Chronic Opioid Use Following Lumbar Discectomy: Prevalence, Risk Factors, and Current Trends in the United States
Article information
Abstract
Objective
Lumbar discectomy is commonly performed for symptomatic lumbar disc herniation. We aimed to examine prescribing patterns and risk factors for chronic opioid use following lumbar discectomy.
Methods
Using a private insurance claims database, patients were identified who underwent primary lumbar discectomy from 2010–2015 and had 1-year of continuous enrollment postoperatively. Patients were excluded with spinal fusion. The strength of opioid prescriptions was quantified using morphine milligram equivalents daily (MMED). Univariate and multivariate logistic regression models were built to examine risk factors associated with chronic postoperative opioid use.
Results
A total of 5,315 patients were included in the study (mean age, 59 years; 50% female). 1,198 of patients (23%) used chronic opioids postoperatively. Chronic opioid use declined significantly from 27% in 2010 to 17% in 2015, p < 0.001. In addition, there were significantly fewer patients receiving high and very high-dose opioid prescriptions from 2010–2015, p < 0.001. The median duration that patients used opioids postoperatively was 211 days in 2010 (interquartile range [IQR], 29–356 days), and decreased significantly to 44 days (IQR, 10–294 days) in 2015. The strongest factors associated with chronic opioid use were preoperative opioid use (odds ratio [OR], 4.0), drug abuse (OR, 2.6), depression (OR, 1.6), surgery in the west (OR, 1.6) or south (OR, 1.6), anxiety (OR, 1.5), or 30-day readmission (OR, 1.4).
Conclusion
Chronic opioid use following primary lumbar discectomy has declined from 2010–2015. A variety of factors are associated with chronic opioid use. Preoperative recognition of some of these risk factors may aid in perioperative management and counseling.
INTRODUCTION
A significant number of patients remain on opioids long term following lumbar discectomy [1,2], despite postoperative complications being uncommon and generally excellent pain relief with this procedure, with documented success rates approaching 90% [3-6].
Opioid use in the United States has been declared a “public health emergency,” with the highest per-capita consumption in the world, and an estimated 11 million misused narcotic prescriptions annually [7,8]. Increased opioid prescription in addition to an increase in heroin and illicit fentanyl use has contributed to opioid-related overdoses increasing by a factor of five between 2009 and 2016 [9]. Fortunately, the increasing awareness of the epidemic combined with legislative action limiting narcotic prescriptions have resulted in a decline in opioid abuse [10-14]. Between 2016 and 2017, the number of opioid-related deaths peaked at 47,600 in 2018 [15]. Nonetheless, the opioid crisis remains a significant and life-threatening burden on healthcare, with orthopedics ranking third highest among opioid prescribing specialties [9,16-18]. Accordingly, the American Academy of Orthopedic Surgeons has released practice guidelines to mitigate inappropriate prescription of opioids among all types of orthopedics surgery [19].
There is limited data on opioid prescribing patterns and chronic use after lumbar discectomy, the overall high rate of persistent opioid use in patients with spinal pathology warrants further study of this topic [2,20,21]. The objective of our study is to examine recent trends in opioid prescribing patterns and prevalence of chronic opioid use in patients undergoing primary lumbar discectomy. In addition, we aim to determine preoperative risk factors for chronic postoperative opioid use.
MATERIALS AND METHODS
This study utilized the Truven Health Analytics Marketscan© Commercial Claims and Encounters Database (IBM, Armonk, NY, USA), which is an administrative claims database that does not include patient identifiers and is Health Insurance Portability and Accountability Act compliant. Thus, this investigation was exempt from Institutional Review Board approval.
1. Data and Patient Sample
The Truven Health Analytics Marketscan Commercial Claims and Encounters Database includes private insurance claims information from an aggregation of private payers. Patients included in this database are either employees with insurance provided through their employer, dependents of insured employees, retirees, or Consolidated Omnibus Budget Reconciliation Act continues, and we included patients who were younger than 65 years old. Although the data is deidentified at a patient level, each individual in this database has a unique identifier that allows claims for unique patients to be linked from inpatient data to outpatient data and pharmaceutical claims. We utilized current procedural terminology (CPT) and International Classification of Diseases, Version 9, Clinical Modification (ICD-9-CM) codes to identify patients and apply our inclusion/exclusion criteria (Supplementary Table 1). Comorbidities were also defined using ICD-9-CM codes (Supplementary Table 2).
