Upper Cervical Spine Trauma: WFNS Spine Committee Recommendations
Article information
Abstract
Craniovertebral junction (CVJ) trauma is a challenging clinical condition. Being a highly mobile functional unit at the junction of the skull and the vertebral column, traumatic events in this area may produce devastating neurological complications and death. Additionally, many of the CVJ traumatic injuries can be left undiagnosed or even raise difficult treatment dilemmas. We present a literature review in the format of recommendations on the diagnosis and management of different scenarios for upper cervical trauma and produce recommendations, which can be applicable to various areas of the globe.
INTRODUCTION
The upper cervical spine, including C0–C1–C2, is a unique anatomical and functional unit. The anatomical orientation of C0–1 and C1–2 joints, constrained by a unique array of ligaments, originates the most mobile segment of the all spine. Contrary to the subaxial spine, C1 and C2 vertebra have rather peculiar forms and do not bear weight through disks, but rather synovial joints. Craniovertebral Junction (CVJ) functions as a single mobile unit with atlas acting like a washer between cervical spine and occiput. However, CVJ motion segments present different mechanical properties: C0–1 is primarily determined by bony structures and it is responsible for 25% of cervical spine flexion-extension, whereas C1–2 is determined by ligamentous structures accounting for 50% of cervical spine axial rotation [1].
Upper cervical trauma usually results from high-energy events such as falls, sports injuries, motor vehicle crashes, and diving accidents. The unique features of CVJ fabricate a myriad of different fractures and/or ligament injuries leading to instability and putting the spinal cord and the vertebral artery at risk. These traumatic injuries can sometimes be very difficult to diagnose, to manage, and to treat. This paper presents the World Federation of Neurosurgical Societies (WFNS) Spine Committee recommendations with a worldwide applicability on the diagnosis and treatment of different upper cervical trauma settings in order to standardize patient care and improve clinical outcomes.
MATERIALS AND METHODS
WFNS Spine Committee designed a consensus conference to work on the diagnosis, classification, management, and treatment of upper cervical spine trauma, in order to generate evidence-based recommendations for global applicability.
A group of expert spine surgeons (SHK, VM, AG, OLA, WCP, NS) reviewed the pertinent literature from 2009 to 2019 on upper cervical trauma and presented their search in Moscow and Peshawar, in May 2019 and November 2019, respectively. For didactic reasons the topics were divided on: Radiologic Assessment of Upper Cervical Trauma, Occipital Condyle Fractures (OCF), Atlanto-occipital Dislocation (AOD) Injuries, Isolated Atlas Fractures, Odontoid Fractures, Hangman Fractures, and Combined Atlas and Axis Fractures: classifications and management
Each of them formulated topic-related questions and statements that were discussed and voted according to the Delphi method to establish evidence-based consensus.
Data sources included relevant citations for systematic reviews, meta-analyses, reviews of clinical trials, evidence-based medicine, consensus development conferences as well as guidelines in the English language literature identified through searches in PubMed database with the pertinent keywords.
The questions to be answered were:
1. Radiologic Assessment of Upper Cervical Trauma
1) What are the most appropriate diagnostic tests for upper cervical spinal trauma?
2) Which radiologic criteria on plain radiographs best describes instability in upper cervical spinal trauma?
2. Occipital Condyle Fractures: Classification and Management
1) For the classification and management of OCF does the Anderson and Montesano classification provides the best algorithm?
2) What is the recommended imaging tool for diagnosis and management of OCF?
3) What is the best imaging tool to assess the integrity of craniovertebral ligaments in OCF?
4) What is the most appropriate treatment for OCF?
3. AOD Injuries: Classification and Management
1) Is computed tomography (CT) obligatory for the establishment of craniovertebral injury in patients with suspicion of AOD?
2) In order to diagnose AOD, is it necessary to perform a cervical CT in all patients after high-energy accidents, especially if they have severe traumatic brain injury (TBI), lower cranial nerves deficits, or spinal cord injury for the diagnosis of AOD?
