Metabolic Syndrome is a Predisposing Factor for Diffuse Idiopathic Skeletal Hyperostosis
Article information
Abstract
Objective
Diffuse idiopathic skeletal hyperostosis (DISH) causes spinal ankylosis, which can result in patients suffering specific spinal fractures that lead to a reduction in the activities of daily life in older patients. Currently, DISH is associated with diabetes mellitus and cardiovascular disease; however, the association between DISH and metabolic syndrome has not been established. The purpose of this study was to investigate a potential association between DISH and metabolic syndrome.
Methods
We retrospectively reviewed clinical data from consecutive subjects undergoing the musculoskeletal health medical checkups, and enrolled 327 subjects (174 men and 153 women; mean, 63.4 ± 13.7-years). Subjects who had spinal ankylosis at least 4 contiguous vertebral bodies were classified as the DISH group (n = 39) while the others were part of the non-DISH group (n = 288). The definition of the metabolic syndrome comes from diagnostic criteria used by the Japanese Society for Internal Medicine. Age, sex, body max index (BMI), hematological evaluation, blood pressure, presence of metabolic syndrome, the visceral fat area on abdominal computed tomography, and spinal epidural lipomatosis (SEL) on magnetic resonance imaging were evaluated.
Results
Compared to the non-DISH group, in the DISH group, mean age (DISH group, 74.3 years; non-DISH group, 1.9 years; p < 0.001), male prevalence were higher (DISH group, 82.1%; non-DISH group, 49.3%; p < 0.001), and BMI was greater (DISH group, 24.8; non-DISH group, 23.0; p = 0.006). the metabolic syndrome was more frequently observed in DISH group (28.9%) than in the non-DISH group (16.0%) (p = 0.045). The visceral fat area was significantly larger in the DISH group than in the non-DISH group (DISH group, 130.7 ± 58.2 cm2; Non-DISH group, 89.0 ± 48.1 cm2; p < 0.001). The prevalence of SEL was similar between the 2 groups (10.3% in the DISH group vs. 8.7% in the nonDISH group; p = 0.464). Poisson regression analysis revealed that the metabolic syndrome was significantly associated with DISH with odds ratio of 2.0 (95% confidence interval, 1.0–3.7; p = 0.004).
Conclusion
Metabolic syndrome was significantly associated with DISH. Our data showed metabolic syndrome is potentially related to DISH.
INTRODUCTION
The concept of diffuse idiopathic skeletal hyperostosis (DISH) was first suggested by Resnick et al. [1] in 1975. DISH is a noninfuriately condition with systemic skeletal ankylosis that mainly affects the T7–11 region of the thoracic spine at onset but tends to extend in the cephalad and caudal direction with age [2]. DISH can negatively affect activities of daily life in older patients because it can cause clinical problems such as low-back pain, limitation in spinal movement [3], dysphasia [4], spinal fracture after minor trauma [5-7], and poor outcomes after surgery for lumbar degenerative disease [8-10]. To date, previous reports have identified certain factors associated with DISH, such as male sex [11,12], old age (> 50 years) [11-13], synthetic retinoid use [14], ethnic factors (less common in the black, Native-American, and Asian) [13,15], and genetic factors (COL6A1) [16].
Furthermore, metabolic abnormalities [17], diabetes mellitus (DM) [18,19], and cardiovascular diseases [20] have also been previously reported to have a potential association with DISH. In 1996, Vezyroglou et al. [19] compared 100 patients with DISH with 100 patients without DISH who were matched for age, sex, and body mass index and found that metabolic disturbances such as DM, dyslipidemia (DL), and hyperuricemia were confined to the DISH group.
