The Biportal Endoscopic Posterior Cervical Inclinatory Foraminotomy for Cervical Radiculopathy: Technical Report and Preliminary Results
Article information
Abstract
The purpose of the current study was to introduce a surgical technique for posterior cervical inclinatory foraminotomy (PCIF) using a percutaneous biportal endoscopic (BE) approach. Consecutive 7 patients underwent BE-PCIF for their cervical radiculopathy. Postoperative radiologic images (x-rays, computed tomography [CT], and magnetic resonance imaging [MRI]) were evaluated postoperatively for optimal neural decompression status and stability. A visual analogue scale (VAS) for the arm pain and the Neck Disability Index were used to evaluate clinical results in the preoperative and postoperative periods. Mean follow-up periods were 6.42 ± 2.99 months. The mean operative time was 101.42 ± 49.30 minutes. Postoperative MRI and CT revealed complete removal of herniated discs and ideal neural decompression of the treated segments in all patients. Disc height and stability were preserved on postoperative x-rays. Preoperative VAS and Oswestry Disability Index scores improved significantly after the surgery. BE-PCIF may be an effective surgical treatment of the cervical radiculopathic lesions, which provides successful surgical decompression as far as distal part of foramen with better operative view and more easy surgical manipulation. This approach may also minimize iatrogenic damages of the posterior cervical musculo-ligamentous structures and help to maximize the preservation of the facet joint.
INTRODUCTION
There are various surgical options to treat the pathologies that cause cervical radiculopathy. posterior cervical foraminotomy (PCF) has evolved continuously and its favorable clinical results were proved by many studies since Spurling and Scoville [1] reported the methods of posterolateral approach for cervical radiculopathy. PCF has several advantages compared to anterior approach, such as the ability to avoid damage of the anterior vital structures and graft problem without the loss of motion segment [1-6].
However, some concerns with PCF also exist, such as degeneration with kyphosis at the operated-level secondary to partial resection of the facet joint and persistent neck and shoulder pain caused by muscle stripping and injury of the ligamentous structures with the open procedure [7-9].
Several minimally invasive PCF techniques using a tubular system and endoscope were developed to decrease the postoperative neck pain due to iatrogenic muscle injury [6,10-12]. Recently, biportal endoscopic (BE) spine surgery was introduced and its clinical efficacy was also reported by several authors [13].
Chang et al. [14] introduced posterior cervical inclinatory foraminotomy (PCIF), which suggested a method to minimize the facet resection an prevent postoperative instability.
We attempted inclinatory cervical foraminotomy by applying BE spine surgery technique to treat cervical radiculopathic pathologies.
The purpose of the present study was to introduce the surgical technique of BE-PCIF and present preliminary clinical and radiologic results. As far as we know, this is the first report to describe the endoscopic PCIF technique.
MATERIALS AND METHODS
The new procedure was explained to the patients in detail, and all patients provided informed consent.
1. Patients
Seven patients underwent BE-PCIF with/without discectomy for their cervical radiculopathy between June 2019 and February 2020. Pre- and postoperative radiologic images (x-ray, computed tomography [CT], and magnetic resonance imaging [MRI]) were taken and compared. Postoperative MRI and CT were evaluated on the second day after operation for the confirmation of adequate neural decompression. X-rays were also examined at last follow-up to investigate the change of disc height, cervical sagittal alignment and the dynamic angle at operated level [15]. Demographic characteristics, classification of pathologies, distribution of operation level, operative time, and surgical complications were reviewed. Clinical results were evaluated and compared preoperatively and postoperatively using a visual analogue scale (VAS) for arm pain and the Neck Disability Index (NDI) [16]. Statistical calculations, including means and standard deviations, were obtained using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). Paired t-tests were used to compare the differences in each parameter of the perioperative outcome. Statistical significance was established at a p-value of less.