3) Is it necessary to treat all patients with AOD surgically?
4. Isolated C1 Fractures: Classification and Management
1) What are the radiographic criteria used for prompt diagnostic evaluation?
2) What are the appropriate classifications to identify subtypes of fractures?
3) Which criteria should guide a specific treatment for isolated C1 fractures?
5. Odontoid Fractures: Classification and Management
1) Which radiologic criteria on plain radiographs best describe instability of atlantoaxial joint from odontoid fracture?
2) For a type II odontoid fracture, what are the predisposing factors for fracture nonunion after C1 lateral mass screws were combined with C2 pedicle/laminar screws?
3) What are the risk factors associated with fusion failure after anterior odontoid screw fixation?
6. Hangman’s Fractures: Classification and Management
1) Besides CT scan, is upright x-ray mandatory to evaluate Hangman’s fracture?
2) Is surgery indicated for Levine IIa Hangman’s fracture?
3) Does Levine type III Hangman’s fracture need both anterior and posterior surgery?
4) Is halo-vest indicated for any Hangman’s fracture?
7. Combined Atlas and Axis Fractures: Classification and Management
1) Is there a high-class evidence for the treatment of combined atlas-axis fractures?
2) Should we recommend external immobilization in most of cases of C1–2 combination fractures?
3) Should we consider surgical treatment for cases in which C1-type II odontoid combination fractures with an atlantodental interval of ≥ 5 mm and C1-Hangman combination fractures with C2–3 angulation of ≥ 11°?
RESULTS
1. Radiologic Assessment of Upper Cervical Trauma
The following key words, “radiologic assessment” and “cervical spine trauma,” were used as search items. The search done on PubMed revealed 82 results, from which 39 papers were removed because they were published >10 years ago. We also removed 43 studies because they were case reposts, in languages other than English and not relevant, and examined only 8 were in terms of evidence-based criteria.
Since injury at upper cervical spine can have devastating consequences, instability should be suspected in all patients with high-energy injuries. Besides routine systemic and neurologic assessment performed according to the Advanced Trauma Life Support Guidelines, a single cross-table lateral plain radiograph remains an acceptable first-line radiographic screening tool, assuming that the entire cervical spine can be visualized. For the past decade, however, fine-cut CT with sagittal and coronal reconstructions plays a key role in diagnosis and surgical planning and has replaced plain radiography as the first-line study for screening of the cervical spine in many institutions, mainly because of its higher sensitivity for diagnosis [2]. An open-mouth odontoid view or coronal CT reformats of the upper cervical spine, provide an anteroposterior (AP) projection in which the occipital condyles, lateral masses of C1, and the odontoid process are visualized. Any deviation from these initial screening measures should prompt further evaluation. Flexion-extension radiographs to check on instability provide little additional information and may increase the risk of neurologic injury. Cervical myelographic CT may be helpful, especially when magnetic resonance imaging (MRI) is contraindicated or unavailable, particularly in the presence of neurologic deficits. MRI is useful to evaluate the severity of spinal cord injury or nerve compression but is less accurate at detecting a fracture than a CT scan. Ligament disruptions of the upper cervical spine, namely rupture of the transverse atlantal ligament (TAL), which is a key element in C1–2 stability, can be well demonstrated by fatsuppressed T2-weighted or short T1 inversion recovery images, but only if performed within several days of the acute injury [3].
