve root retraction during the modified inclined procedures. Posterior neck and arm pain visual analogue scale (VAS) scores, neck disability index (NDI) scores, and MacNab criteria for evaluating disability and pain responses were collected. A translation ≥ 3 mm on a flexion-extension radiograph indicated instability [14]. After the surgery, almost all the patients were monitored using the above protocol; however, those with complications were treated with additional management. A single observer who highly experienced endoscopic spine surgery has measured the parameters twice. The kappa value between the 2 measurements was 0.83, indicating excellent agreement.
Dysesthesia is defined as a painful, uncomfortable sensation described as burning, icy-hot, prickly, itchy-prickly, or intensely creepy-crawly [15]. We documented postoperative dysesthesia when the preoperative dysesthetic pain character changed, dysesthetic pain severity deteriorated, and new dysesthetic symptoms were present.
Cervical foraminal stenosis was classified into the following 2 grades based on MRI findings on axial T2-weighted images at the cervical disc level, using the grading system suggested by Kim et al. [16].
Grade 0: Absence of foraminal stenosis
Grade 1: Narrowest width of neural foramen is 51%–100% of the width of the extraforaminal nerve root at the level of the anterior margin of the SAP.
Grade 2: Neural foramen width is the same as or less than 50% of the width of the extraforaminal nerve root.
We measured 4 parameters to document the changes in the neural foraminal space and facet on the pre- and postoperative T2-weighted MRI using the methods described by Nakamura and Taguchi [17] and Kim et al. [12]. Two values for the middle and distal foraminal widths and one for the facet length were measured on axial MRI from the intervertebral disc levels. One foraminal height value was measured on oblique sagittal MRI from the middle pedicle level. The preoperative and postoperative values were measured along the same plane.
(1) Midforaminal diameter (MFD): A linear distance was measured on the line, vertical to the longitudinal axis of the intervertebral foramen at the midforaminal area (Fig. 3).
(2) Distal foraminal diameter (DFD): A linear distance was measured on the line, vertical to the longitudinal axis of the intervertebral foramen at the distal foraminal part indicated 2-mm lateral to the outer border of the vertebral body (Fig. 3).
(3) Facet joint width (FJW): A linear distance between the medial and lateral borders of the facet joint was measured from T2-weighted axial MRI of the middle of the facet joint (Fig. 3).
(4) Midforaminal height (MFH): A linear distance was measured on the oblique sagittal plane, vertical to the longitudinal axis of the intervertebral foramen at the midforaminal area (Fig. 3).
(5) Foraminal expansion ratio: We calculated the foraminal expansion ratio using the calculation formulas:
(6) Facet joint resection rate: We calculated the estimated amount of facet resection using the formula:
Statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA). Continuous variables are expressed as means and standard deviations. Clinical VAS and NDI scores were measured preoperatively, postoperatively, and at 1 week, 1 month, 6 months, and final follow-up visits. The MacNab criteria were assessed at the final follow-up, which was reported by the patients and analyzed using the Wilcoxon rank-sum test. The values of radiologic parameters, other variances in operation times, and hospital stays were also analyzed using the Wilcoxon rank-sum test. A p-value of < 0.05 was considered significant.
We included 49 (30 men and 19 women) and 46 (35 men and 11 women) patients who underwent PECF and modified-PECF, respectively. The mean age was 57.1±8.4 years in the PECF group, and 56.4±5.9 years in the modified-PECF group (Table 1). The mean follow-up duration was 10.7±1.9 months in the PECF group, and 10.4±1.3 months in the modified-PECF group. The mean operation time was 61.0±12.1 minutes and 56.5±9.8 minutes in the PECF and modified-PECF groups, respectively. The mean hospital stay in the PECF group was 5.1±3.0 days, and 4.8±2.6 days in the modified-PECF group. No significant differences were found in age, follow-up duration, operation time, and hospital stay between the 2 groups (Table 1). The most common operating levels in both groups were C5–6 and C6–7 levels (Table 1). Most patients in both groups had grade 2 foraminal stenosis (Table 1).
The PECF group had 4 transient neuropraxia patients, 2 motor weaknesses, and 2 hypesthesia through the involved nerve roots. There were 5 transient neuropraxia patients in the modified-PECF group: 1 motor weakness of the involved nerve root and 4 hypesthesia of the fingertip. Most sensory neuropraxia in the modified-PECF group was localized to the fingertips of the involved nerve root distribution (Table 1). All the transient neuropraxia occurred 1 or 2 days after the surgery, which resolved within 2 weeks of conservative treatment. One week after the operation, 2 patients had postoperative dysesthesia in the modified-PECF group, which may have been caused by dorsal root ganglion (DRG) retraction with a working cannula during partial vertebrotomy. The symptoms subsided after 1 or 2 weeks of conservative treatment (Table 1). Three patients underwent modified-PECF surgery at the C4–5 level. One patient with C5 palsy with shoulder drop occurred 2 days after surgery (Fig. 4A–C). Fortunately, the patient recovered from the weakness after 2 months of conservative treatment (Table 1). Two patients had dural tears in each group. In the PECF group, one dural tear occurred during the drilling, and another during the bone punching. However, 2 dural tears in the modified-PECF group occurred during the facet joint drilling (Table 1). All the dural tear was small and treated with a fibrin sealant patch without neurologic deficits. In 2 patients of the PECF group, posterior neck pain with a different character recurred 4 weeks later (Table 1). Postoperative MRI showed excessive facet violation over 75% of facet resection, which might cause a relapse of the neck pain (Fig. 4D–F). Two patients in the PECF group relapsed with radiating arm pain after a symptom-free duration of 8 and 10 months (Table 1). One of the 2 patients underwent MRI at 1-year of follow-up, and MRI showed restenosis of the intervertebral foramen (Fig. 5A–C).
