 |
 |
- Search
| Neurospine > Volume 17(Suppl 1); 2020 > Article |
|
|

Abstract
Minimally invasive techniques for transforaminal lumbar interbody fusion (MIS-TLIF) are advantageous because they allow for sufficient surgical exposure and fewer complications through a smaller incision than conventional TLIF. It could be difficult to maintain minimally invasive spine surgery following the unexpected complications after MIS-TLIF. Because MIS-TLIF is usually done via a paramedian small incision with posterior fusion using screws and rods, visualization of the surgical field is limited, and it is difficult to directly assess the neural structure without removing instrumentation. Unilateral biportal endoscopic decompression (UBE) is a rapidly growing surgical method using two 1-cm incisions that are 2 to 3 cm apart. We would like to suggest UBE as an option for immediate reoperation after MIS-TLIF because it has the advantages of targeting pathologic regions and a wide field of visualization through small wounds. The operation is independent of the existing incision from MIS-TLIF, enabling immediate revision surgery without the removal of the screws and rods. UBE has the advantages of targeting specific surgical regions and providing a wide visualization of the operation field through small incisions. UBE can be very useful for discectomy or decompression surgery as well as in immediate reoperation after MIS-TLIF.
Lumbar spinal fusion is a treatment option for symptomatic spinal instability, spinal stenosis, spondylolisthesis, and degenerative scoliosis [1]. Various methods have been developed to achieve interbody fusion. The surgical approach can be either anterior or posterior. Anterior lumbar interbody fusion and lateral lumbar interbody fusion; Oblique lumbar interbody fusion and extreme lateral interbody fusion have all been performed via the anterior approach [2]. Posterior lumbar interbody fusion or transforaminal lumbar interbody fusion (TLIF) are generally performed via the posterior approach [3]. Foley et al. [4] first described the minimally invasive technique for TLIF (MIS-TLIF), and it has since become an increasingly popular method for lumbar fusion [5].
MIS-TLIF using the tubular retractor system was introduced with the aim of reducing blood loss and soft tissue trauma through smaller incisions, increasing the speed of recovery, and reducing postoperative pain compared with the conventional open technique [6]. As with other operations, there are cases where immediate complications occur, although they are very rare. Postoperative hematoma or cerebrospinal fluid-related problems, wound dehiscence, or implant malpositioning were common postoperative complications [7]. Rarely, there is a case of bony fragment or fracture [8]. If there is an immediate complication after the conventional approach, revision can be performed in an open fashion through the previous incision site. Because MIS-TLIF is usually done via a paramedian small incision with posterior fusion using screws and rods, visualization of the surgical field is limited, and it is difficult to directly assess the neural structure without removing instrumentation. Avoiding a midline incision is one of the main goals of MIS-TLIF, so we do not make an additional midline incision in cases of reoperation.
A new unilateral biportal endoscopic decompression (UBE) was recently introduced. UBE is a rapidly growing surgical method that uses 2 small independent incisions, similar to arthroscopic knee or thoracoscopic surgery. Here we introduce UBE as a solution for immediate reoperation after MIS-TLIF. We experienced 2 cases of successful immediate revision surgery with UBE after MIS-TLIF and report them here with detailed descriptions of the surgical technique.