The United States (US) region in which the surgery was performed was categorized according to US Census Bureau definitions, including: Northeast, North Central, Western, or Southern regions. Few patients (< 1%) included in the Marketscan database do not have an identifiable region associated with their surgical procedure, and these patients were not included in the geographic analysis.
1) Inclusion and exclusion criteria
Patients were included who had a diagnosis of lumbar disc displacement (ICD-9-CM 72210), and who underwent a discectomy procedure (CPT 63030, 63056). It was mandated that these patients had prescription drug coverage as part of their insurance plan, and were continuously enrolled in their insurance policy from 3 months prior to 1-year following surgery. Patients were excluded who had spinal fusion procedures or instrumentation that was placed, or if the discectomy was a revision. Because it was found that several opioid prescription outliers existed and were determined to be aberrantly coded, patients were excluded who had prescription quantities that were in excess of the 99th percentile (Fig. 1).
2. Opioid Utilization
All opioid prescriptions were examined starting 90 days prior to surgery, up to 1-year following surgery. Several time periods surrounding the index surgery were examined. The preoperative period was categorized as 90 days prior to 7 days preceding surgery; the perioperative period was defined as 6 days preceding surgery to 90 days following surgery, and the postoperative period was defined as 91 to 365 days following surgery. All prescriptions were associated with national drug codes, which are 10-digit numbers that allow identification of specific opioid formulations. Given that we identified all opioid medications (ex: oxycodone, fentanyl, morphine, codeine), these medications were converted to an equivalent strength unit of morphine milligram equivalents daily (MMED). The formula for calculating MMED is strength per unit × (number of units/days supply) × MME conversion factor=MMED. High-dose opioid prescriptions were defined as ≥ 90 MMED, and very high-dose opioid prescriptions were defined as ≥ 200 MMED, according to Centers for Disease Control and Prevention (CDC) guidelines that advise against routine prescriptions of this strength. We defined chronic opioid use as receiving a cumulative opioid quantity of ≥ 120 days’ supply or ≥ 10 different opioid prescriptions filled between postoperative months 3–12. This definition has been utilized in previous studies [22,23] and is based on Office of the Inspector General Recommendations [24].
3. Statistical Analysis
Data were displayed as mean ± standard deviation for normally distributed variables, median (interquartile range [IQR]: lower quartile–upper quartile) for nonnormally distributed variables, or N (%) for categorical variables. Temporal and geographic trends were analyzed using logistic regression models, with age and sex as covariates. Univariate regression was performed for each variable of interest in relation to chronic postoperative opioid use. Variables with significance of p < 0.10 were used to construct a multivariate logistic regression model in order to assess the degree to which these variables are independently associated with chronic opioid use. Significance was considered throughout the study at p < 0.05. The analysis was performed using Stata 15 (StataCorp LP., College Station, TX, USA).
RESULTS
1. Characteristics of the Study Population
A total of 5,315 patients were identified who met criteria for inclusion into our study. Patients were 49 years old on average and 2,672 (50%) were female. 3,105 (58%) had at least one preoperative opioid prescription, 5,111 (96%) had at least one perioperative opioid prescription, and 2,146 (40%) had at least one postoperative opioid prescription (Fig. 2). Average length of stay was 2.5 days. The most prevalent medical comorbidities were hypertension (58% of patients), depression (32%), anxiety (30%), and obesity (25%), Table 1.