We measured the MFD, DFD, and MFH to analyze the change in foraminal width, focusing on the foraminal expansion ratio. The mean expansion ratio of MFD in the PECF group was 4.5±1.9 and 5.4±2.6 in the modified-PECF group (Table 2). Both surgical groups showed more than 4 times midforaminal expansion, and no significant difference was found between the 2 groups (p=0.164) (Table 2). The mean expansion ratio of DFD in the PECF group was 1.6±0.7 and 2.1±1.0 in the modified-PECF group (Table 2). The DFD in the modified-PECF group was significantly expanded more than in the PECF group (DFD expansion ratio, p<0.001) (Table 2). Furthermore, the modified-PECF group showed a remarkable expansion in MFH compared with the PECF group (MFH expansion ratio, p<0.001) (Table 2). In the modified-PECF group, the mean expansion ratio of MFH was 1.5±0.7 and 1.1±0.1 in the PECF group (Table 2). These radiologic results of foraminal expansion revealed that the modified inclined technique enabled an improved expansion of the distal foraminal area and MFH compared with the PECF group. The facet resection rate in the PECF group was 40.2%±12.6%, and 30.4%±8.6% in the modified-PECF group (Table 2). Both surgical groups showed excellent radiological results of facet joint preservation. However, the modified inclined technique improved facet joint preservation compared to the PECF procedures (facet resection rate, p<0.001) (Table 2).
We analyzed the foraminal expansion and facet resection rates according to the severity of foraminal stenosis, including grades 1 and 2. In the grade 1 foraminal stenosis, there was no significant difference in the expansion ratio of MFD, DFD, and MFH between the 2 groups (expansion ratio of MFD: p=0.94, DFD: p=0.74, MFH: p=0.09) (Table 3). Even in the grade 1 patients, the modified-PECF group showed enhanced facet joint preservation compared with the PECF group (facet resection rate in grade 1, p=0.03) (Table 3). On the other hand, patients with grade 2 foraminal stenosis had the same radiologic outcomes as the overall patients, including MFD, DFD, MFH, and facet resection rate. These results revealed that the modified inclined technique might not benefit from foraminal expansion in patients with grade 1 foraminal stenosis. However, in patients with grade 2 foraminal stenosis, the modified inclined technique offers the advantage of significant foraminal expansion (MFD, DFD, MFH) and improving facet preservation compared to the PECF (Table 3).
The VAS scores for neck and arm pain in both surgical groups significantly improved after the surgery (Table 4). Preoperative neck pain was more severe in the modified-PECF group than in the PECF group (p=0.02) (Table 4). However, neck pain at 1 day and 1 week after surgery was significantly lower in the modified -PECF group than in the PECF group (postoperative: p=0.01, one week: p=0.01) (Table 4); no significant differences were observed after 1-month follow-up. On the other hand, in the arm pain VAS scores, significant differences were not observed between the 2 groups preoperatively, postoperative, at 1-week, 1-month, and 6-month follow-up. Lower arm pain VAS scores were documented in the modified-PECF group at the final follow-up (p=0.02) (Table 4). There was a significant improvement in the NDI scores after the surgery. Although the preoperative NDI score in the modified-PECF group was higher than that in the PECF group (p<0.001) (Table 4), there was no significant difference in the NDI scores between the 2 groups after the surgery (Table 4). The MacNab criteria revealed that both groups had remarkable success rates (PECF, 96%; modified-PECF, 98%; Table 4). In 2 patients who had a fair response in the PECF group, the symptoms of radiculopathy were not resolved after the surgery. Radiologic documents showed insufficient mid foraminal expansion and inadequate facet resection; expansion ratio of MFD: 1.6 and 1.4, expansion ratio of DFD: 0.1 and 0.2; facet resection rate: 23.5% and 4.2 %, respectively, for 2 patients. However, an additional operation for the involved level was not performed during the follow-up.
Postoperative transient neuropraxia can occur through neural manipulation using dissectors, punches, and forceps without neural retraction. In this study, both groups had neuropraxia cases; 4 out of 49 (8%) in the PECF group, and 5 out of 46 (10%) in the modified-PECF group. In the modified-PECF group, 4 patients had finger hypesthesia and only 1 patient experienced transient motor weakness. Otherwise, 2 patients with motor weakness were observed in the PECF group, and 2 hypesthesia occurred through the involved nerve root dermatome, including the fingers. During ventral foraminal decompression with the modified inclined technique, sufficient space was created between the nerve root and distal part of the SAP. At this step, we can remove the distal portion of the SAP more safely and widely without compressing the nerve root, even in grade 2 foraminal stenosis (Fig. 2J). On the other hand, during the usual PECF for grade 2 osseous foraminal stenosis, additional compression to the involved nerve root is inevitable during punching of the distal part of the SAP because the nerve root is severely squeezed between the hypertrophied SAP and prominent bony spur. Additional compression of the vulnerable nerve root may cause motor weakness and a broader area of hypoesthesia. Therefore, during the PECF, excessive facet resection over 75% occasionally occurs for sufficient neural decompression (Fig. 4).