This study reviewed 2 patients who underwent immediate reoperation using UBE after MIS-TLIF. Clinical data were reviewed that include age, sex, history, radiographs, surgical approaches, visual analogue scale (VAS), and physical and neurological exams. This study was approved by the Institutional Review Board (IRB) of Gangnam Severance Hospital, Yonsei University College of Medicine (IRB No. 3-2019-0413) and all patients signed informed consent.
A 67-year-old woman presented to Gangnam Severance Hospital with left buttock and leg pain and intermittent neurogenic claudication lasting less than 5 minutes for 12 months. The pain radiated to the left S1 dermatome. The patient had undergone 6 nerve blocks and continuous medical therapy for more than 6 months, but her symptoms did not improve. Magnetic resonance imaging (MRI) showed degenerative spondylolisthesis and left extraforaminal disc at L4–5 with foraminal stenosis. The patient underwent MIS-TLIF of L4–5.
The patient began ambulating on postoperative day 2, however, complained of sudden onset right leg pain on postoperative day 6. The pain was an 8/10 on the VAS, and she developed subjective weakness at the right hip, knee, and ankle. CT scans revealed a bony fragment at the right L4 pedicle (Fig. 1). We wanted to avoid removing the previously inserted screws and rod, which would be necessary if entering through the previous incision to remove the bony fragment. Therefore, we planned to remove the inferior articular process through a new incision using a right-sided approach. After general anesthesia, the patient was placed in a prone position on a Jackson table. From the CT image, we decided the target point on anteroposterior and lateral x-ray. Orient it towards the target, along the medical pedicular line, we made two independent incision 2 cm apart (Fig. 2A, B). Inferior incision for endoscope and superior incision for working channel (Fig. 2; Supplementary video clip 1). The operator was positioned on the patient’s right side and the assistant on the left. Two approximately 1-cm stab incisions were made 2 cm apart (Fig. 2C, D). The endoscope was inserted through the left (inferior) incision, and continuous irrigation was begun. We ensured that there was saline output though the right (superior) incision because without continuous irrigation, the operative field is not clear and bleeding control is difficult to achieve. The working channel was then used to insert the surgical instrument and endoscope to secure surgical visualization (Supplementary video clip 1).
After confirming the anatomical landmark under endoscopy, we first identified the upper and lower lamina, and then followed the anatomical structures to visualize the interlaminar space and the pedicle. The previous TLIF resulted in a laminectomy and facetectomy after removing the surrounding soft tissue. We were able to identify the screw thread in our operative field, and a broken piece of the medial pedicle was found next to it. When the bony fragment was removed, there was an area of bone bleeding that was controlled using bone wax. We then cleaned the surrounding tissues and confirmed that there was a sufficient gap between the root and screw thread, placed a Hemovac drain, and finished the operation. The bony fragment was removed successfully (Supplementary video clip 1). The operation time was 67 minutes, and blood loss was 50 mL. The medial pedicle had fractured for unclear reasons after the patient began ambulating following the first operation. The patient continued to complain of back pain at the operation site immediately after the revision surgery. However, her leg pain and weakness improved immediately. The patient discharged on postoperative day 4 with back and leg pain that was a VAS 4/10. Postoperative CT demonstrated that the bony fragment had been completely removed (Fig. 1). The patient was also regularly followed in the outpatient clinic after discharge and patients did well without pain at 6 months from revision surgery. Follow-up will continue to confirm fusion.
