Demographic Trends in Paddle Lead Spinal Cord Stimulator Placement: Private Insurance and Medicare Beneficiaries
Article information
Abstract
Objective
Although spinal cord stimulators (SCS) continue to gain acceptance as a viable nonpharmacologic option for the treatment of chronic back pain, recent trends are not well established. The aim of this study was to evaluate recent overall demographic and regional trends in paddle lead SCS placement and to determine if differences in trends exist between private-payer and Medicare beneficiaries.
Methods
A retrospective review of Medicare and private-payer insurance records from 2007–2014 was performed to identify patients who underwent a primary paddle lead SCS placement via a laminectomy (CPT-63655). Each study cohort was queried to determine the annual rate of SCS placements and demographic characteristics. Yearly SCS implantation rates within the study cohorts were adjusted per 100,000 beneficiaries. A chi-square analysis was used to compare changes in annual rates.
Results
A total of 31,352 Medicare and 2,935 private-payer patients were identified from 2007 to 2014. Paddle lead SCS placements ranged from 5.9 to 17.5 (p < 0.001), 1.9 to 5.9 (p < 0.001), and 5.2 to 14.5 (p < 0.001) placements per 100,000 Medicare, private-payer, and overall beneficiaries respectively from 2007 to 2014. SCS placements peaked in 2013 with 19.6, 7.1, and 16.8 placements per 100,000 Medicare, private-payer, and overall patients.
Conclusion
There was an overall increase in the annual rate of SCS placements from 2007 to 2014. Paddle lead SCS placements peaked in 2013 for Medicare, private-payer, and overall beneficiaries. The highest incidence of implantation was in the Southern region of the United States and among females. Yearly adjusted rates of SCSs were higher among Medicare patients at all time points.
INTRODUCTION
Since its introduction by Shealy et al in 1967, spinal cord stimulators (SCS) have gained a wide range of application amongst a number of medical specialties for neuropathic pain alleviation [1,2]. The recent intersection between the health and economic burden of chronic back pain and the ongoing opioid epidemic has heightened the need for safer alternatives to treat chronic back pain [3,4]. SCSs continue to gain acceptance amongst spine surgeons as a nonpharmacologic treatment option to address chronic back pain from failed back surgery syndrome and other pain pathologies such as complex regional pain syndrome (CRPS), where conservative medical management (CMM) therapies have failed. In a number of randomized controlled trials, SCSs have been shown to be more effective in the treatment of chronic pain in spine patients compared to CMM or reoperation [5-7]. With the rising popularity of SCSs, the role insurance providers’ play in utilization has begun to garner attention. Private-payers have shown to have lower overall costs following implantation while simultaneously less likely to receive SCS coverage approval when compared to their public counterparts [8,9]. However, to date, one has explored what effect these differences in providers have on annual incidence of SCS.
Presently, SCS placement is performed either percutaneously with cylindrical leads or with paddle lead placement via a laminectomy. Although previous studies have reported on the trends of SCS use, most are outdated and there is a lack of consensus amongst these studies [10-12]. The aim of this study was to evaluate recent overall demographic and regional trends in paddle lead SCS implantation. Additionally, given the disparity of post-SCS cost-effectiveness and coverage among insurance providers, the study will examine if differences in annual trends exist between private-payer and Medicare beneficiaries.
MATERIALS AND METHODS
1. Data Source
A retrospective database review was conducted, utilizing the commercially available PearlDiver Patient Records Database (www.pearldiverinc.com; PearlDiver Inc., Colorado Springs, CO, USA), which contains Medicare (2005–2014) and privatepayer insurance (Humana, 2007–2016) patient records, searchable by billable codes. All queried data are de-identified and Health Insurance Portability and Accountability Act compliant. As such, this study was exempt from Institutional Review Board approval.
2. Study Population
Our study includes all Medicare and private-payer patients suffering from neuropathic related pain who underwent a primary paddle lead SCS placement via a laminectomy (CPT-63655) from 2007 to 2014. Only primary paddle lead SCS placements were included in this study. Percutaneous cylindrical lead placements were not included because coding does not differentiate between trial and permanent cylindrical lead placement. Furthermore, International Classification of Diseases, Ninth Revision diagnosis codes were used to exclude patients with a history of spine infection, trauma, or a primary malignancy or metastasis of the spine.