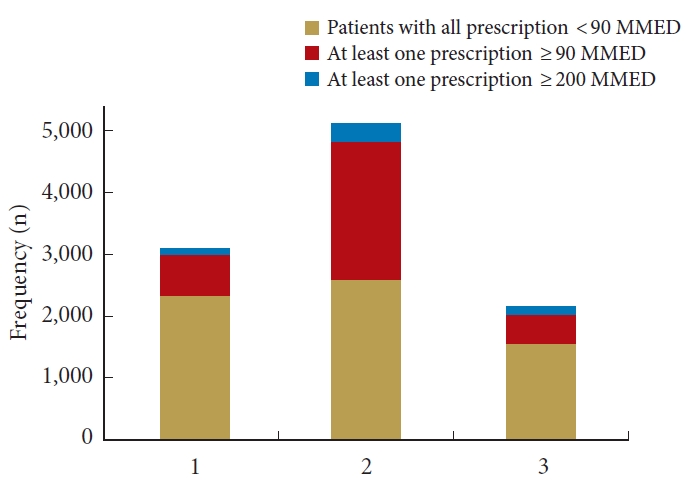
Proportion of patients receiving high-dose (≥90 MMED) and very high-dose (≥ 200 MMED) opioid prescriptions in the preoperative, perioperative, and postoperative period surrounding lumbar discectomy. In the preoperative period, 3,105 of patients (58%) received at least one opioid prescription, with 636 of these patients (20%) receiving at least one high-dose opioid prescription (≥ 90 MMED) and 139 of patients (4.5%) receiving at least one very high-dose opioid prescription (≥ 200 MMED). In the perioperative period, 5,111 of patients (96%) received at least one opioid prescription, with 2,217 of these patients (43%) receiving at least one high-dose opioid prescription (≥ 90 MMED) and 302 of patients (5.9%) receiving at least one very high-dose opioid prescription (≥ 200 MMED). In the postoperative period, 2,146 of patients (40%) received at least one opioid prescription, with 461 of these patients (21%) receiving at least one high-dose opioid prescription (≥ 90 MMED) and 129 of patients (6.0%) receiving at least one very high-dose opioid prescription (≥ 200 MMED). MMED, morphine milligram equivalents daily.
2. Trends and Patterns of Opioid Prescribing
Overall, 1,198 of patients (23%) were using opioids chronically following lumbar discectomy from 2010 to 2015. Of these patients, 952 (79%) had at least one opioid prescription filled prior to surgery, and 246 (21%) did not have any opioid prescriptions filled prior to surgery.
1) Temporal trends
This proportion of patients using opioids chronically decreased significantly over time from 27% in 2010 to 17% in 2015 (p < 0.001). In addition, the proportion of patients receiving high and very high-dose opioid prescriptions decreased significantly from 2010 to 2015. The proportion of high-dose opioid prescriptions decreased from 59% in 2010 to 43% in 2015 (p < 0.001), and the proportion of very high-dose opioid prescriptions decreased from 26% in 2010 to 19% in 2015 (p = 0.002). The duration of postoperative opioid use was 98 days (IQR, 29–356), which decreased significantly from 211 days (IQR, 29–256) in 2010 to 44 days (IQR, 10–294) in 2015 (Table 2).
2) Regional trends
Out of 5,315 patients, 5,287 (99%) had an identifiable region and were included in the analysis of regional trends in opioid prescribing. There was no significant variation in the prevalence of chronic opioid use, high/very high-dose opioid prescriptions, or the duration of postoperative opioid use among US regions (Table 3).
3. Univariate and Multivariate Regression Analysis of Chronic Postoperative Opioid Use
On univariate analysis, factors significantly associated with chronic postoperative opioid use included preoperative opioid use, drug abuse, depression, anxiety, surgery in the West, South, or North Central regions, tobacco use, if there was a 30-day hospital readmission, chronic obstructive pulmonary disease (COPD), age 45–54 and hypertension (Table 4).