A 58-year-old woman presented to Gangnam Severance Hospital with lower back pain, bilateral buttock pain, and intermittent neurogenic claudication lasting less than 10 minutes for 13 months. The pain radiated to the L4–5 dermatomes bilaterally. She had been treated with percutaneous neuroplasty and continuous medical therapy for more than 12 months, however, her symptoms had not improved. MRI showed a disc protrusion and spinal stenosis at L3–4 and L4–5 with foraminal stenosis. The patient underwent MIS-TLIF of L3–4–5.
The patient complained of left buttock and leg pain four days postoperatively that was a 9 out of 10 on the VAS for pain. She occured grade 4 weakness of her left hip flexion/extension. Computed tomography (CT) was performed and revealed a bony fragment in the left L3 foramen (Fig. 3). We planned a L3 laminectomy through a new incision. We performed the revision surgery using UBE using the same steps outlined in case 1 at the opposite side (Fig. 4).
After visualization of the surgical field was confirmed, we first identified the upper and lower lamina, and then followed the anatomical structures to visualize the interlaminar space and pedicle. Laminectomy was done using a high-speed drill and Kerrison punch. Shortly thereafter, we were able to identify the large bony fragment, and after removing it, we performed meticulous bleeding control and cleared the soft tissue. After confirming there were no more fragments, we inserted a Hemovac drain and finished the operation. The bony fragment was removed completely without any complications. The operation time was 76 minutes and blood loss was 150 mL. The patient’s leg pain and paresthesia improved immediately postoperatively, but her weakness was unchanged. Five days after surgery the patient was transferred to the Rehabilitation Department for rehabilitation therapy. The patient was discharged 22 days postoperatively with a back pain VAS score of 2 and complete resolution of her weakness. Postoperative CT demonstrated that the bony fragment had been completely removed (Fig. 3). The patient was regularly followed in the outpatient clinic after discharge and is now 9 months from revision surgery, free of pain. Follow-up will continue to confirm fusion.
MIS-TLIF is a useful surgical method for lumbar fusion surgery. MIS-TLIF has the advantage of good surgical outcomes, fewer complications and a smaller incision than conventional TLIF [4-6,9]. Although it is very rare our experience, it is possible for the bony fragment to compress the root after MIS-TLIF. The revision surgery can be difficult after MIS-TLIF if immediate postoperative complications arise. Two of the primary goals of MIS-TLIF are operating through a small incision and avoiding a midline incision though this interferes with reoperation. Posterior fusion with screws and rods through a paramedian incision is usually done after MIS-TLIF, and it is difficult to directly visualize the neural structures without removing the previous hardware. In addition, avoiding an additional midline incision for reoperation is ideal. We felt that these limitations of immediate revision surgery after MIS-TLIF could be addressed using the recently developed UBE technique.