2. Indication, Inclusion, and Exclusion Criteria
BE-PCIF was indicated in the patients with cervical radiculopathy due to foraminal stenosis with or without paracentral or foraminal disc protrusion. The exclusion criteria were the presence of segmental instability, severe kyphosis, central stenosis, ossification posterior longitudinal ligament, myelopathy, and patients with associated infection, tumor, and fracture in the region of the spinal segment.
3. Preoperative Evaluation
Patients were routinely evaluated with anteroposterior, lateral, oblique, and dynamic x-rays to assess spine alignment, disc space height, foraminal bony encroachment, and instability. Additional radiographic evaluations such as MRI and CT were taken to evaluate the degree of foraminal stenosis and acquire detailed information about the facet joint such as degree of joint hypertrophy, tropism, size, and shape of bony spur and inclination angle of the spinous process. This allowed the surgeon to determine the amount of the facet joint resection and approach angle for ideal decompression with the preservation of segmental stability.
4. Surgical Technique
1) Equipments used in BE-PCIF
During the operation, we used a 4-mm solid egg diamond burr (CNS Medical Co., Inc., Pocheon, Korea), 5-mm shaver (Striker Corp., Kalamazoo, MI, USA), 3.5-mm bendable diamond burr (All care, Seoul, Korea) and 0° 4.0-mm-diameter arthroscope (Striker, Corp.). Ninety degrees 3.75-mm radiofrequency ablator (VAPR, DePuy Mitec, Warsaw, IN, USA) and 30° 1.4-mm microablator radiofrequency probe (DePuy, Raynham, MA, USA) were used to control intraoperative bleeding. We also used standard foraminotomy instruments such as serial dilator, Kerrison punches (1, 2 mm), 1.5-mm pituitary forceps (standard and up-bite), and variable small angled chisels and curettes (Fig. 1).
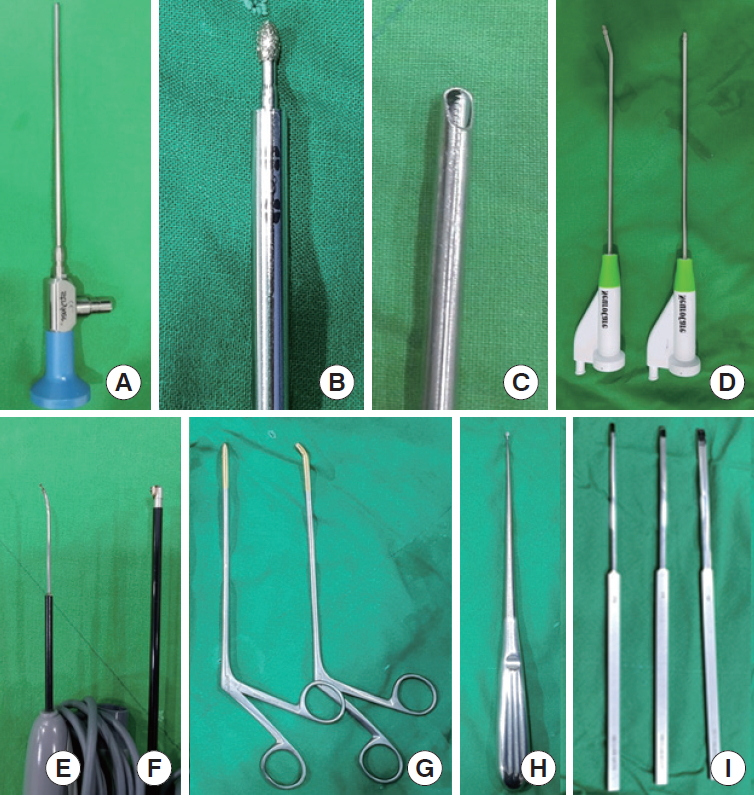
The equipments were used in biportal endoscopic posterior cervical inclinatory foraminotomy. 0° 4-mm diameter arthroscope (A), 4-mm diameter solid egg diamond burr (B), 5-mm diameter shaver (C), 3.5-mm diameter bendable diamond burr (D), 3.75-mm radiofrequency ablator (E), 30° 1.4-mm microablator radiofrequency probe (F), 1.5-mm pituitary forceps straight and up-bite (G), 1-mm curette (H), Chisels 2, 3, 4-mm (curved) (I).