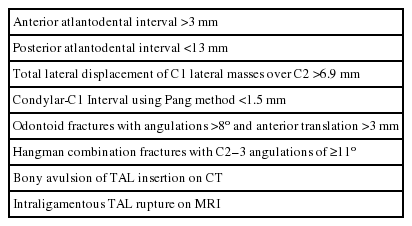
Concerning the radiological criteria of instability, anterior atlantodental interval (AADI) is considered normal if ≤ 3 mm in adults and child ≤ 5 mm in children, and posterior atlantodental interval (PADI) is normal if ≥ 13 mm. An AADI ≥ 5 mm denotes a rupture of TAL and accessory stabilizing ligaments. If 3 mm < AADI < 5 mm, TAL must be attenuated. It is worth noting that with an intact TAL, complete bilateral C1–2 dislocation can occur at 65° of rotation, whereas with a disrupted TAL, dislocation can occur at 45° of rotation. Additionally, according to the rule of Spencer, a total lateral displacement of the lateral masses of C1 over the masses of C2 > 6.9 mm (7 mm) in AP or open-mouth is indicative of C1 burst fracture or rupture of the TAL [3]. Table 1 presents a summary of validated criteria defining upper cervical spine instability.
In line with the literature review, the WFNS Spine Committee proposed and voted upon the statements as follows:
Statement 1: In patients with history and physical examination findings suspecting with cervical spinal trauma, cervical CT plays an integral role in diagnosis and surgical planning as the first-line study for screening of the cervical spine. This statement got a strong consensus (yes: 95%; no: 5%).
Statement 2: AADI > 3 mm or PADI < 13 mm indicate a possible TAL disruption and instability in C1–2. This statement reached a full 100% consensus.
Statement 3: Before placement of screws at upper cervical spines in patients with cervical trauma, preoperative 3-dimensional (3D) CT scanning should be performed to rule out anatomical bony abnormalities. This statement reached a full 100% consensus.
2. Occipital Condyle Fractures: Classification and Management
OCF generally occur with axial trauma and are almost always unilateral (> 90%). The incidence of OCF has been estimated to be between 1% and 3% of blunt craniocervical trauma cases and their treatment remains controversial [4].
For this reason, a PubMed search with the keywords “occipital condyle fracture” and “humans” displayed 21 articles published in English after 2008. Of these, 2 were systematic reviews, 5 case series, 12 case reports, and 1 comment to the editor.
The historical classification of Anderson and Montesano (based solely on 6 retrospective patients) and, more recently, the modified classification of Tuli (based on only 3 own retrospective cases) are mainly of academic interest, as they contribute marginally to the clinical decision-making process [4]. The newer classification system by Mueller et al. [5] is more useful in the treatment algorithms of OCF, as it identifies AOD, craniocervical misalignment, and neural element compromise, which are of paramount significance for treatment planning. It establishes 3 types of OCF, unilateral as type 1, bilateral as type 2, OCF with AOD as type 3.
Only 20 cases of OCF had been documented until 1988, because plain radiographs (usually open-mouth radiographs) have an unacceptably low sensitivity (estimated to be 3.2%). CT imaging with reconstruction views is recommended to establish the diagnosis of OCF (level II recommendation). An MRI is recommended to assess the integrity of the craniocervical ligaments for determining the stability of OCF (level III recommendation) [6].
The small amount of cases explains the variety of different treatment recommendations, ranging from conservative therapy with neck immobilization to surgical fusion (level III evidence) [7]. In a retrospective study (n = 23), Byström et al. [8], using the Mueller classification, found no unstable patients. Consequently, they recommended 6 weeks treatment with nonrigid orthosis (cervical collar) for unilateral OCF, or a more rigid external immobilization in a halo-vest device for bilateral OCF both without AOD (level III recommendation). Type 2 OCF is associated with higher comorbidity and mortality than unilateral OCF without AOD. A dynamic flexion-extension radiograph together with a clinical examination should be performed before ending treatment. If AOD has been diagnosed in addition, it requires surgical occipitocervical stabilization— independently of the OCF type—and it is a significant predictor for poor outcomes (level III recommendation) (Table 2) [9].
According to the literature review, the WFNS Spine Committee proposed and voted upon the statements as follows:
Statement 1: Classification system proposed by Mueller et al. may be preferable in the management of OCF. This statement got a strong consensus (yes: 95%; no: 5%).