Metabolic syndrome is characterized by metabolic abnormalities, including insulin resistance and the associated abdominal obesity, hyperglycemia, hyperinsulinemia, DL, and hypertension [21,22]. Previous studies indicated that metabolic syndrome increased the risk of type 2 DM, cardiovascular events, and death. The concept of metabolic syndrome was first reported in the United States in 2001 and the pathophysiology of metabolic syndrome has been revised after additional research. According to the National Health and Nutrition Examination Survey [23], the prevalence of metabolic syndrome in the United States over 20 years is approximately 31.9% (30.6% in men and 33.2% in women). Recently, the incidence of metabolic syndrome is increasing, even in developing countries, due to Western diet patterns.
Hence, metabolic disturbances seem to have an impact on the development of DISH. However, as DISH remains insufficiently investigated and understood, its definitive etiology is still unclear. Therefore, the purpose of this study was to elucidate the association between DISH and the metabolic syndrome.
MATERIALS AND METHODS
We obtained approval from the Institutional Review Board (IRB) of Keio University School of Medicine (IRB number: 20160199) before initiating this retrospective cross-sectional study, and the study was a part of the musculoskeletal health checkup studies [24,25]. Study subjects were notified of this study’s opt-out option. We retrospectively identified 333 consecutive participants who underwent a musculoskeletal checkup in addition to a regular medical checkup from 2012 to 2016. The musculoskeletal checkup was voluntary and was not organized by the government or by a company. The cost of the musculoskeletal checkup was charged to the individual. Public medical insurance was not applied to this musculoskeletal medical checkup. Inclusion criteria for the study were participants: (1) who had the musculoskeletal checkup, (2) who are at least 20 years old, and (3) who have a complete dataset. The exclusion criteria for this study were participants: (1) who had a history of ankylosing spondylitis and (2) who did not consent to be in the study. Among these, 5 were excluded because of missing data, and we excluded one more because of a history of ankylosing spondylitis. Thus, 327 subjects were included in the study that comprised 174 men and 153 women with a mean age of 63.4± 13.7 years (range, 24–89 years) at the time of investigation. The presence of DISH was evaluated based on findings seen in the lateral and the anteroposterior aspects of spine radiographs. Subjects were diagnosed with DISH and classified into the DISH group (n = 39) if they had spinal ankylosis with flowing ossification along the anterolateral aspect of at least 4 contiguous vertebral bodies [1]; otherwise, they were categorized non-DISH group (n = 288). Variables such as waist circumference, systolic blood pressure (DBP), and diastolic blood pressure (DBP) were measured, and blood and urine assessments and serial radiographs of the thoracic spine, lumbar spine, abdominal computed tomography (CT), and lumbar spine magnetic resonance imaging (MRI) were performed.
In the abdominal CT, the visceral fat area (VFA) was measured at the level of the navel (Aquilion CXL, Toshiba Medical Systems Corp., Tochigi, Japan). Digital Imaging and Communication in Medicine data were analyzed using the sliceOmatic software (TomoVision, Magog, Quebec, Canada) [25]. Details of lumbar spine MRI acquisition have been described elsewhere by Ishihara et al. [25]. The anterior-posterior (AP) distance ratio of epidural fat was measured on T2-weighted axial images, and spinal epidural lipomatosis (SEL) was defined as 0.6 AP distance ratio of epidural fat in at least one lumbar level [26]. Additionally, we retrieved the results of blood and urine analyses, including high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), adiponectin, fasting blood glucose, glycated hemoglobin, insulin, homeostasis model assessment as an index of insulin resistance, urine microalbumin, high sensitivity C-reactive protein, and B-type natriuretic peptide. All blood samples were collected under overnight fasting conditions. The diagnostic criteria used for the metabolic syndrome were those defined by the Japanese Society for Internal Medicine [27] and are as follows: VFA ≥ 100 cm2 with any 2 of the following conditions: (1) TG ≥ 150 mg/dL and/or HDL-C < 40 mg/dL, (2) SBP ≥ 130 mmHg and/or DBP ≥ 85 mmHg, or (3) fasting plasma glucose ≥ 110 mg/dL.