2) Surgical procedure
The operation was performed in a prone position under general anesthesia. The abdomen was relaxed using an H-shape pillow to avoid increased abdominal pressure. A gel-type facial pad was used to protect the face and eyeballs from direct high contact pressure. The neck was flexed and upper back was slanted down to reduce the chance of intraoperative bleeding by good venous return. A cervical traction device was not used. The patient’s head was fixed and both shoulders were pulled by plasters (Fig. 2).

Patient’s operative position. Neck and bilateral shoulders were fixed with plaster without headrest. The upper back was slanted down.
The entire posterior neck is prepared with an antiseptic solution and draped. The surgeon stands on the opposite side of the lesion. For making 2 portals, under the guidance of C-arm fluoroscopy, 2 skin incisions of 0.5 cm long were made vertically along lateral margin of the spinous process. The first skin incision for a cranial portal was made at the level of the upper cervical spinous process related to the target while the other skin incision for a caudal portal was made at the level of lower cervical spinous process. The distance between these 2 portals was about 2 cm (Fig. 3).

The skin entry points for 2 portals and needle targeting. (A) Two skin incisions for 2 portals (red dot, endoscopic view portal; blue dot, working portal for instruments) were illustrated on x-ray anteroposterior (AP) images. Needle targeting toward V-point (green dot) to determine 2 skin entry points and approach angle is shown by C-arm AP/lateral images (B, C). Red line, midline; yellow line, medial pedicular line.
Serial dilators were used to dissect the neck muscle and acquire operative space. A 0° endoscope (Striker) was inserted through the cranial portal after inserting the cannula. A saline irrigation system was applied with a natural drainage system (2 m high from operation room floor). Surgical instruments were inserted through the caudal working portal. After triangulation with the endoscope and instrument on the margin of the superior laminar, inferior laminar, and medial point of the facet joint (V-point) (Fig. 4), minor bleeding was controlled with a radiofrequency probe.
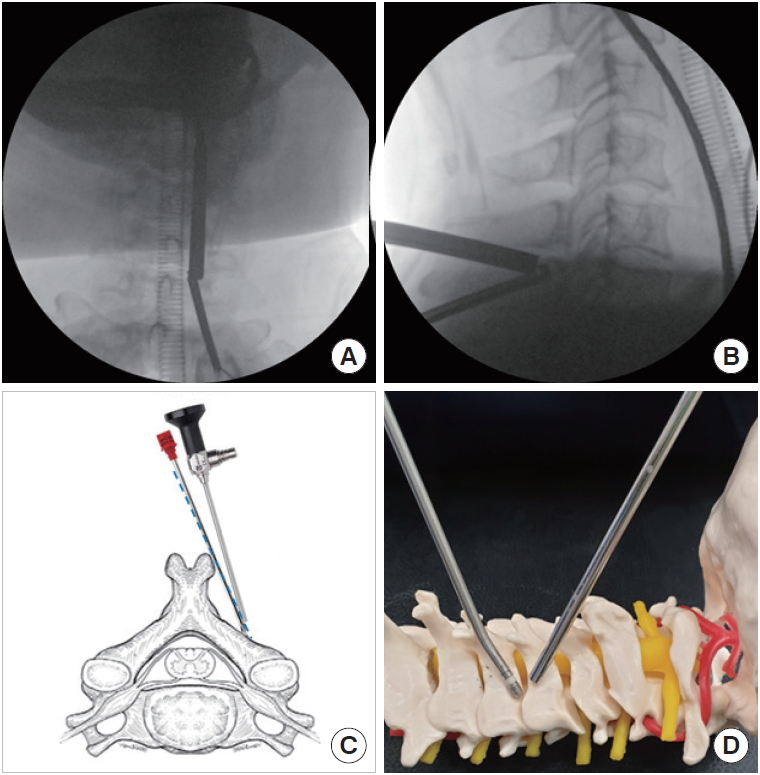
Triangulation with endoscope and instruments. Triangulation of endoscope and instruments is done at docking point (V-point) under the C-arm anteroposterior/lateral views (A, B). (C) Inclinatory operative trajectory (blue dot line) is illustrated schematically with endoscope and instrument. (D) Triangulation of scope and instrument is simulated on the artificial cervical spine model.