The 1 patient who underwent C4–5 modified-PECF experienced C5 palsy 2 days after the surgery. In this patient, severe osseous foraminal stenosis with prominent bony spur was observed on the preoperative images, and they were sufficiently removed using the modified inclined technique. However, more extensive neural retraction was necessary to remove the uncovertebral hypertrophy, which might cause C5 nerve root palsy (Fig. 4). Therefore, if the C4–5 operation level has severe osseous foraminal stenosis, the modified inclined technique is not recommended; rather, we consider the anterior cervical approach to prevent postoperative C5 palsy.
The overresection of the pedicle and vertebrae can lead to instability. Pediculotomy should be carefully performed only to drill no more than 3–5 mm combined dimension of the pedicle and corpus, which is measured by the 3.0- or 3.5-mm diamond drill. Furthermore, oblique pediculotomy using an inclined surgical approach can reduce the amount of pediculotomy required. This study did not show cases of instability caused by excessive pediculotomy or facet resection.
VAS score for neck pain in the modified-PECF group was lower on 1 day and 1 week after surgery than in another group. There is a possibility that less facet resection and facet capsule preservation were associated with decreased neck pain VAS score within 1 week after surgery. However, after 1-month follow-up, significant differences between the groups disappeared, possibly due to facet joint healing and stabilization.
Whether distal foraminal decompression improves clinical outcomes during the posterior cervical approach for foraminal stenosis treatment remains controversial. Nakamura and Taguchi [17] reported a clinical series in which residual stenosis in the lateral portion of the intervertebral foramen was weakly associated with postoperative outcomes. However, no comparative study has analyzed the association between the degree of distal foraminal decompression and postoperative outcomes. Herein, a significant difference in the arm pain VAS score was not observed between the 2 groups within 6 months after the surgery, despite the modified-PECF group having a higher expansion ratio of the distal foraminal area and foraminal height. At the final follow-up, the modified-PECF group showed significantly improved arm pain compared with the PECF group. The extra space in the distal foraminal area may help maintain the expanded foraminal space. Furthermore, the modified inclined technique influences the contour and course of the nerve root. After SAP base resection, the DRG was decompressed entirely, and the nerve root restored its natural downward angulation (Fig. 1B). Restored nerve root course could also help enhance the postoperative arm pain VAS. However, if the bony spur indented the nerve root, its distorted course of the nerve root may not be restored (Fig. 1A).
In the PECF group, a patient who experienced a relapse of symptoms showed restenosis of the foraminal space outlined by the SAP base and lower-level pedicle on the 1-year MRI. This patient did not undergo pediculotomy, bony spur removal, and foraminal narrowing at the SAP base had not sufficiently expanded. The restenosis may have occurred first at the SAP base area (Fig. 5A–C). However, the modified inclined technique offered sufficient expansion of the SAP base part, and restenosis was not observed in any foraminal area on the 1-year MRI, despite the presence of a prominent bony spur (Fig. 5D–F).
The present study had several limitations. This was a retrospective study, and the follow-up period was relatively short, though it was reasonable for assessing midterm results. A multicenter study with larger sample size and long-term follow-up is required to confirm the findings of this study. We measured the facet joint resection using a linear distance and not the total volume of the resected facet joint. Foraminal diameter expansion was measured at the most stenotic mid-disc level. This did not represent foraminal changes at the SAP base.
Both surgical groups showed excellent facet joint preservation, midforaminal expansion, and favorable midterm clinical outcomes without serious complications. The modified inclined technique has radiologic benefits over the conventional PECF, including enhanced facet joint preservation, natural course restoration of nerve roots, and restenosis prevention by expanding the SAP base of the intervertebral foramen in the grade 2 osseous foraminal stenosis. Furthermore, this technique can improve postoperative neck pain within 1 week after surgery by preserving the facet joint; it may enhance the postoperative arm pain after 6-month follow-up by preventing restenosis.
SUPPLEMENTARY MATERIALS
Supplementary video clip can be found viahttps://doi.org/10.14245/ns.2244268.134.
NOTES
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: JYK, DHH, DCL, CKP; Data curation: JYK, DHH, THK; Formal analysis: JYK, DHH, THK; Funding acquisition: DCL, CKP; Methodology: JYK, DHH, DCL, CKP; Project administration: JYK, DHH, DCL, CKP; Visualization: JYK, DHH, DCL, CKP; Writing - original draft: JYK, DHH, THK; Writing - review & editing: JYK, DHH, DCL
Fig. 1.
Two types of full endoscopic posterior cervical foraminotomy (PECF) for osseous foraminal stenosis. (A) Intraoperative photo and illustration of the PECF. (B) Intraoperative photograph and illustration of the modified-PECF. Skin incision points are different for the 2 types of PECF. (C) On the anteroposterior x-ray image, PECF commonly creates the skin incision on the uncovertebral joint (UVJ) line, and modified-PECF makes the skin incision 1 cm medial to the UVJ line. (D) More medially created skin entry offers the inclined surgical route for undercutting the facet joint. (E) On the lateral x-ray image, the PECF makes the skin incision on the upper endplate line of the involved intervertebral disc; however, the modified-PECF group creates the skin incision on the lower endplate line for a slight cranially directed approach. IPV, inclined pedicular-vertebrotomy.