Statement 2: CT imaging should better be used to establish the diagnosis and management of OCF. This statement reached a full 100% consensus.
Statement 3: MRI, in addition to CT scan, is recommended to assess the integrity of the craniocervical ligaments for determining the stability of OCF. This statement reached a full 100% consensus.
Statement 4: Conservative treatment should be preferred to surgical treatment in OCFs without AOD. This statement reached a full 100% consensus.
3. AOD Injury
AOD, found in 10% of all fatal cervical spine injuries and more than 30% of motor vehicle accidents fatal cases, is the most severe type of injury of the craniocervical region. Seventy percent of cases can be accompanied by brain and spinal cord injury and severe neurological deficits, which make it difficult to diagnose. This condition is extremely unstable and delay in surgical treatment can cause a significant increase in neurological deficit, up to development of a fatal outcome [10]. The Congress of Neurological Surgeons published the latest recommendations regarding AOD management in 2013. Thus, the main goal of our study was to perform an updated review of current concepts for classifications and management of AOD. A PubMed search was performed for articles in English language released after 2009 using the key words: (“occipitocervical” or “occipito-atlantal” or “atlanto-occipital”) and (“dislocation” or “instability” or “dissociation”). The initial data selection consisted of 564 paper abstracts. A total of 95 full texts were chosen for study, but only 14 papers published after 2009 were considered for detailed analysis.
According to current recommendations, lateral radiography can be recommended as a diagnostic tool for AOD. However, in the study of Theodore et al. [11], the sensitivity of radiography in detecting AOD for children and adults was 50.5%, and was associated with neurological deterioration after admission in 18.5% of all patients who initially underwent radiographic evaluation. Of these 28 patients, 10 had neurological deterioration and accounted for 18.5% of all patients who initially underwent radiographic evaluation. Soft tissue swelling was mentioned on radiographs in 30 patients (55.5%), indicating a sensitivity in the diagnosis of AOD of 69%. However, CT was much more sensitive and allowed correct diagnosis in 94.6% of the cases. MRI was done to clarify the diagnosis in a residual amount of patients in whom the AOD was minimal. MRI revealed damage to joint capsules and tectorial membranes, as well as prevertebral soft tissue swelling.
Several methods for detecting AOD are described in the literature: powers ratio (> 1), Wholey line - Basion-Dental Interval (BDI) < 12 mm, Harris method (combined BDI with Basion-Axis Interval [BAI]), X-line method, and Pang method. Regarding the sensitivity and specificity of these methods, the values are significantly higher when performing CT than x-ray. Nevertheless, some methods significantly depend on the stability of the atlantoaxial complex (X-line, BDI, BAI), so the values may differ significantly in the case of dislocation in the C1–2 segment. Thus, only condyle-C1 Interval (CCI) and condylar sum had consistently high sensitivity and specificity, and only CCI determined by the Pang method had 100% sensitivity and specificity (class I evidence) [6]. Moreover, there the authors have found a significant interobserver variation: agreement was absolute only for CCI, whereas or BDI, BAI, X-lines, and powers, the Kappa values were significantly lower (0.57, 0.25, 0.25, and 0.20 respectively) [12]. The only optimal method for determining AOD was the CCI using Pang method or condylar sum calculation, which had not only 100% sensitivity and specificity, but also allowed to achieve absolute interobserver agreement. Taking into account the sensitivity of data obtained from various research methods, cervical spine CT is indicated for all such patients (class I evidence). If implementation of CT is impossible, lateral radiography of the cervical spine with the definition of BAI and BDI in accordance with the Wholey or Harris methods is recommended for patients after a high-energy injury (class III evidence). Soft tissue swelling at the x-ray should indicate an AOD until a CT scan of the cervical spine is performed. In this case, it is necessary to take into account the probability of a false-positive result when the atlantoaxial level is unstable. The presence of soft tissue swelling may indicate damage in the C0–1 segment. MRI is necessary in the absence of dislocation to assess the extent of damage to the ligamentous complex.