After identifying V-point, the inferolateral portion of the upper lamina, superolateral part of the lower lamina and medial point of the facet joint (V-point) was drilled out with endoscopic drills (Supplementary video clip 1). The ligament flavum was preserved to protect the neural structure during drilling for laminotomy. Drilling around the V-point was continued till the caudocranial margin of ligament flavum was exposed. The operator could assume the shape of the root through a thin layer at the lateral margin of ligamentum flavum. The boundary of decompression was extended to the further lateral part of the foramen by using a bendable 3.5-mm diamond burr (Supplementary video clip 2). After circumferential drilling along the pathway of the root, additional decompression for the distal portion of root with the 1-mm Kerrison’s punches and small curettes was followed.
In the case which needs more wide decompression of distal root, the cranial tip of the superior articular process (SAP) was also removed by using 2-mm punches or small chisel (Supplementary video clip 3).
After sufficient bony decompression, ligament flavum was removed by piecemeal in the direction of root from the thecal sac. Bleeding control was performed while removing the ligament flavum. Immediate hemostasis around root origin was done by using the small radiofrequency ablator because venous plexus is abundant around root origin area and sometimes, it makes troublesome intraoperative bleeding (Supplementary video clip 4). Such beforehand or immediate bleeding control was imperative to preserve a clear operative view.
Sufficient foraminal decompression was verified by passing a ball tip probe through the foraminal canal without any resistance. Free nerve root was revealed by gentle manipulation (Supplementary video clip 5) (Fig. 5).
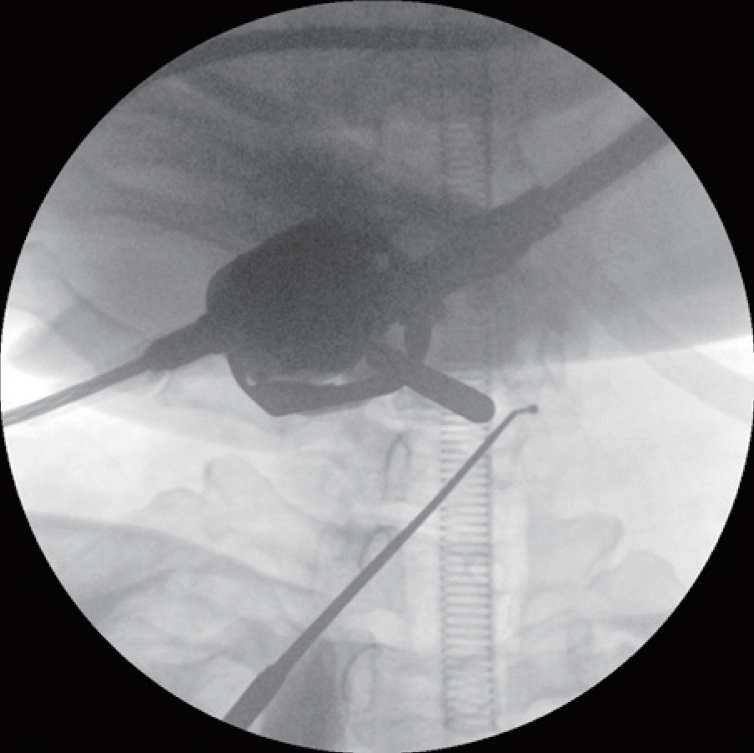
Sufficient decompression in the foraminal area is verified by passing ball probe through the foraminal canal.