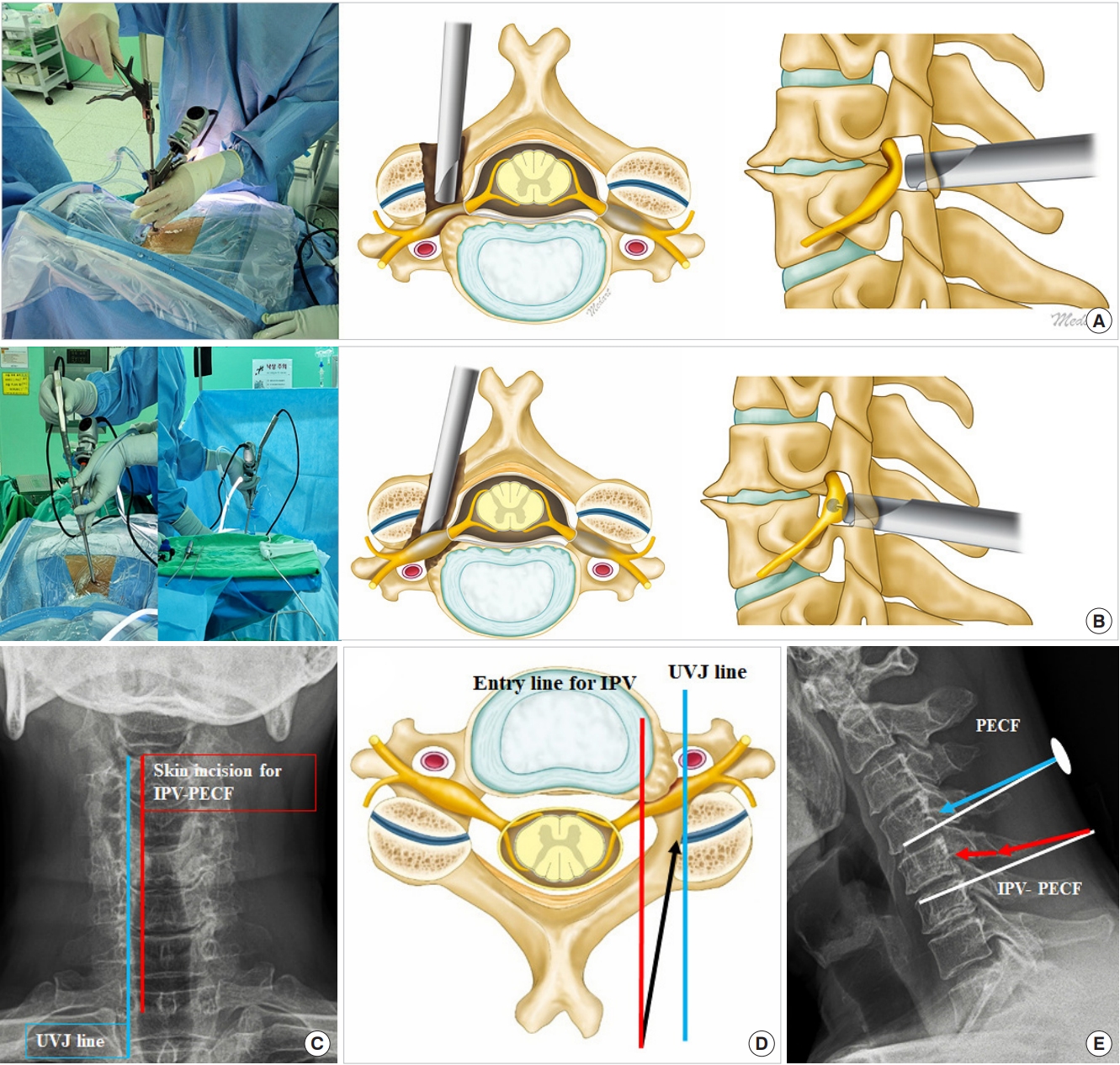
Fig. 2.
Intraoperative endoscopic views of inclined pedicular-vertebrotomy posterior endoscopic cervical foraminotomy at the left C5–6 level. (A) Drilling is initiated from the anatomical V-point (black dotted line). (B) After broad drilling, the superior articular process (SAP) and craniolateral border of the lower-level lamina, contour of the pediculotomy, and distal part of the SAP were exposed. The exiting nerve root can be confirmed through the drilled inner cortical bone (yellow arrowheads). (C) The drilled inner cortical bone was elevated by detaching from the ligamentum flavum (LF) and dura using the dissector. (D) The distal part of the SAP was further resected using the 1-mm punch (white arrowhead). The nerve root was still compressed by the SAP base part at the lateral pedicular area (yellow asterisk). (E) After removing the SAP base and lateral pedicular portions, the decompressed nerve root was observed at the foraminal exiting zone (red asterisk). (F) While protecting the nerve root using a bevel of the working cannula, the bony spur was removed by a 3.0-mm endoscopic diamond drill without violating the intervertebral disc (black arrowhead). (G) The bony spur was sufficiently removed. (H) Inclined pedicular-vertebrotomy (blue asterisk) induced complete neural decompression and restored the nerve root’s natural course. Features of bony removal after modified-PECF are observed on the computed tomography (CT). (I) The severely collapsed intervertebral foramen is remarkably expanded. The bony spur and superior pedicle are obliquely drilled out (red asterisk) to expand the foraminal width and height more. (J) Postoperative 3-dimensional CT images showing surgical route for modified inclined approach (red arrows) and well-preserved facet joint (black asterisk). The modified inclined technique offers a significant expansion of lower foraminal levels (blue arrows). IAP, inferior articular process.