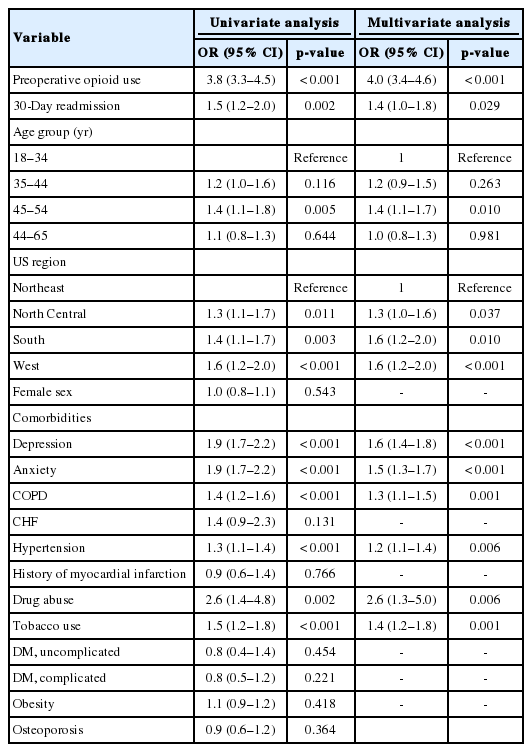
Univariate and multivariate analysis of factors of interest in association with chronic postoperative opioid use following lumbar discectomy
In order of decreasing odds ratios, the factors independently associated with chronic opioid use were preoperative opioid use (OR, 4.0; 95% confidence interval [CI], 3.4–4.6); drug abuse (OR, 2.6; 95% CI, 1.3–5.0); depression (OR, 1.6; 95% CI, 1.4–1.8), surgery in the Western (OR, 1.6; 95% CI, 1.2–2.0), or Southern (OR, 1.6; 95% CI, 1.2–2.0) United States; anxiety (OR, 1.5; 95% CI, 1.3–1.7); if there was a 30-day readmission (OR, 1.4; 95% CI, 1.0–1.8); age 45–54 (OR, 1.4; 95% CI, 1.1–1.7); tobacco use (OR, 1.4; 95% CI, 1.2–1.8); COPD (OR, 1.3; 95% CI, 1.1–1.5); surgery in the North Central United States (OR, 1.3; 95% CI, 1.0, 1.6); and hypertension (OR, 1.2; 95% CI, 1.1–1.4). All variables significant on univariate analysis were also significant on multivariate analysis.
DISCUSSION
In the present study of 5,315 patients undergoing primary lumbar discectomy, we found that a significant proportion (23%) of patients were prescribed opioids long term and of these, 21% were not using opioids prior to surgery. Encouragingly, between 2010 and 2015, the prevalence of chronic opioid use in this population decreased by 10%, the median duration of opioid use decreased by more than half, and the proportion of high-dose and very high-dose prescriptions reduced significantly. Additionally, we found the strongest independent risk factors for chronic postoperative opioid prescription to be preoperative opioid use, drug abuse, depression, and anxiety - among others.
Primary lumbar discectomy is highly successful at providing pain relief when indicated in patients affected by lumbar disc herniation and is usually performed as an outpatient procedure. Complication rates following this procedure are typically low [3-6], and a small proportion of patients may have recurrent pain or herniation [1]. Previous studies have examined risk factors for chronic opioid use in patients undergoing spine surgical procedures, and found similar risk factors to those in our study, with preoperative opioid use and mental health disorders being among the strongest and most consistent predictors of chronic opioid use [20,21,25]. Our study provides further insight into the specific risk factors for chronic opioid use in lumbar discectomy specifically, as risk factors for chronic opioid use following this procedure have not been well outlined in the literature. Though several of the risk factors identified in our study are supported by other, more broad studies in the literature, medical comorbidities such as COPD and hypertension are unique to our study. We have also highlighted national trends that span a time period of important developments in the US opioid epidemic.
Although our retrospective study cannot determine a causal relationship between preoperative opioid use and chronic postoperative opioid prescription, it has been suggested that weaning patients off of opioids prior to surgery may reduce postoperative opioid requirements [26]. In our study, a majority of patients who used opioids chronically following surgery were also using opioids preoperatively (79% of patients), and subsequently we identified preoperative opioid use as being independently associated with 4-fold increased odds of chronic opioid use following lumbar discectomy. Thus, it may be advantageous to consider limiting and avoiding preoperative opioid prescriptions when possible, and instead relying on the use of nonsteroidal anti-inflammatory medications which have been shown to be equally effective at treating back pain and back-related disability [27]. Other significant risk factors of persistent opioid use include anxiety and depression—both are important diagnoses within the biopsychosocial model that have been shown to exacerbate the pain response [28,29]. Anxiety and depression have been previously identified to be risk factors for substance abuse and pain syndromes, and we found these conditions to be independent predictors of chronic opioid use following lumbar discectomy. Thus, findings from this study contribute to the possibility that patients with poorly managed psychiatric conditions may benefit from a formal preoperative evaluation and/or treatment prior to lumbar discectomy surgery.