Discectomy was conducted by using the hook and the pituitary forceps after adequate decompressive work and perineural adhesiolysis, Scope retractor was used to acquire enough space for discectomy with the root protection (Supplementary video clip 6). In cases of very narrow operative space in axilla region of root, additional pediculotomy was performed before root manipulation for discectomy.
After checking complete decompression by dura pulsation, meticulous hemostasis was done. The wound was closed with subcutaneous suture and skin tape. After surgery, patients are advised to wear a neck collar for a week.
RESULTS
A total of 7 patients (3 men and 4 women; mean age, 59 ± 12.1 years) were enrolled in this study. A total of eleven levels were operated using the aforementioned BE-PCIF. Of these, there were 3 levels of cervical disc herniation and 8 levels of pure foraminal stenosis. The mean hospital day was 5.71 ± 3.86 days, and the mean operation time was 101.42 ± 49.30 minutes (64.54 ± 15.40 minutes/level). The mean follow-up period was 6.42 ± 2.99 months (Table 1). Postoperative MRI and CT scans depicted successfully removed disc herniation and optimal neural decompression of the treated segments in all patients (Figs. 6-8). Significant postoperative change of cervical sagittal alignment or segmental dynamic angle was not seen at the follow-up period. Mean preoperative and postoperative disc space heights were 5.41 ± 1.03 mm and 5.2 ± 1.04 mm. Disc height was relatively preserved steadily over this time during the follow-up period. Preoperative and postoperative radiologic features at the treated level are shown in Table 2. Preoperative VAS and NDI scores were improved significantly after the surgeries: VAS score changed from 7.71 ± 0.75 preoperatively to 0.85 ± 0.69 at the last follow-up visit, while NDI score changed from 60.85 ± 26.85 to 10.57 ± 5.74 (p < 0.05). Dura tear occurred in 1 case and was treated with a gelfoam and TachoSil fibrin sealant patch (Baxter Healthcare Corporation, Deerfield, IL, USA). The tear did not produce cerebrospinal fluid leak or any postoperative negative consequences. There was no case of significant complications after the surgery such as dysthesia, motor weakness, and postoperative hematoma (Table 3).
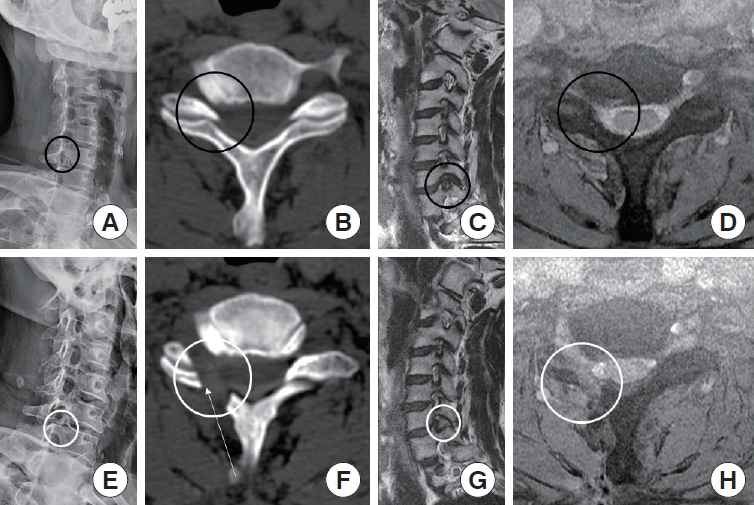
Pre-and postoperative radiologic images of the 4th case. A 67-year-old man presented with right shoulder and arm pain on right C7 dermatomal distribution, paresthesia, and weakness of elbow extension. He underwent biportal endoscopic posterior cervical inclinatory foraminotomy on the C6–7 level right side. Preoperative images showed foraminal stenosis at right side of C6–7 level (A-D), ideal foraminal decompression with obliquely undercut facet joint was shown in postoperative images (E-H). Black circles, compressed areas of right C7 root by C6-7 foraminal stenosis; white circles, enlarged right C6–7 foramen after the operation; white arrow, inclinatory operative trajectory and medial surface of resected facet joint.