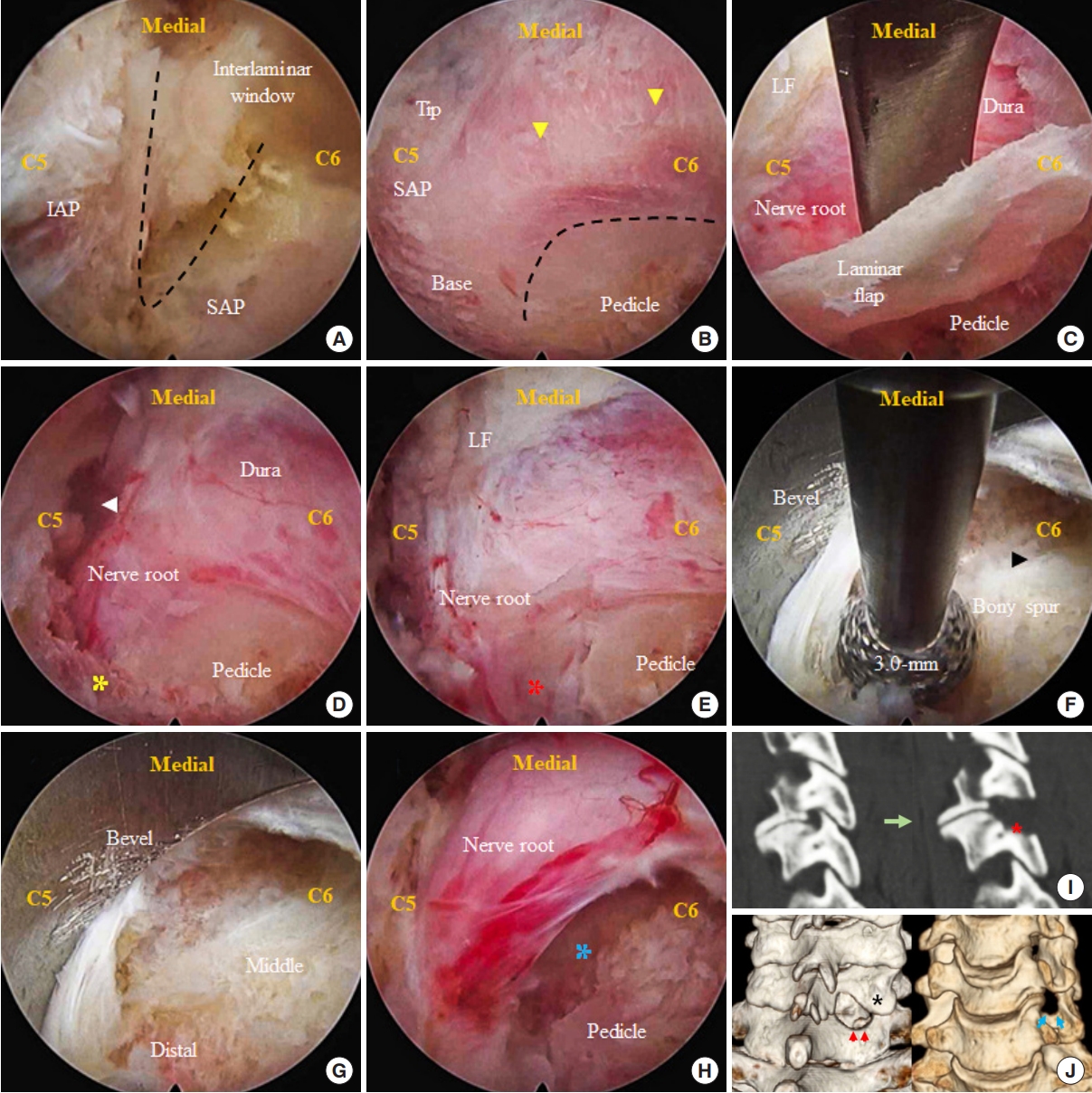
Fig. 3.
Measurement of the parameters on the pre- and postoperative T2-weighted axial magnetic resonance imaging (MRI) from the center of operating intervertebral disc and T2-weighted oblique sagittal MRI from the middle pedicle level. (A, B) Midforaminal diameter (MFD), distal foraminal diameter (DFD), facet joint width (FJW), and mid foraminal height (MFH) were measured on the preoperative MRI. (C, D) After posterior endoscopic cervical foraminotomy (PECF), 4 parameters were measured from the same axial and sagittal cut with preoperative measured level. (E, F) Four parameters were also measured using the same postoperative MRI methods after modified-PECF.