Endoscopic spine surgery techniques can be largely divided into full-endoscopic spine surgery and endoscopic-assisted spine surgery. The transforaminal and interlaminar approaches are popular in full-endoscopic spine surgery [10]. The transforaminal approach is performed through a Kambin’s intervertebral safety triangle, which lies between the exiting and traversing root [11]. The interlaminar approach can be useful in cases with anatomical constraints such as a high iliac crest and superior migrated disc herniation. The transforaminal approach is preferred for shoulder-type disc herniation, centrally located disc herniation, and recurrent disc herniation, while the interlaminar approach is preferred for axillary type disc herniation and migrated discs, especially those of a high grade [12]. Endoscopic decompression surgeries for stenosis have recently been introduced and are thriving [13]. Full-endoscopic spine surgery is advantageous in that it employs a small puncture incision and allows for rapid recovery, minimal blood loss, and preservation of posterior structures [10,12,13]. However, there are disadvantages associated with the transforaminal approach, including incomplete removal of the herniated disc, ineffective treatment of lumbar spinal stenosis, and a steep learning curve [14]. The interlaminar approach is advantageous for treating patients with a high iliac crest, narrow foramen, and facet joint hypertrophy, which are barriers to the transforaminal approach, and it allows direct access to posterior structures, direct visualization of the spinal canal, and familiar anatomic orientation similar to open or microscope-assisted tubular surgery [10,12]. However, using instruments through a full-endoscopic spine surgery limits the instruments’ size and the independent range of movement.
UBE was recently introduced to overcome the drawbacks of full-endoscopic spine surgery in stenosis decompression and revision surgery [13]. UBE is a rapidly growing surgical method that uses 2 independent 1-cm incisions, approximately 2 to 3 cm apart, similar to arthroscopic knee or thoracoscopic surgery. Two portals are used, one for the endoscope and the other for insertion and manipulation of instruments. UBE is a new method that combines the advantages of microscope-assisted and interlaminar endoscopic spine surgery [10]. The advantages of UBE include the use of conventional instruments and the ability to move the instruments with independent visualization through a separate portal. Because of the wide field of visualization, it is possible to access contralateral and foraminal areas using UBE, and there is less bleeding because of continuous irrigation. In addition, UBE is available with a smaller armamentarium because ordinary arthroscopy and conventional surgical instruments can be used [13]. It can be used not only in discectomy or decompression but also in fusion surgery [15].
Rao et al. [16] demonstrated bone chips might have extruded during compression maneuver applied just prior to final tightening of screws to maintain the normal lordotic curvature. In our cases, it is possible that bone chips were extruded during cage insertion and tightening and in the other case, there would have been a pedicle injury during facetectomy and screw insertion, which later led to fracture after ambulation. For these reasons, relook at whole operative field through the microscope after final tightening of the screws would have prevented these complications [16].