Pre- and postoperative radiologic images of the 7th case. A 62-year-old woman presented with bilateral shoulder and arm pain on C6 and right C7 dermatome. She underwent biportal endoscopic posterior cervical inclinatory foraminotomy on C5–6, C6–7 level right side, and C5–6 level left side with switching technique [25]. (A-C) Preoperative images showed foraminal stenosis on bilateral side C5–6 level and right side of C6–7 level (black circles). (D-F) Ideal bilateral foraminal decompression with obliquely undercut facet joint was shown in postoperative images (white circles). (G) A 3-dimensional computed tomography scan identified the remained facet joints and the range and adequacy of foraminotomy.
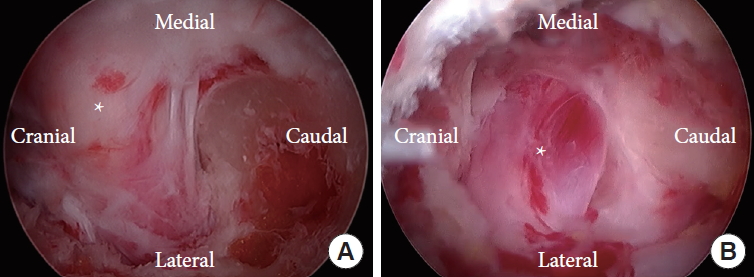
Comparison of operative view between traditional posterior cervical foraminotomy (PCF) and biportal endoscopic posterior cervical inclinatory foraminotomy (BE-PCIF). (A) In traditional PCF, direct unroofing by the removal of dorsal part of facet joint was performed to get sufficient decompression to the distal part of the root. (B) The undercut dome-shaped foramen was shown above the root after the distal root decompression by BE-PCIF. Asterisk means root.
DISCUSSION
Cervical radiculopathy is a common disease that leads to significant disability from nerve root dysfunction. Anterior cervical approach including anterior cervical discectomy and fusion (ACDF) and cervical artificial disc replacement has been considered as the gold standard treatment for cervical radiculopathy. However, the morbidity of anterior cervical surgery ranges from 13.2% to 19.3% [17-19]. Unfavorable postoperative complications such as pseudoarthrosis and adjacent segment disease have been reported [20].
Posterior cervical foraminotomy (PCF) gained popularity as an alternative to ACDF, sparing problems associated with fusion and surgical instrumentations. Compared to the anterior cervical approach, the posterior cervical approach technique has significant advantages, such as no vital organ damage in the anterior neck, preservation of a cervical range of motion, and no complications caused by a bone graft [2,6,11,21-23].
Despite these advantages, postoperative neck pain was the most common complication to be overcome in posterior cervical surgery [1-5]. The preservation of the posterior neck muscles and ligamentous structures is crucial to prevent postoperative instability and axial neck pain. Some authors reported relative advantages of posterior endoscopic cervical discectomy and foraminotomy to minimize iatrogenic injury of the posterior cervical structures and achieve similar goals of conventional PCF without significant complications [12].
In our series, BE-PCIF had achieved good clinical and radiological outcomes. The BE spine surgery system, which was used in these series, led to favorable clinical outcomes and high satisfaction by patients due to its minimal invasiveness. All patients have improved neck pain, VAS and NDI were satisfied with less postoperative neck pain, minimal operative scar, short hospital stay, and early return to previous routine work. Such advantages in endoscopic spinal surgery were reported previously [17] and also confirmed in current cases.