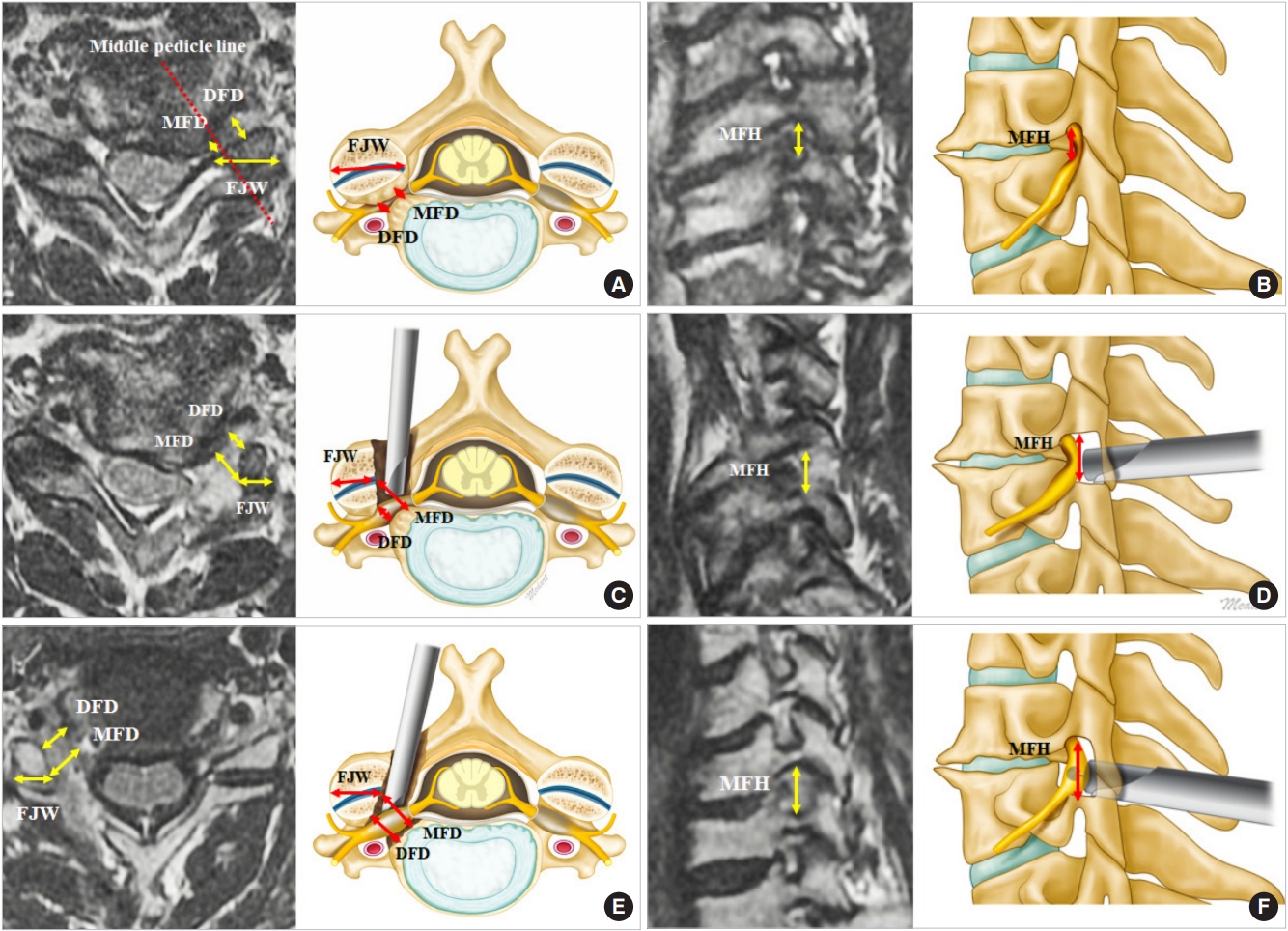
Fig. 4.
Illustrated cases of complications. (A–D) C5 palsy occurred after modified inclined approach for posterior endoscopic cervical foraminotomy (modified-PECF) at the right C4–5 level. (A) Preoperative magnetic resonance imaging (MRI) shows severe osseous foraminal stenosis (yellow arrow). (B) Postoperative MRI presents sufficiently decompressed neuroforamen. Prominent bony spur was adequately removed (white arrow). (C) The nerve root restored its natural downward path after removing the bony spur using a modified inclined technique (blue asterisk). (D–F) Mechanical posterior neck pain relapsed 10 months after the PECF at the left C5–6 level. (D) Preoperative MRI reveals severe foraminal stenosis caused by the prominent bony spur. (E, F) Excessive facet resection (red asterisks) over 75% of resection rate is observed on the postoperative MRI and computed tomography.
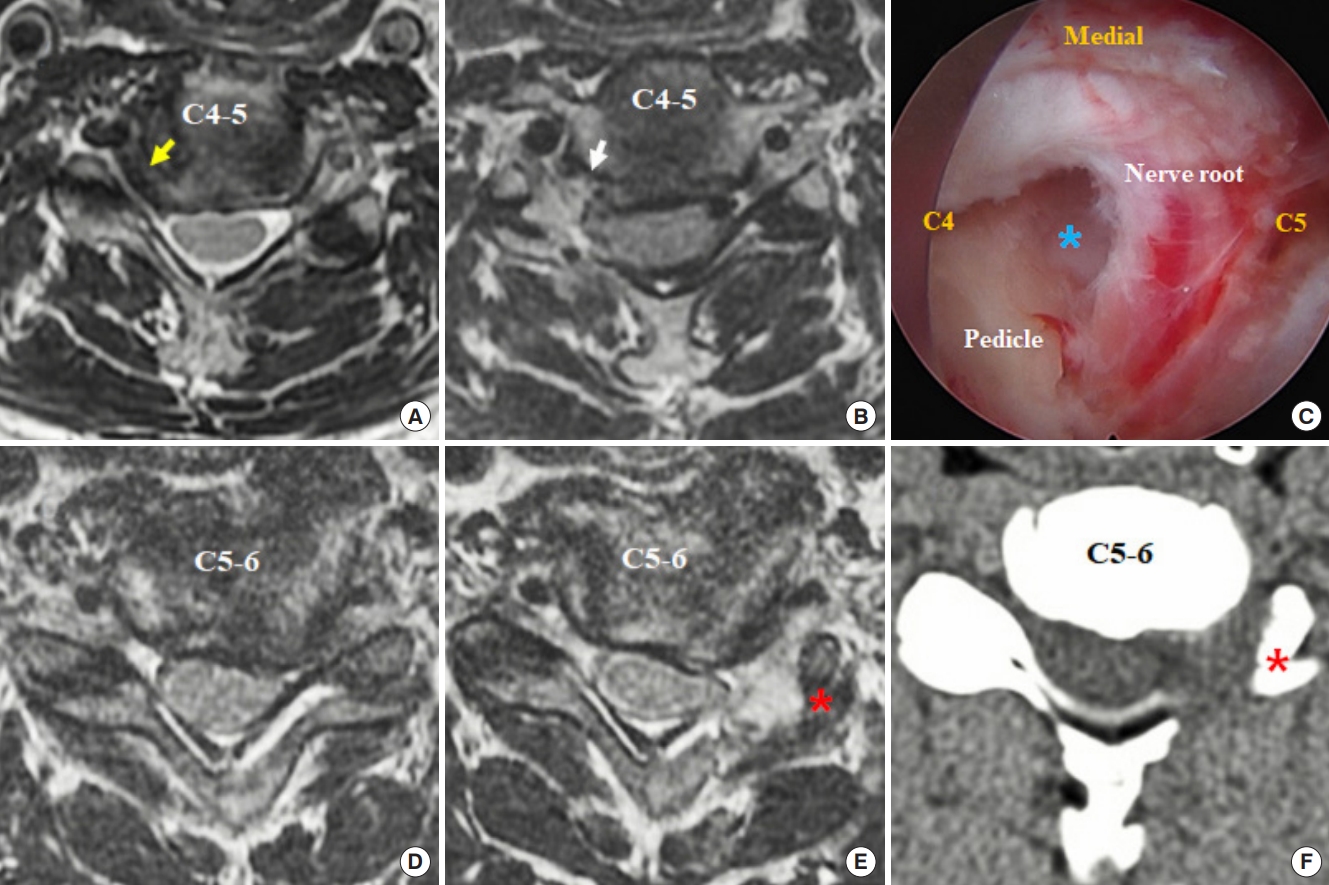
Fig. 5.
Illustrated cases with follow-up magnetic resonance image (MRI) in the 2 surgical groups. (A–C) Symptoms relapsed after performing the posterior endoscopic cervical foraminotomy (PECF). (A) Preoperative T2-weighted oblique sagittal and axial MRI shows osseous foraminal stenosis (red arrow), mainly in the middle and lower foraminal levels. (B) Postoperative MRI reveal sufficient decompression of the middle foraminal level, and the remaining stenosis (blue asterisk) was observed in the lower foraminal level. (C) On the 1-year follow-up MRI, definite restenosis is found in the lower foraminal level (red asterisks), but more minor in the middle foraminal level. (D–F) Follow-up MRI of modified inclined approach for posterior endoscopic cervical foraminotomy (modified-PECF). (D) Preoperative T2-weighted oblique sagittal and axial MRI showing severe