3. Trends in SCS Placement
Each database was queried separately to identify patients in the Medicare and private-payer cohorts. Each cohort was further queried to determine the number of SCS placements and to calculate annual rates. Data were then pooled to provide overall assessment of the population. A breakdown of demographic parameters, including total number of patients, age, region, and gender was also performed. As the private-payer database permits the query of race and physician specialty information, these additional parameters were included in the private-payer cohort.
4. Data Analysis
The frequency of SCS placement amongst different demographic parameters including age range (less than 65, 65–84, and greater than 85 years), female sex, and region was determined in each cohort. Additionally, frequency of SCS placements was determined for race and physician specialty within the private-payer cohort. Annual rates of SCS placements within both study cohorts were adjusted per 100,000 beneficiaries. A chi-square analysis was used to compare changes in annual rates, with significance set at p < 0.05.
RESULTS
1. Patient Demographics
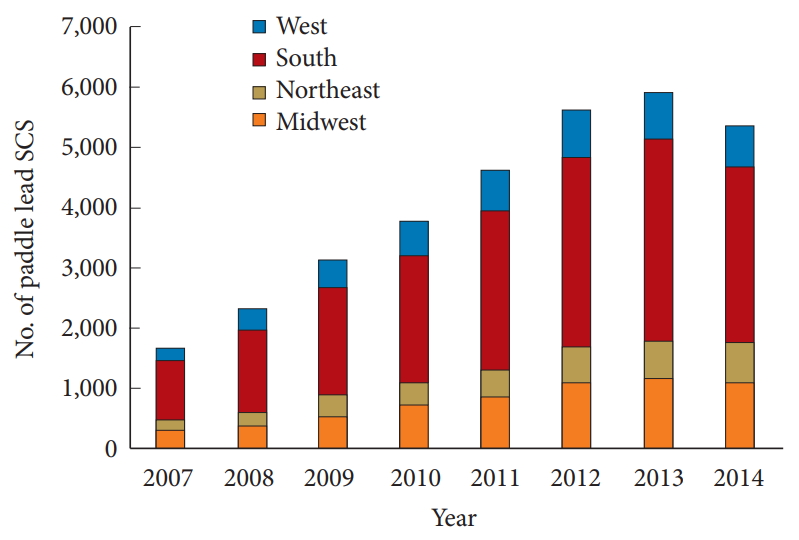
In total, 34,287 paddle lead SCS placements were identified in the Medicare (n= 31,352) and private-payer (n= 2,935) insurance databases from 2007 to 2014 (Fig. 1). Incidence of overall SCS placement was highest in ages 65–84 years (54.0%) amongst Medicare beneficiaries and all providers (52.9%) while SCS placement rates were highest in patients < 65 years old (56.8%) amongst private-payers. SCSs were placed in greater proportions in women (59.3% Medicare vs. 57.1% private-payer vs. 59.1% all providers). The highest incidence of SCS placement was in the Southern United States (US) region (55.6% Medicare vs. 67.0% private-payer vs. 56.6% all providers) and lowest in the Northeastern US region (11.4% Medicare vs. 2.4% privatepayer vs. 10.6% all providers). Further query of the private-payer database showed that the proportion of SCS placement was highest amongst white patients (79.6%) and high proportions of SCS placements were performed by general acute care hospital specialist (29.4%), neurological surgeons (28.1%), orthopaedic spine surgeons (16.0%), and neurologists (12.6%) (Table 1).
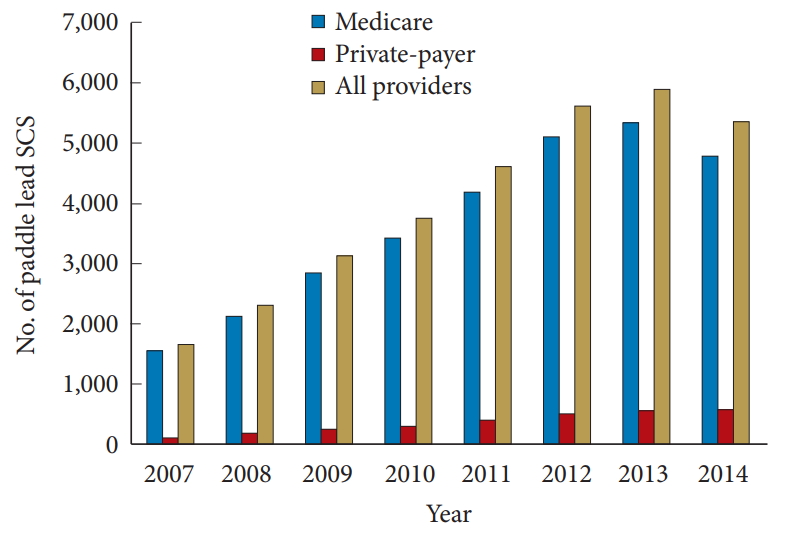
Total number of paddle lead spinal cord stimulators (SCS) among insurance providers from 2007 to 2014.