Common surgical failure in PCF is persistent pain due to remnant disc protrusion and insufficient decompression. Wide decompression is required to prevent such failures. However, several studies reported that facet joint violation can cause segmental hypermobility, especially when resected more than 50% [7-9].
Hence, regarding to preserve the segmental stability, it is important to preserve the facet joint as much as possible within the limits of sufficient decompression. In this study, the inclinatory foraminotomy technique, as Chang et al. [14] introduced previously, was applied to preserve segmental stability by undercutting of the facet joint. This approach allowed enough foraminal decompression with less facetectomy without violation of facet capsule compared with conventional surgery that would need about 50% facetectomy for sufficient foraminal decompression. Radiological results in this study showed significant enlargement of the foraminal area with successfully removed protruded discs without compromising the stability of the cervical spine in all cases.
In most cases, authors could realize BE-PCIF had more advantages compared with traditional PCF. Perineural fat on an axillar area of exiting root could be found very easily and a wider operative view for surgical management was acquired. Especially, during the decompression of the distal part of the root, the facet joint could be more effectively preserved by tunnel-shaped foraminotomy, which undercut the facet joint and save the dorsal portion of the facet capsule and it was different from traditional PCF which sacrifices the integrity of the facet joint by direct unroofing for the decompression of the distal root (Fig. 8).
The authors think the following factors of BE-PCIF might have facilitated such successful results in the current cases.
First, an optimized surgical view was provided in BE-PCIF. Magnified, clear operative view by spinal endoscope under continuously irrigating water medium helped the surgeon to distinguish between nerves and surrounding structures well. Such a better operative view enables the operator to perform meticulous, fine manipulation around the root safely, especially during bleeding control of the venous plexus around the root or dissection for perineural adhesion. The spinal endoscope has a thin and long stick shape body with an optic lens called ‘surgical eye’ which is located in the distal tip. Such structural property of endoscope with an inclined approach angle in the current technique enabled close access to operative target in relative narrow space [24]. These advantages facilitated decompressive work, especially, in the distal root area. The bony structure of the facet joint was undercut by drill or tip of SAP was cut with a chisel with a good operative view and effective handling of instruments.
Second, the unconstrained use of instruments such as up-bite pituitary forceps, bendable drills, angled chisel, and curette also contributed to the successful surgical results in the current cases. During foraminal decompression, the inclinatory approach from the contralateral side provided a more efficient surgical trajectory along the root pathway to handle the operative instruments with an optimized operative view toward the far lateral foraminal area. The working portal of 2 portals provided relatively large operative space for disengaged use of the operative instruments. Additionally, various angled instruments made it easier for the operator to perform complicated surgical works in the foraminal area where is difficult to access due to the limited approach angle and narrow operative space.
The unique characteristics of BE-PCIF, such as sufficient operative space and effective handling of various instruments by inclinatory, optimized surgical view would lead to successful surgical results for cervical foraminal decompression in the current cases.
Although there was only 1 case, the seventh patient who was presented with bilateral cervical radiculopathy was also treated by BE-PCIF. Traditional PCF surgery for bilateral pathology was usually avoided because of the increasing risk of postoperative instability from bilateral facet violation and axial neck pain from excessive soft tissue injury during an operation. The seventh patient who underwent BE-PCIF showed favorable postoperative clinical course without such negative consequences. The authors assume it came from major advantages of BE-PCIF, such as minimized oblique facet resection and musculoligamentous injury.
BE-PCIF could be used as an effective treatment of the cervical radiculopathy caused by foraminal stenosis due to foraminal bony spur with or without disc herniation. However, the authors think this technique is not suitable for cases of central canal stenosis, instability, and disc space collapse which would need anterior cervical surgery with height restoration. The operator should make a careful decision for operative indication by examining preoperative CT, MRI, and dynamic x-ray.