We examined the association between categorical variables and the presence of DISH using the chi-squared test. For the comparison of continuous variables between the DISH and non-DISH groups, we assumed no clear violation of the normality assumption and used Student t-test. We applied a Poisson regression model to examine a possible association between DISH and metabolic syndrome. In this model, we adjusted for confounding factors, including age, sex, and lifestyle factors such as smoking and alcohol drinking. VFA, blood pressure, lipid metabolism, and carbohydrate parameters were not used as adjustment factors because these factors were covered by the diagnostic criteria for metabolic syndrome. Data are expressed as mean ± standard deviation. A p-value less than 0.05 was considered statistically significant. We used IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA) and Stata 15 (Stata Corp., College Station, TX, USA) for all statistical analyses.
RESULTS
1. Demographic Parameters and Metabolic Syndrome
Demographic data pertaining to DISH and non-DISH groups are presented in Table 1. Patients in the DISH group were significantly older (DISH group, mean 74.3 years; non-DISH group, mean 61.9-years; p < 0.001), and the proportion of males was higher (DISH group, 82.1%; DISH group, 49.3%; p < 0.001). Mean body height, waist circumference, smoking habit, and alcohol consumption were similar between the 2 groups; by contrast, body weight (DISH group, 65.6 ± 10.8 kg; non-DISH group, 60.9 ± 13.3 kg; p = 0.035) and BMI (DISH group, 24.8; non-DISH group, 23.0; p = 0.006) were significantly higher in the DISH group than in the non-DISH group.
2. Blood Pressure and VFA
Blood pressure and VFA on the abdominal CT were diagnostic criteria for metabolic syndrome. SBP in the DISH group (DISH group, 129± 19.2 mmHg; non-DISH group, 121.6± 17.8 mmHg; p = 0.026) was significantly higher than that in the nonDISH group, but DBP was comparable (Table 1). The VFA on abdominal CT was significantly larger in the DISH group than in the non-DISH group (DISH group, 130.7 ± 58.2 cm2; non-DISH group, 89.0 ± 48.1 cm2; p < 0.001).
3. Blood and Urine Analyses
Blood and urine analyses were conducted to evaluate lipid and carbohydrate metabolism, indicating metabolic abnormalities. In lipid metabolism parameters, no significant difference in LDL-C, TG, or adiponectin was observed between the 2 groups; however, HDL-C was significantly lower in the DISH group (53.2 ± 13.6 mg/dL) than in the non-DISH group (60.5 ± 15.7 mg/dL, p = 0.006) (Table 1). Similarly, carbohydrate metabolism parameters had no significant difference between the 2 groups except for urine microalbumin, which was higher in the DISH group (DISH group, 36.2 ± 80.3 mg/dL; non-DISH group, 14.4 ± 60.1 mg/dL; p = 0.046).
4. Metabolic Syndrome and SEL on Lumbar MRI
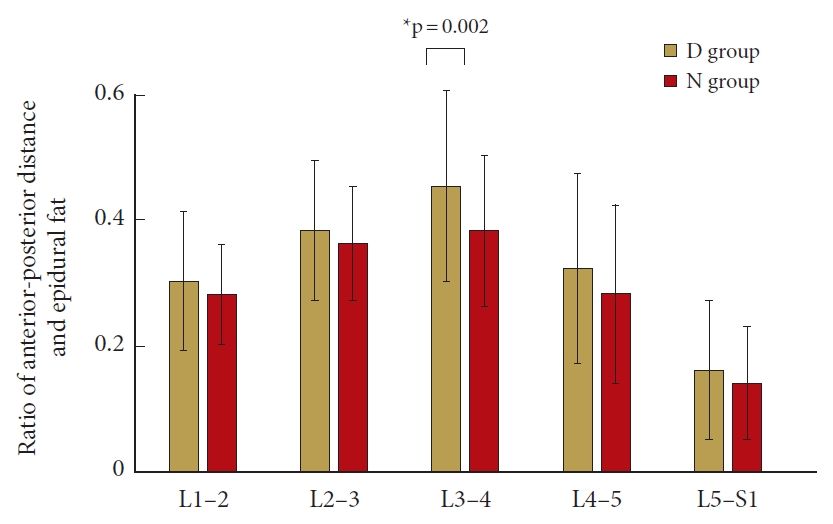
From the results of the investigated parameters and lumbar MRI, diagnoses of metabolic syndrome and SEL were made. The prevalence of the metabolic syndrome was significantly higher in the DISH group (28.9%) than in the non-DISH group (16.0%, p = 0.045). Based on lumbar MRI, 29 out of 327 subjects (8.9%) were diagnosed with SEL. The prevalence of SEL was not significantly different between the 2 groups (10.3% in the DISH group vs. 8.7% in the non-DISH group, p = 0.464). Fig. 1 illustrates the results of AP distance ratio of epidural fat at each level. At L3–4, the AP distance ratio was significantly larger in the DISH group (0.45 ± 0.11) than in the non-DISH group (0.38 ± 0.15. p = 0.002) (Fig. 1). However, there was no significant difference at L1–2, L2–3, L3–4, or L5–S1.