In our cases, reoperation with UBE after MIS-TLIF was safely completed by targeting the exact location of concern and securing a wide view through 2 small incisions. Of course, it was difficult to adjust our angles because of the previously implanted screws, but no other special problems occurred. Through the UBE technique, we were able to remove the bony fragment without removing the screw, and this new revision surgery after MIS-TLIF is more convenient than previous revision techniques that need to remove existing screws first and to remove the bony fragment and insert the screw again. Our case patients were followed for 9 months and 6 months. Although these were not long-term periods, patients had no complications. Long-term follow-up is not considered an important part of bony fragment removal. However, long-term follow-up is needed to confirm fusion of MIS-TLIF. Based on our experience, we suggest that UBE can be used as a revision option for MIS-TLIF as well as other MIS fusion surgery techniques, including oblique lumbar interbody fusion and direct/extreme lateral interbody fusion, because it is performed through a new small incision rather than the previous incision and allows sufficient visualization to identify neural structures without the removal of previous instrumentation. In addition, UBE will be useful in the treatment of incidental durotomy and postoperative hematoma after conventional surgeries.
SUPPLEMENTARY MATERIALS
Supplementary video clip 1 can be found via https://doi.org/10.14245/ns.2040174.087.v.1.
Fig. 1.
(A) Computed tomography (CT) showed a bony fragment at the right L4 pedicle (white dotted circle). (B) Postoperative CT confirmed that the bony fragment had been removed. Preoperative (C) and postoperative CT axial images (D). Bony fragment (white dotted circle) was removed postoperatively.
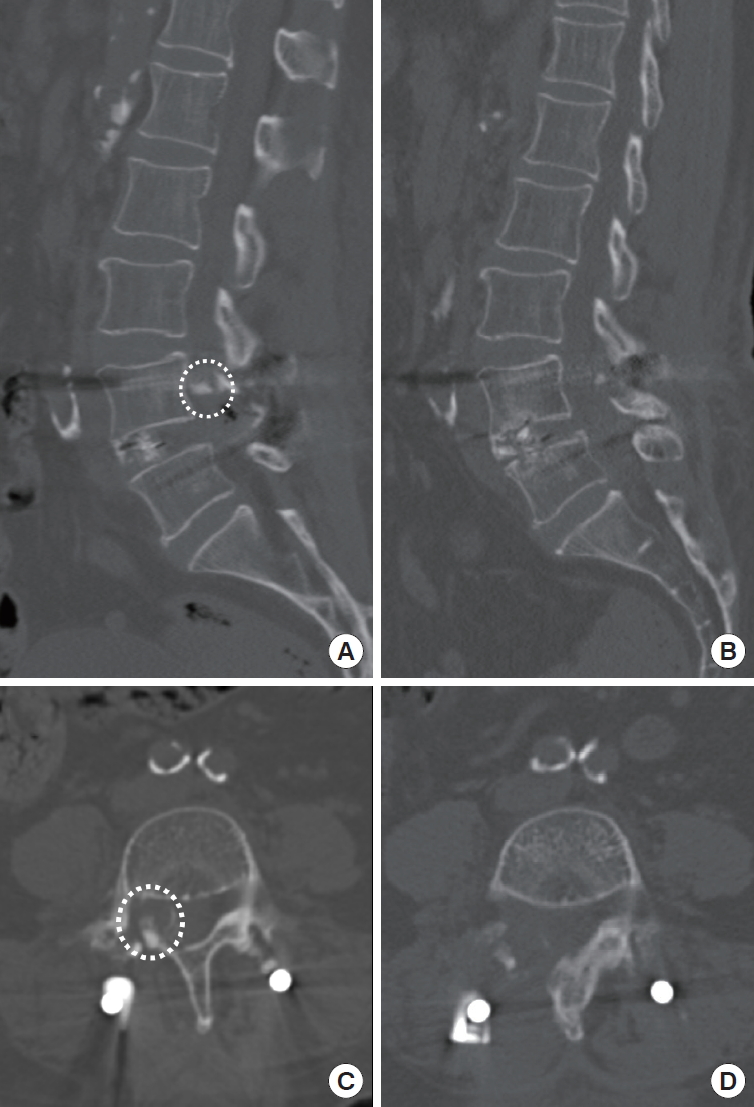
Fig. 2.
Target oriented approach for biportal endoscopic revisional surgery in case 1. From the computed tomography image (Fig. 1), we decided the target point (asterisk) on anteroposterior (A) and lateral radiographs (B). Orient it towards the target (black arrow), along the medial pedicular line, make 2 independent incision (black and white double arrows) 2 cm apart (A, B). Inferior incision for endoscope and superior incision for working channel. Black dotted line is previous minimally invasive technique for transforaminal lumbar interbody fusion (MIS-TLIF) incision. Photo image of postoperative wound. There was 2.5-cm skin wound for MIS-TLIF bilaterally, and medial of the right MIS-TLIF wound, 2 independent 1-cm wounds for biportal endoscopic surgery was seen (C, postoperative 3 days; D, postoperative 2 months).
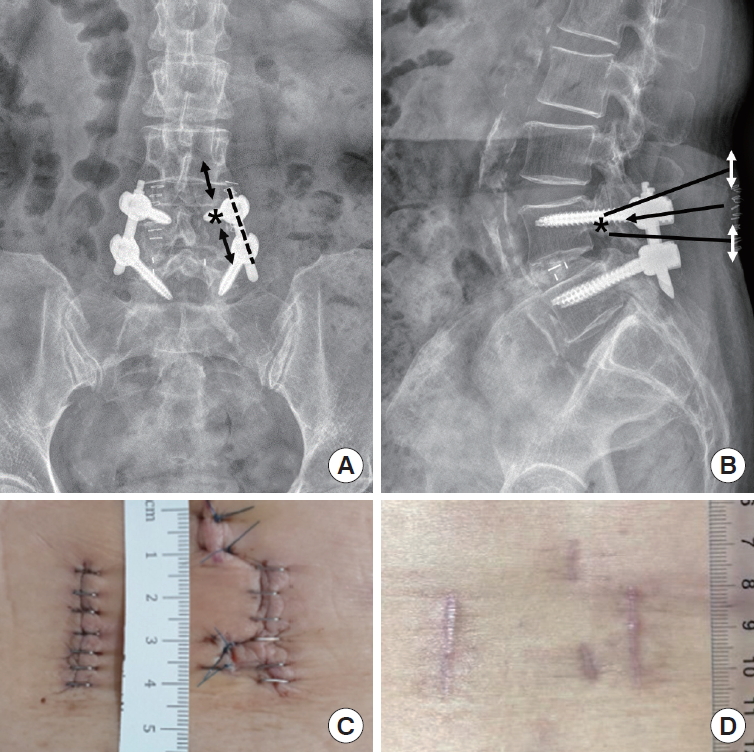
Fig. 3.
(A) Computed tomography (CT) showed a bony fragment in the left L3 foramen (white dotted circle). (B) Postoperative CT confirmed that the bony fragment had been removed. Preoperative (C) and postoperative CT axial images (D). Bony fragment (white dotted circle) was removed postoperatively.
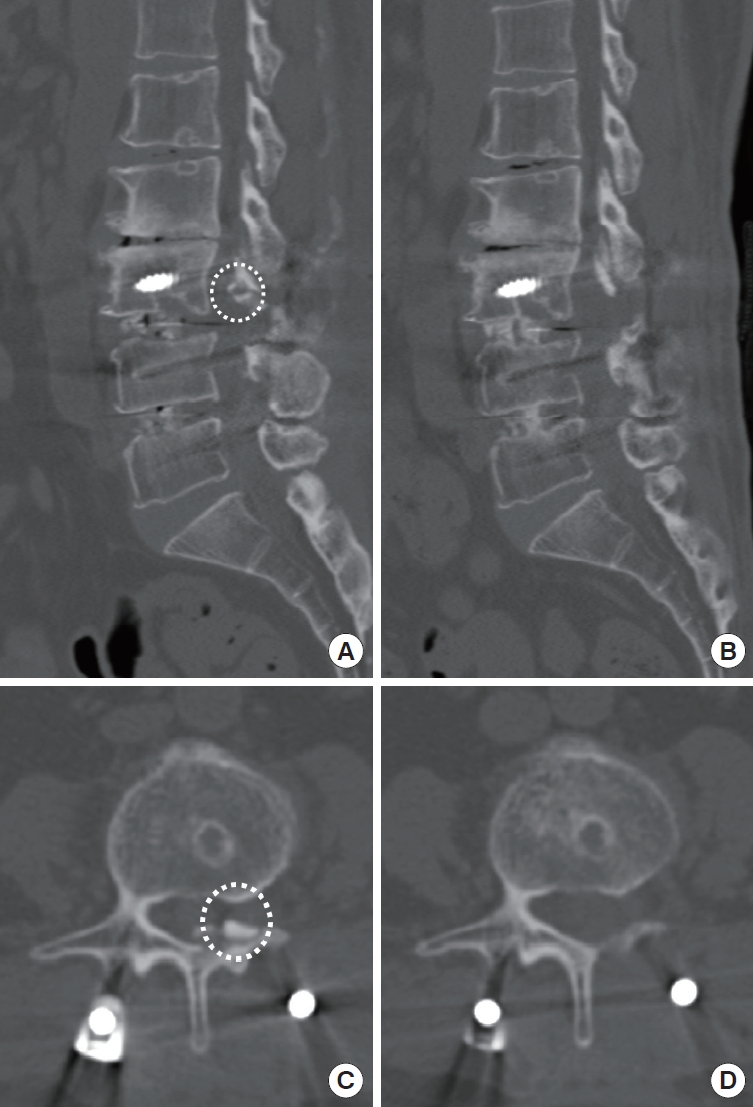
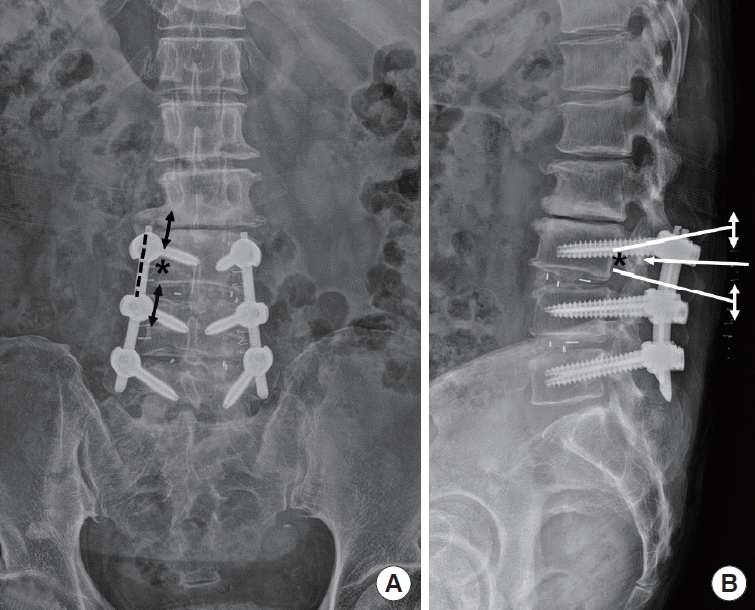
Fig. 4.
Target oriented approach for biportal endoscopic revisional surgery in case 1. From the computed tomography image (Fig. 3), decide the target point (asterisk) on anteroposterior (A) and lateral radiographs (B). Orient it towards the target (black arrow), along the medical pedicular line, make 2 independent incision (black and white double arrow) 2 cm apart (A, B). Superior incision for endoscope and inferior incision for working channel. Back dotted line is previous minimally invasive technique for transforaminal lumbar interbody fusion incision.
REFERENCES
1. Resnick DK, Choudhri TF, Dailey AT, et al. Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 8: lumbar fusion for disc herniation and radiculopathy. J Neurosurg Spine 2005 2:673-8.