One of the demerits of BE-PCIF is a technical difficulty with a steep learning curve as other endoscopic spinal surgeries have. The decompression of the distal part of the cervical root in current cases needed demanding surgical skill because the distal area of foramen had very narrow space to handle the operative instruments and required more flat approach trajectory to access the target. Direct perineural drilling was performed with inclinatory surgical angle as much as possible and remnant thin bony eggshell around the root was removed by a curette. Angled chisel was also a useful surgical tool to remove the tip of SAP. Although the authors achieved a successful outcome in this study, the efficacy of this technique should not be generalized to all spine surgeons. The operator was an expert who has performed over 2,000 cases of BE spine surgery. Especially in this surgery, unmastered use of angled instruments in such a limited operative space may induce injury to the neural structures and result in unfavorable clinical outcome. Thus, surgeons should try this technique after they overcome the learning curve of BE spinal surgery with a lot of surgical experiences.
The great advantage of this technique is the preservation of the facet joint by undercutting the bony structure of the foramen with inclinatory approach angle and minimal injury of the surrounding musculo-ligamentous structures, which also makes us expect the maintenance of the stability at operated segment. However, this study is a retrospective study of case series and has short follow-up periods. Although, in the current studies, the preservation of segmental stability and less neck pain was observed until 6 months after the operation, further follow-up evaluation with a large number of patients would be necessary to prove the efficacy of BE-PCIF in long-term.
CONCLUSIONS
BE-PCIF may be an effective surgical treatment of the cervical radiculopathic lesions, which provides successful surgical decompression of the cervical foramen with a better operative view and more easy surgical manipulation. This approach may also minimize the iatrogenic damages of the posterior cervical musculo-ligamentous structures and help to maximize the preservation of the facet joint.
Notes
The authors have nothing to disclose.
SUPPLEMENTARY MATERIALS
Supplementary video clips 1-6 can be found via https://doi.org/10.14245/ns.2040228.114.v.1, https://doi.org/10.14245/ns.2040228.114.v.2, https://doi.org/10.14245/ns.2040228.114.v.3, https://doi.org/10.14245/ns.2040228.114.v.4, https://doi.org/10.14245/ns.2040228.114.v.5, https://doi.org/10.14245/ns.2040228.114.v.6, and https://doi.org/10.14245/ns.2040228.114.v.7.
The operation video of laminotomy of the inferolateral portion of upper C6 lamina with a diamond drill.
ns-2040228-114-v1.mp4The operation video of laminotomy of the superolateral portion of lower C7 lamina and additional drilling around the root. Tunnel shaped decompression was acquired by drilling of lower lamina. Inter articular plane of the facet joint was revealed during drilling toward lateral portion of lower lamina. The Silhouette of the root was seen through a thin layer at the lateral margin of ligamentum flavum.
ns-2040228-114-v2.mp4The operation video of resection of SAP by curved chisel. The tip of SAP was cut by curved chisel. Isolated bony fragment was removed by curved hook and forcep.
ns-2040228-114-v3.mp4The operation video of the Ligament Flavectomy and coagulation of venous plexus. ligament flavum was removed by piecemeal fashion. Beforehand bleeding control was performed by coagulation of venous plexus around the root with a small tip RF. The root was exposed after removal of lateral part of ligament flavum by punch.
ns-2040228-114-v4.mp4The operation video of passing the probe into the foramen around root. The ball tip probe was passed beyond the distal root through the foramen. Sufficient root decompression was checked by manipulation of the root without resistance in enlarged foraminal area around the root.
ns-2040228-114-v5.mp4The operation video of the root retraction with scope retractor for discectomy. The root which was swollen and compressed by protruded disc was retracted by a scope retractor. Protruded disc was removed by hook and forcep. Decompressed root was seen after discectomy.
ns-2040228-114-v6.mp4The author’s interview and the overall surgical procedures.
ns-2040228-114-v7.mp4