2. Trends in SCS Placement
SCS placements ranged from 5.9 to 17.5 (p < 0.001), 1.9 to 5.9 (p < 0.001), and 5.2 to 14.5 (p < 0.001) placements per 100,000 Medicare, private-payer, and overall beneficiaries respectively from 2007 to 2014 (Fig. 2). SCS placements peaked in 2013 with 19.6, 7.1, and 16.8 placements per 100,000 Medicare, private-payer, and overall patients (Fig. 1). Our analysis showed a significant increase in annual rate of SCS placement within the Midwest (p < 0.001) and Northeast (p < 0.001) regions amongst Medicare beneficiaries and the Midwest (p < 0.001), Northeast (p = 0.008), and Southern (p < 0.001) US regions amongst private-payer beneficiaries (Table 2). Among all providers, increases in annual rates were seen in the Midwest (p < 0.001), Northeast (p = 0.001), South (p < 0.001), and West regions (p = 0.012) (Fig. 3). There was a significant increase in the annual rate of SCS placements in women (p < 0.05) in all cohorts.
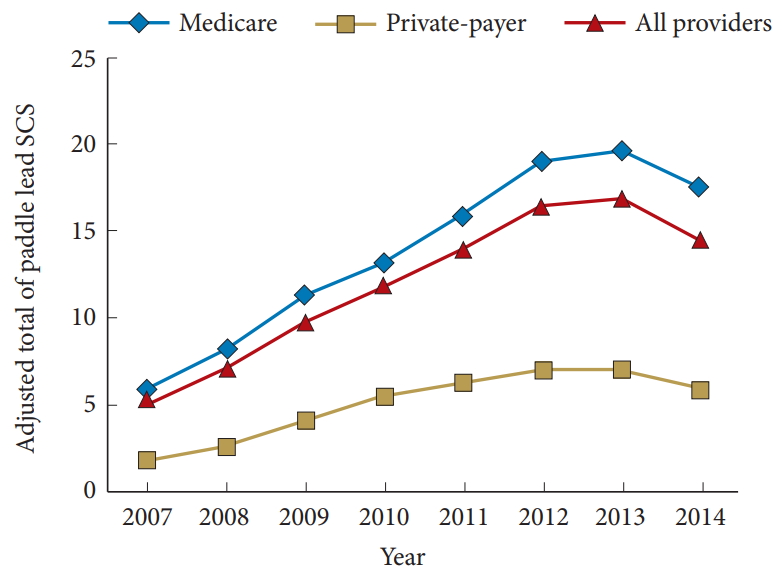
Comparison of adjusted total of paddle lead spinal cord stimulators (SCS) per 100,000 beneficiaries from 2007 to 2014.
DISCUSSION
Current pain literature supports the use of SCSs compared to other treatment options such as CMM; nonetheless, there is a lack of data on the recent trends of SCS placements [5-7]. Using 2 separate insurance databases, our results show that SCS placements increased significantly over an 8-year period, peaking in 2013. The highest incidence of implantation was amongst women and in the Southern region of the US. Adjusted total were lower among private-payers at all time intervals compared to Medicare patients.
SCS trends have been reported in a similar study by Lad et al. [10] using the National Inpatient Sample database. This study demonstrated that SCS placement was relatively stable over 14 years from 1993 to 2006, findings that contrast with results of the present study. Furthermore, a survey of 50 institutions by Gharibo et al. demonstrated a 262% increase in SCS implantation in 2012 compared to a previous survey of pain medicine fellowship programs in 1999 [11,13]. While adjusted annual rates of both the private-payer and Medicare groups increased the 8-year period among, there was a noticeable disparity between the cohorts. Within all time intervals adjusted annual rates of paddle lead SCS among Medicare patients were greater than those among private-payers. Prior studies among differing surgical specialties have demonstrated that insurance status can be predictive of choice of surgical technique [14,15]. Elsamadicy et al. [8] demonstrated that overall cost-effectiveness of SCS was decreased among Medicare patients compared to private-payers, however, drew no association to utilization trends. However, this would be expected drive rates of SCS down in the Medicare population, the opposite of this study’s observation. One potential source of disparity could be that Medicare patients are traditionally older patients who present at advanced stages of disease with high comorbidity burden and thus may be perceived as more optimal candidates for conservative and cost effective measures, such as SCS [16,17]. Interestingly, Heyward et al. [9], demonstrated than private-payer were less likely to receive coverage for SCS implantation for the management of low back pain when compared to patients covered by public providers. Coverage propensity may be an additional driving force behind the greater disproportion of Medicare paddle lead SCS utilization.