To date, the question of applying the AOD classification remains unresolved. Traynelis classified AOD into 4 types: type I (anterior), type II (longitudinal), type III (posterior), and “other” (complex). This classification does not allow an adequate assessment of the injury, since the relative position of the condyles and C1 may depend on the head position. Given the extreme instability of the injury, all 3 types can occur in one patient depending on the head placement, so this classification is not of great clinical significance. However, the most simple and rational scale is Horn’s scheme, based on CT and MRI findings, that allows a clear conclusion about the stability of the injury and the need for surgical treatment [11].
1) Treatment of AOD
Traction as the primary method of treatment was reported in older papers in 3 adult patients. Two of them died, and the third one had deterioration in neurological status. The lack of immobilization of the cervical spine or the use of traction is associated with a high chance of deterioration of the patient’s condition. As a primary treatment, the use of a halo-vest device is more effective than brace (collar). However, any external immobilization in patients with AOD is recommended only until the moment of patient's vital functions stabilize, after which it is necessary to perform surgical treatment, or such cases when surgery could not be performed for various reasons (class III evidence).
As reported in the literature, most patients had surgery as the primary treatment method with a significant improvement, around 75%, at the final follow-up among survivors. Therefore, the optimal method of treatment for adult patients with AOD is surgery [13]. The treatment of choice in most cases of traumatic AOD is posterior occipitocervical fusion, which can be done using a variety of techniques including posterior wiring and structural grafting and screw fixation with structural grafting.
According to the literature review, the WFNS Spine Committee proposed and voted upon the statements as follows:
Statement 1: CT can be enough to define CCI in patients with suspicion of AOD. This statement got a positive consensus (yes: 72%; no: 28%)
Statement 2: In case of severe TBI, lower cranial nerves deficit and/or spinal cord injury an AOD may be suspected. This statement reached a full 100% consensus.
Statement 3: Cervical traction is not recommended for AOD. This statement got a positive consensus (yes: 92%; no: 8%).
Statement 4: Patients with AOD should be operated for occipitocervical fixation, as the general condition of the patients is stable. This statement reached a full 100% consensus.
4. Isolated C1 Fractures: Classification and Management
Using the key word “atlas fracture,” a PubMed search provided 728 references that were filtered for “classification and management.” As atlas fractures account for approximately 1% to 2% of all fractures of the spinal column, most of the articles found were very small number of case series and numerous case reports. We were unable to find class I or II studies comparing conservative and operative management or studies matching different operative treatment strategies. Recommendations made are based on 18 studies with class III medical evidence case series and on expert opinion of WFNS Spine Committee members.
Cervical spine x-rays remain the first-line diagnostic tool to identify isolated atlas fractures. Nevertheless, this type of fractures might often be overlooked on the x-ray. The management of C1 fractures is based on the integrity of the transverse ligament that can be assessed indirectly with several radiological measures. The sum of lateral mass displacement of C1 over C2 > 6.9 mm in the open mouth AP x-ray means that the TAL is probably damaged – the “rule of Spence.” However, this rule has shown to be inaccurate for assessing the integrity of the TAL, as 60% of patients with a TAL rupture would not have met the “rule of Spence” criteria. MRI is a more sensitive indicator of TAL integrity/disruption than the rule of Spence. An additional criterion for instability is the AADI in lateral x-ray. If this interval is > 3 mm, it means that there is an atlantoaxial translation, which indicates instability [14].
CT is always necessary to evaluate the integrity of the atlas ring and to classify an atlas fracture between stable and unstable burst fractures. Axial CT slices can detect a bony avulsion of TAL as a criterion for a potential instability. If a dislocation of the C1 lateral mass is obvious and the CT was unable to detect a bony avulsion of TAL, MRI is recommended to evaluate TAL integrity. With the transverse process fracture of C1, an angioCT or angio-MRI is recommended to exclude vertebral artery lesion [15].