osseous foraminal stenosis (red arrow), both in the middle and lower foraminal levels. (E) Postoperative MRI reveals sufficient decompression of the middle and lower foraminal levels and well-preserved facet joint. Partial pediculotomy (blue asterisk) induces the expansion of the lower foraminal level. (F) After 1 year of modified-PECF surgery, restenosis was not observed in any levels of the foramen, and the drilled pedicle is well-preserved without fracture (red asterisk).

Table 1.
Patient information
Table 2.
Radiological outcomes of the foraminal diameter and height
| Parameter |
PECF (n = 49) |
Modified-PECF (n = 46) |
p-value | ||
|---|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | ||
| MFD (mm) | 1.8 ± 0.8 | 7.2 ± 1.7 | 2.0 ± 0.9 | 9.1 ± 2.1 | - |
| DFD (mm) | 2.8 ± 0.8 | 4.2 ± 1.3 | 2.8 ± 1.0 | 5.2 ± 1.4 | - |
| MFH (mm) | 8.9 ± 1.2 | 9.9 ± 1.1 | 7.5 ± 2.0 | 10.1 ± 1.2 | - |
| Foraminal expansion ratio | |||||
| MFD | 4.5 ± 1.9 | 5.4 ± 2.6 | 0.164 | ||
| DFD | 1.6 ± 0.7 | 2.1 ± 1.0 | < 0.001* | ||
| MFH | 1.1 ± 0.1 | 1.5 ± 0.7 | < 0.001* | ||
| Facet joint resection | |||||
| FJW (mm) | 13.6 ± 2.1 | 8.1 ± 2.0 | 13.9 ± 2.4 | 9.6 ± 1.9 | - |
| Facet resection rate (%) | 40.2 ± 12.6 | 30.4 ± 8.6 | < 0.001* | ||
Table 3.
Radiologic outcomes according to the grades of foraminal stenosis
| Foraminal expansion ratio |
Grade 1 |
p-value |
Grade 2 |
p-value | ||
|---|---|---|---|---|---|---|
| PECF (n=13) | Modified-PECF (n=9) | PECF (n=36) | Modified-PECF (n=37) | |||
| MFD | 3.3 ± 1.3 | 3.3 ± 1.1 | 0.94 | 5.0 ± 1.9 | 5.4 ± 2.6 | 0.179 |
| DFD | 1.5 ± 0.3 | 1.7 ± 0.6 | 0.74 | 1.6 ± 0.8 | 2.2 ± 1.1 | 0.002* |
| MFH | 1.1 ± 0.1 | 1.2 ± 0.1 | 0.09 | 1.1 ± 0.1 | 1.6 ± 0.7 | < 0.001* |
| Facet resection rate (%) | 39.3 ± 11.8 | 27.3 ± 6.3 | 0.03* | 40.5 ± 13.0 | 31.2 ± 9.0 | 0.001* |
Table 4.