The demographic makeup of SCS patients was another area of interest in this study. Our results show that SCSs are predominantly implanted in white female patients within both insurance providers. This finding is consistent with other studies in the literature. In a study of 4,536 patients undergoing paddle lead SCS for the treatment of chronic pain, Babu et al. [18] reported that 60.3% of SCS placements were performed in women. Likewise, Geurts et al. [19] also reported that their SCS placement population was 74% women in a study assessing the effectiveness of SCSs in the treatment of CRPS type 1. Lad et al. [10] further reported that a majority of SCS placements occurred in patients between the ages of 45–64 years, with the fewest placements occurring in patients > 85 years. We report similar findings in our private-payer population, as 56.8% of SCS placements occurred in patients younger than 65 years, while the lowest percentage of SCS placement in all cohorts occurred in patients > 85 years.
A regional analysis of SCS placement by Lad et al. [10] further supports our finding that the most popular region of implantation was the Southern region of the US. The Southern region of the Unites States represents the largest population among the private-payer and Medicare databases. Similarly, prior studies have associated this region with the highest incidence of reported back pain and degenerative spinal conditions [20,21]. The observed increased incidence of paddle lead SCS in this region is indicative of the overall large population of patients with degenerative spinal conditions. As expected, almost all regions saw significant annual increases over the observed 8 years reflecting the rising popularity and utilization of SCSs. However, private-payers within the West region did not see significant growth over the study period possibly reflecting lack of regional adoptance of this technique. Amongst SCS private-payers, patients aged < 65 were the majority, compared to patients aged 65–85 among all providers, and may be regionally viewed as less-likely candidates in the West compared to other regions. This would account for why, overall, the region saw growth while private-payers did not. Interestingly, the western region had been shown to have some of the highest odds (odds ratio, 1.57) of prescribing narcotics for back pain managing and could represent a different regional paradigm in the management of back pain [21].
As the popularity of SCS continues to increase, so has the diversity of physician and specialist who perform the procedure. The private-payer insurance database demonstrated that a majority of SCS placements were performed by general acute care hospital specialists, neurological surgeons, orthopaedic surgeons or neurologists. Hussaini et al. [22] demonstrated that 62.2% of SCS placements were by pain medicine specialist or anesthesiologist, while 22.0% were by neurosurgeons, 10.2% by orthopaedic spine surgeons, and 5.3% by physical medicine and rehabilitation physicians. Hussaini et al. [22] further showed that SCS trial-to-conversion rate was highest amongst orthopaedic spine and neurological surgeons.
The primary advantage of our study compared to prior literature is the utilization of 2 independent health insurance patient populations to establish the trend of SCS placements over an 8-year period. This enabled us to establish an overall increase in SCS placements, with a decline in the last year queried. Also, the inclusion of data from both private-payer and Medicare databases leads to a more accurate representation of the general US population undergoing SCS placement. Furthermore, our study addresses the paucity of data on recent trends of SCSs. To our knowledge, the only similar study on SCS trends was published about a decade ago [10]. Nonetheless, our study has a number of limitations. We only included data from paddle lead SCS placement with laminectomy, and not percutaneous cylindrical lead implantation. As such, our findings pertain to paddle lead SCS placement only and cannot be generalized to the full population. Additionally, as a retrospective database study, accuracy of our results is affected by inaccuracies in coding. Instances of miscoding and non-coding of diagnoses have been identified previously in national databases and could be potential sources of error [23].
CONCLUSION
As the popularity of SCSs in the treatment of chronic neuropathic pain increases, so is the need for insight on the current trends of its utilization. There was an overall increase in the annual rate of SCS placement from 2007 to 2014. SCS placements peaked in 2013 within Medicare and private-payer beneficiaries. Yearly adjusted rates of SCSs were higher among Medicare patients at all time points. The highest incidence of implantation occurred in the Southern region of US. Among private-payers the majority of implantations were performed by general acute care hospital specialists, neurological surgeons, orthopaedic spine surgeons, and neurologists.
Notes
The authors have nothing to disclose.