5. Subgroup Analysis
We examined the association of metabolic syndrome and SEL with DISH (Table 2). Before adjustment for any variable, metabolic syndrome was weakly associated with DISH; however, SEL was significantly associated with DISH (relative risk [RR], 2.6; 95% confidential interval [CI], 1.3–5.1; p < 0.01). After adjustment for age, sex, smoking habits, and alcohol drinking, metabolic syndrome was positively assciated with DISH (RR, 2.0; 95% CI, 1.0–3.7; p = 0.04), but SEL was not associated with DISH. These results imply that the presence of DISH and metabolic syndrome exist together.
6. Case Presentation
A 73-year-old male had spinal ankylosis from T4–9 and was assigned to the DISH group (Fig. 2). His body height, body weight, and BMI were 162 cm, 78 kg, and 29.4 kg/m2, respectively. According to the abdominal CT image, the VFA was 258.1 cm2 and the patient had 2 positive conditions: (1) TG of 239 mg/dL and (2) SBP of 155 mmHg and DBP of 99 mmHg (Fig. 3). On the lumbar MRI, the AP distance ratios of epidural fat were lower than 0.60, except 0.61 at L5–S1 (Fig. 4). The patient was diagnosed with metabolic syndrome and SEL.

Case presentation: a 73-year-old male. Serial radiographs of the thoracic spine indicated spinal ankylosis from T2 to T9. Anteroposterior (A) and lateral (B) radiographs.

Abdominal computed tomographic image of the visceral adipose area (red) and subcutaneous fat area (blue) at the level of the navel. The visceral adipose area was 258.1 cm2.
DISCUSSION
Here, we demonstrate that DISH was observed more frequently in obese older males compared to the non-DISH subjects. These observations are consistent with those reported in previous studies [28,29]. Toyoda et al. [2] investigated findings from standing whole-spine radiographs of 345 consecutive patients who underwent spinal surgery and reported that the prevalence of DISH increased with age. In the present study, the prevalence of DISH was 11.9%, relatively low. In 2018, Banno et al. [29] evaluated 504 older volunteers and found that the prevalence of DISH was 8.3%. Additionally, they found that DISH occurred more frequently in men (14.3%) than in women (4.3%), and that the mean age was higher in subjects with DISH than in those without DISH (78.4 years vs. 73.5 years, respectively). The prevalence of DISH is significantly affected by subject’s population, such as patients who underwent spinal surgery [2] or healthy volunteers [29]. The all participants of the present study were medical checkup examinee without severe spinal complaint. Obesity is one of characteristics of DISH. Recently, Chaput et al. [30] conducted CT-based survey of 214 trauma patients who were under 50 years of age and revealed that ossification of the anterior longitudinal ligament was associated with increased adiposity. Further, they suggested that obesity may play a more important role in spinal ossification than in age-related degeneration.