Clinical outcomes
| Variable | PECF | Modified-PECF | p-value |
|---|---|---|---|
| VAS of neck pain | |||
| Preoperative | 6.7 ± 1.0 | 7.2 ± 0.8 | 0.02* |
| Postoperative | 3.3 ± 0.7 | 2.9 ± 0.6 | 0.01* |
| 1 Week | 2.7 ± 0.9 | 2.3 ± 0.7 | 0.01* |
| 1 Month | 2.2 ± 0.7 | 2.0 ± 0.7 | 0.17 |
| 6 Months | 2.0 ± 0.6 | 1.9 ± 0.6 | 0.69 |
| Final follow-up | 1.9 ± 0.5 | 1.7 ± 0.6 | 0.29 |
| VAS of arm pain | |||
| Preoperative | 7.1 ± 0.8 | 7.3 ± 1.0 | 0.26 |
| Postoperative | 2.4 ± 0.8 | 2.2 ± 0.6 | 0.20 |
| 1 Week | 1.8 ± 0.8 | 1.7 ± 0.8 | 0.38 |
| 1 Month | 1.5 ± 0.6 | 1.3 ± 0.6 | 0.21 |
| 6 Months | 1.3 ± 0.5 | 1.2 ± 0.4 | 0.22 |
| Final follow-up | 1.3 ± 0.5 | 1.1 ± 0.3 | 0.02* |
| NDI | |||
| Preoperative | 23.9 ± 3.9 | 28.7 ± 3.4 | < 0.001* |
| 1 Week | 13.0 ± 2.7 | 14.0 ± 2.8 | 0.11 |
| 1 Month | 9.7 ± 2.5 | 9.5 ± 3.0 | 0.66 |
| 6 Months | 7.4 ± 3.0 | 7.0 ± 2.3 | 0.70 |
| Final follow-up | 5.8 ± 2.6 | 5.7 ± 1.6 | 0.30 |
| MacNab criteria | |||
| Excellent | 6 (12) | 15 (33) | - |
| Good | 41 (84) | 30 (65) | - |
| Fair | 2 (4) | 1 (2) | - |
| Poor | 0 (0) | 0 (0) | - |
| Success rate (good+excellent) | 96% | 98% | - |
REFERENCES
1. Woods BI, Hilibrand AS. Cervical radiculopathy: epidemiology, etiology, diagnosis, and treatment. J Spinal Disord Tech 2015;28:E251-9.

3. Selvanathan SK, Beagrie C, Thomson S, et al. Anterior cervical discectomy and fusion versus posterior cervical foraminotomy in the treatment of brachialgia: the Leeds spinal unit experience (2008-2013). Acta Neurochir (Wien) 2015;157:1595-600.



4. McAnany SJ, Kim JS, Overley SC, et al. A meta-analysis of cervical foraminotomy: open versus minimally-invasive techniques. Spine J 2015;15:849-56.


5. Dodwad SJ, Dodwad SN, Prasarn ML, et al. Posterior cervical foraminotomy: indications, technique, and outcomes. Clin Spine Surg 2016;29:177-85.

7. Ruetten S, Komp M, Merk H, et al. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33:940-8.

8. Zhang C, Wu J, Zheng W, et al. Posterior endoscopic cervical decompression: review and technical note. Neurospine 2020;17(Suppl 1):S74-80.




9. Wu PH, Kim HS, Lee YJ, et al. Posterior endoscopic cervical foramiotomy and discectomy: clinical and radiological computer tomography evaluation on the bony effect of decompression with 2 years follow-up. Eur Spine J 2021;30:534-46.



10. Wu PF, Li YW, Wang B, et al. Posterior cervical foraminotomy via full-endoscopic versus microendoscopic approach for radiculopathy: a systematic review and meta-analysis. Pain Physician 2019;22:41-52.

11. Song KS, Lee CW. The biportal endoscopic posterior cervical inclinatory foraminotomy for cervical radiculopathy: technical report and preliminary results. Neurospine 2020;17(Suppl 1):S145-53.




12. Kim JY, Hong HJ, Lee DC, et al. Comparative analysis of 3 types of minimally invasive posterior cervical foraminotomy for foraminal stenosis, uniportal-, biportal endoscopy, and microsurgery: radiologic and midterm clinical outcomes. Neurospine 2022;19:212-23.




13. Kim HS, Wu PH, Lee YJ, et al. Safe route for cervical approach: partial pediculotomy, partial vertebrotomy approach for posterior endoscopic cervical foraminotomy and discectomy. World Neurosurg 2020;140:e273-82.


14. Ito M, Tadano S, Kaneda K. A biomechanical definition of spinal segmental instability taking personal and disc level differences into account. Spine (Phila Pa 1976) 1993;18:2295-304.


15. Cho JY, Lee SH, Lee HY. Prevention of development of postoperative dysesthesia in transforaminal percutaneous endoscopic lumbar discectomy for intracanalicular lumbar disc herniation: floating retraction technique. Minim Invasive Neurosurg 2011;54:214-8.






