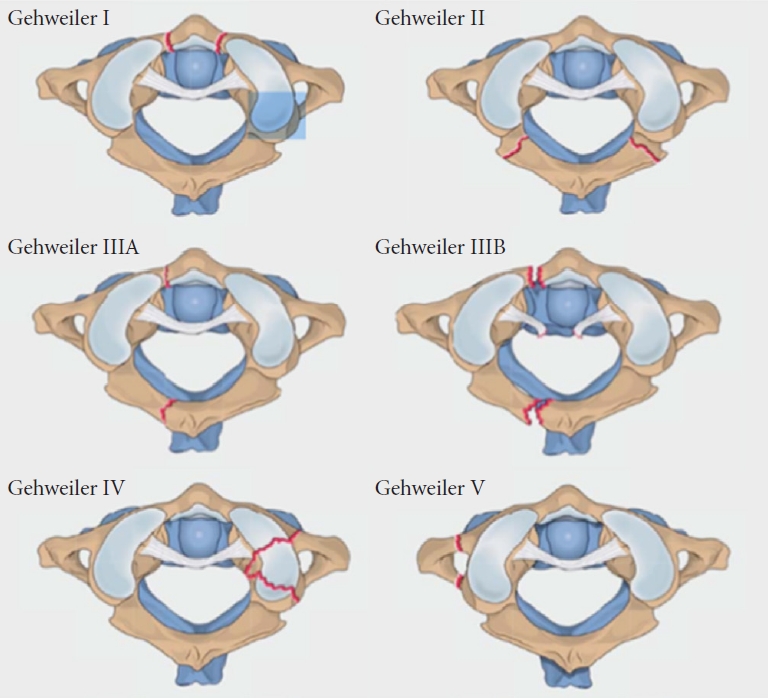
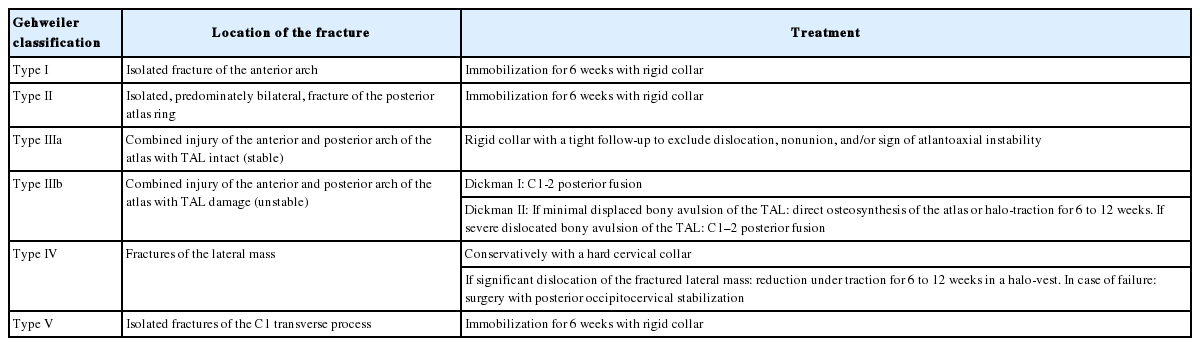
Regarding the classification systems, the Jefferson classification relates the mechanism of injury with the type of fracture, whereas the Dickman classification focus on the integrity of the TAL and degree of dislocation of the bony avulsion fragment from the lateral mass, which is important to define surgical treatment options. However, the Gehweiler classification, because it integrates categories of the previous classifications, is far more useful for treatment decision (Fig. 1) [16].