Our results indicate higher SBP and larger VFA in DISH subjects compared to non-DISH subjects, and one previous study [31] has reported a higher frequency of hypertension in patients with DISH (61.1%) compared to those without DISH (25.0%). One of the highlights of the present study was estimation of the VFA in DISH subjects, which was significantly larger than that seen in the control group. Dan Lantsman et al. [32] also investigated abdominal CT findings in 43 DISH patients and reported that VFAs were larger in DISH patients than in controls. They also suggested that the greater amount of fat tissue may represent a potential pathogenic pathway of enthesopathic excessive bone production. In 2001, Rogers and Waldron [33] conducted a unique study to investigate the prevalence of DISH in skeletons from cemeteries in monasteries and churches. They found that skeletons from individuals with higher social status had a significantly greater prevalence of DISH compared to those from individuals with lower social status (p < 0.001); therefore, the authors opined that a rich diet, such as that with animal fat and alcohol, might be associated with the onset of DISH, even in medieval periods.
We revealed multiple abnormalities in laboratory data in subjects with DISH, such as in lipid (HDL-C) and carbohydrate (urine microalbumin) metabolism parameters. Further, the prevalence of DM in DISH patients tends to be greater than that in the normal population [18]. In 2009, Mader and Lavi [31] investigated individuals in the early phase of DISH, i.e., younger than 50 years of age, and reported that the prevalence of first-degree relatives with DM was greater in DISH patients. In 2018, they investigated serum adiponectin levels in patients with DISH and reported that higher serum adiponectin was associated with serum cholesterol and LDL levels and extension of bony bridges (r= 0.245, p = 0.02). In the present study, lower HDL-C levels but higher urine microalbumin indicated abnormal carbohydrate and lipid metabolism in DISH subjects, suggesting that carbohydrate and lipid metabolism may play either a direct or an indirect role in the pathogenesis of DISH. Despite previous studies suggesting a relation between DISH and cardiovascular disease [20], we could not find any significant association.
The unique aspect of our study is that it analyzed the involvement of SEL in subjects with DISH. To the best of our knowledge, no previous study has investigated the association between DISH and SEL, and similarly to those in previous studies, the patient profile of subjects with SEL and DISH included obesity and metabolic dysfunction [26,34]. Theyskens et al. [34] reviewed the medical records of 28,902 patients and found that the factors associated with SEL were old age, high modified Charlson comorbidity index, male gender, BMI > 30 kg/m2, and systemic corticosteroid use. In agreement with the Ishihara study, we found a larger amount of epidural fat on the lumbar MRI in DISH patients at all lumbar segments, especially a significant increase at L3–4. Our results indicate that systemic lipid metabolism abnormalities may exist in DISH subjects.
This study has several limitations. First, we diagnosed DISH based on serial radiographs rather than CT scans, even though CT scans can advantageously detect 3-dimensional vertebral ossification. We did not obtain spinal CT scans, but we hypothesize that CT scans of the whole spine would identify a larger prevalence of DISH than that reported here. Furthermore, we could not evaluate major ossification of the spine, ossification of posterior longitudinal ligament, because we could not obtain cervical spine radiographs. Second, as this was a cross-sectional study, a causal association between metabolic syndrome and DISH cannot be evaluated. Third, the subjects of the present study were not randomly selected healthy volunteers; rather, all subjects in the present study wanted information about their medical condition and thus agreed to participate in the medical checkup. This constitutes a potential selection bias. However, as there have been few studies investigating a possible association between metabolic syndrome and DISH, we believe that this study makes a significant contribution to the explanation of the etiology associated with ossification of the spinal ligaments.
In conclusion, our data suggested that advanced age, male sex, higher BMI, and metabolic syndrome are associated with DISH. Metabolic syndrome is a predisposing factor for DISH. This result can promote understanding the etiology of DISH.
Notes
MM has relevant financial activities outside the submitted work: NuVasive Japan (consultancy, institutional grant). The other authors declare that there are no relevant conflicts of interest.