2. Mobbs RJ, Phan K, Malham G, et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 2015 1:2-18.


3. Hackenberg L, Halm H, Bullmann V, et al. Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J 2005 14:551-8.




5. Holly LT, Schwender JD, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications. Neurosurg Focus 2006 20:E6.

6. Lee CK, Park JY, Zhang HY. Minimally invasive transforaminal lumbar interbody fusion using a single interbody cage and a tubular retraction system: technical tips, and perioperative, radiologic and clinical outcomes. J Korean Neurosurg Soc 2010 48:219-24.




7. Schoenfeld AJ, Ochoa LM, Bader JO, et al. Risk factors for immediate postoperative complications and mortality following spine surgery: a study of 3475 patients from the National Surgical Quality Improvement Program. J Bone Joint Surg Am 2011 93:1577-82.


8. Wagner R, Iprenburg M, Telfeian AE. Transforaminal endoscopic decompression of a postoperative dislocated bone fragment after a 2-level lumbar total disc replacement: case report. Neurosurg Focus 2016 40:E8.


9. Lee WC, Park JY, Kim KH, et al. Minimally invasive transforaminal lumbar interbody fusion in multilevel: comparison with conventional transforaminal interbody fusion. World Neurosurg 2016 85:236-43.


10. Choi G, Pophale CS, Patel B, et al. Endoscopic spine surgery. J Korean Neurosurg Soc 2017 60:485-97.




11. Kambin P, Sampson S. Posterolateral percutaneous suction-excision of herniated lumbar intervertebral discs. Report of interim results. Clin Orthop Relat Res 1986 (207):37-43.
12. Choi KC, Kim JS, Ryu KS, et al. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation: transforaminal versus interlaminar approach. Pain Physician 2013 16:547-56.

13. Lin GX, Huang P, Kotheeranurak V, et al. A systematic review of unilateral biportal endoscopic spinal surgery: preliminary clinical results and complications. World Neurosurg 2019 125:425-32.


14. Lee SH, Kang BU, Ahn Y, et al. Operative failure of percutaneous endoscopic lumbar discectomy: a radiologic analysis of 55 cases. Spine (Phila Pa 1976) 2006 31:E285-90.






