An old study by Fowler et al. [17], enrolling 48 patients, provided class III evidence for conservative treatment of atlas fractures independently of the lateral mass distance. Kontautas et al. [18] studied 17 patients with isolated atlas fractures, out of 29 patients with upper cervical spine injuries, and observed an overall fusion rate of 96,4%. Stable fractures (n = 13) were treated with immobilization (neck collar) and all achieved a successful union, whereas unstable fractures (n = 4) were managed with halo-vest immobilization, but 1 of them (25%) failed to heal. Longo et al. [19], in a systematic review concluded that 6 to 12 weeks of halo-fixation after reduction under traction is advised to manage unstable atlas fractures with efficacy and safety predominantly with Dickman type II lesion to avoid fusion loss of motion and surgical complications.
The treatment of C1 fractures is influenced by the presence of concomitant cervical spine injuries, but still remains controversial. The first study to address the quality-of-life issues revealed that the presence of an unstable atlas fracture was associated with a worse outcome at long-term follow-up (mean, 75 months; range, 19–198 months), compared with those who sustained a stable atlas fracture (class III evidence). Nonetheless, due to its retrospective nature, the cross-sectional outcome assessment showed a relatively low response rate (60%) [20]. Regarding conservative treatment, due to the fact that there is no evidence suggesting the superiority of any form of external immobilization (halo, hard collar, soft collar) over another, the one with the lowest complication rate might be the best. It is known that the halo-traction, as well as fixation in a halo-vest is an invasive form of conservative fracture management not without risks for the patient. Complications of halo-vest are documented such as fracture redislocation, screw loosening, and the discomfort for the patient, especially in elderly patients [19].
Surgical treatment is recommended when there is an atlas fracture associated with atlanto-occipital instability and an intraligamentous rupture of the TAL. In a study, analyzing 8 patients with unstable atlas burst fractures, which is a fracture of the anterior and posterior arches associated with rupture of the TAL and an incongruence of the atlanto-occipital and the atlantoaxial joints, 63% of patients (5 of 8) were initially treated with immobilization, but later, they required a transarticular screw fixation. After that, all 8 patients required surgical stabilization and all achieved bony fusion [21]. Gehweiler types 1, 2, and 5 require cervical spine immobilization for 6 weeks using a hard cervical collar. In type 5 fracture, involving the transverse foramen, a vertebral artery lesion has to be excluded by angio-CT or angio-MR. Gehweiler type 3a is a stable fracture with ligament intact, and it demands conservative therapy that is a hard collar. Later follow-up to exclude dislocation, nonunion, and/or signs for atlantoaxial instability is mandatory. In unstable Gehweiler type 3b fracture with intraligamentous TAL rupture (Dickman type I) warrants atlantoaxial fusion, if the unlikelihood of ligamentous healing may potentially result in posttraumatic translational atlantoaxial instability (class III evidence). In unstable Gehweiler type 3b fracture with dislocated bony avulsion of the TAL (Dickman type II), if there is minimal dislocation of bony avulsion fragment that heals to the lateral mass after atlas ring fixation creating a stable atlantoaxial complex direct osteosynthesis of atlas or halo-traction is recommended for 6 to 12 weeks. If the dislocation is severe or translatory atlantoaxial instability develops after conservative management, atlantoaxial fusion is currently the treatment of choice because the severely displaced bony avulsion fragment may not heal to the lateral mass, ultimately resulting in an unstable atlantoaxial complex (class III evidence). In Gehweiler type 4 fractures, as most of them are minimally displaced a hard cervical collar is adequate. In the rare case of significant dislocation of fractured lateral mass, resulting in either incongruence of the atlanto-occipital and atlantoaxial joint or in local scoliotic deformity, a reduction under traction and retention for 6 to 12 weeks in a halo-fixator in young patients is acceptable. After initial reduction and after 3, 6, and 12 weeks under halo-traction, a CT evaluation is necessary to confirm an accurate realignment and to assure fracture healing. In case of inadequate initial reduction under halo-traction or early redislocation, surgery is indicated in order to maintain reduction [20]. Atlantoaxial fusion can be performed either by transarticular C1–2 screw fixation or posterior screw and rod fixation according to Harms (Table 3).