Our study also found there to be regional variation in the proportion of patients who use opioids chronically following surgery, with the highest rates in the Western and Southern regions of the US. Previous studies of geographic variation in opioid prescriptions have also found the Southern and Western regions to have higher prescribing rates [30,31]. Several hypotheses have been suggested for this variation, such as differences in opioid prescribing legislation [12-14], and state prescription drug monitoring programs [32]. In addition, factors such as race/ethnicity and socioeconomic status may play a role in the regional differences we identified [33,34]. Thus, investing in programs personalized to the needs of each region and state, along with developing more uniform guidelines and physician education, may be key to achieving more uniform control of postoperative opioid use.
With the high prevalence of opioid dependence in patients with back pain and declining but still significant opioid use for patients undergoing spine surgery, understanding opioid prescription in patients with spinal pathology remains central to balancing the need to reduce overprescribing while ensuring patients have access to optimal pain control [2,20,21]. This detailed analysis of opioid prescribing patterns after lumbar discectomy, one of the most commonly performed spine procedures, provides valuable insight to the progress that is largely driven by opioid prescribing guidelines (such as the CDC guidelines [35]), cultural shifts and public awareness on part of patients, and legislation. Between 2010 and 2015, we found that chronic opioid prescriptions after lumbar discectomy decreased in not only prevalence but also in duration and dose. Nevertheless, 17% of all patients during this timeframe were still using opioids after 3 months postoperatively—with more than half receiving high to very high-dose opioid prescriptions, demonstrating a patient group with the potential for improvement. The decreased opioid prescription is in-line with a national trend in declining opioid use among US adults during the same timeframe,36 which has been attributed largely to health policy initiatives and prescribing guidelines issued around this time [36,37].
Practice guidelines and educational initiatives developed from our results may be distributed to not only surgeons, but also primary care physicians. In addition, our results provide substance for guidelines and legislature that may be implemented to improve prescription habits in patients with a high risk of chronic opioid use. For example, patients who are using opioids preoperatively, or patients with certain medical comorbidities. Finally, the data provides independent risk factors for chronic opioid use that should be examined on an individual basis for patient education, counseling of expectations, preoperative optimization, and development of multimodal pain regimens. While the potential exists for decreased comfort or satisfaction with decreased postoperative opioid prescription, several studies have demonstrated that multimodal pain regimens and goal-directed decreases in postoperative opioid prescription following orthopedic surgical procedures many not negatively affect outcomes or patient satisfaction [38-40].
While our study has the strength of utilizing a large, national cohort of patients with a comprehensive assessment of detailed quantification of opioid prescription, there are several potential limitations that should be noted. As a retrospective study with rigorous selection criteria, many patients who underwent lumbar discectomy in the database were not included in the final analysis (Fig. 1). Thus, the potential for selection bias exists and our results should be interpreted in the context of our specific patient population. Follow-up was limited to 1 year, and we were not able to stratify patients by demographic variables such as race/ethnicity. The nature of administrative claims data also prevented analysis of certain granular data that would be valuable for future studies to analyze. For example, anxiety and depression may have been present in some patients without a formally coded and identifiable diagnosis within our database, anxiety and depression were also classified as binary variables, though these conditions are inherently heterogeneous in their severity. The data source also precluded analysis of single versus multilevel discectomy, postoperative patient-reported outcomes, and specific indications for opioid prescription. Further, it is important to note that opioid prescription was used as a proxy for opioid use, similar to other studies on this topic [23,41]. Lastly, the cohort included in the database only consists of private payers under age 65 who have prescription coverage, most of whom are employed. The external validity may not be applicable to older patients and those who are uninsured or covered by government programs.
CONCLUSION
The prevalence, dose, and duration of chronic opioid prescriptions following primary lumbar discectomy have declined from 2010–2015. However, 1 in 5 patients is still dependent on long-term opioids postoperatively. Factors independently associated with long-term opioid use included preoperative opioid use, drug abuse, depression, surgery in the Western/Southern US, anxiety, and a 30-day readmission. Recognition of these risk factors enables appropriate preoperative optimization, pain management, patient education, and setting expectations that have the potential to reduce the incidence of chronic opioid use postoperatively.
Notes
Dr. Bicket reports Axial Healthcare (past service on advisory board, stock options) and Alosa (advisory board). Except for that, the authors have nothing to disclose.
SUPPLEMENTARY MATERIALS
Supplementary Tables 1-2 can be found via https://doi.org/ns.2040122.061.
ICD-9-CM and CPT codes used in cohort definition
ICD-9-CM codes used to identify medical comorbidities