In accordance with the literature review, the WFNS Spine Committee proposed and voted upon the statements as follows:
Statement 1: Treatment of isolated fractures of atlas should be based on CT and MRI criteria, in order to define the fracture type and the integrity of the TAL. This statement got a positive consensus (yes: 74%; no: 26%).
Statement 2: The majority of atlas fractures is stable and is successfully managed conservatively. This statement reached a full 100% consensus.
Statement 3: Surgical indications for atlas fracture are atlanto-occipital instability, an intraligamentous rupture of the TAL, and any “unstable” atlas fracture. This statement reached a full 100% consensus.
5. Odontoid Fractures: Classification and Management
A PubMed search based on keyword “odontoid fracture” revealed 1,462 search results, from which 822 studies were published > 10 years ago and 640 studies were more recent ones. The 15 most relevant studies from an evidence-based perspective were selected for analysis.
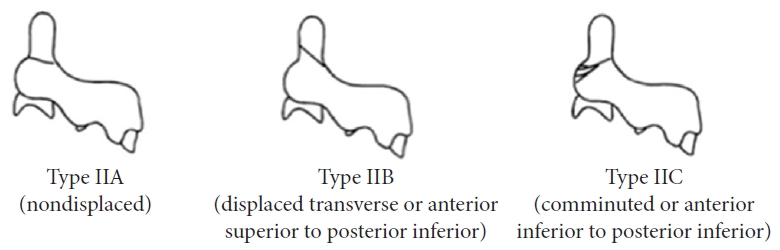
Odontoid fracture is a common cervical injury, representing about 20% of total cervical fractures [22]. Odontoid fractures were classified by Anderson and D’Alonzo into 3 types, focused on anatomy and the locations of the fracture line, without treatment guidelines. In 2005, Grauer et al. [23] proposed a modified treatment-oriented classification of odontoid fractures. This classification divided odontoid fractures into 3 groups (I, II, and III) and distributed type II fracture into 3 subtypes (IIA, IIB, and IIC) (Fig. 2).
According to Grauer’s classification, types I, IIA, and III of odontoid fractures are treated with external immobilization using halo-vest fixation or Philadelphia brace. Anterior screw fixation in type IIB and posterior atlantoaxial fusion in type IIC are usually the recommended ways of treatment for these fractures (Table 4). Cho et al. [22] reviewed 69 patients with odontoid fractures according to Grauer’s classifications and treatment guidelines. At the last follow-up, the overall fusion rate was 88.4% and there was a statistically significant improvement in neck visual analogic scale in types II and III fractures. Therefore, Grauer’s classification appears to be very meaningful to decide treatment plan for odontoid fractures, especially in type II odontoid fracture [22].
There are some measures to describe atlantoaxial joint instability. If the AADI is more than 3 mm in adults, it indicates TAL disruption and instability in C1–2, and if it is more than 5 mm, it means transverse ligament and accessory stabilizing ligament have ruptured [22].
In a retrospective study of 117 patients with type II odontoid fractures, Wang et al. [24] evaluated the predisposing factors of fracture nonunion after posterior C1–2 pedicle or translaminar fixation. Fracture nonunion was detected in 76 of those 117 patients (65%) at final follow-up. The logistic regression analysis revealed that advanced age (> 45 years), long duration of the fracture (> 2 months), and preoperative separation of the odontoid fracture (> 4 mm) were independently associated with the postoperative fracture nonunion. Cho et al. [25] designed a retrospective study, including 41 patients with a type II and rostral shallow type III odontoid fracture to analyze the risk factors associated with fusion failure after anterior odontoid screw fixation. Anterior odontoid screw fixation resulted in solid bony union in 33 patients (80.5%), fibrous union in 3 (7.3%), and nonunion in 5 (12.2%). The incidence of fusion failure significantly increased when surgery was delayed for more than 1 week (p = 0.0051). A fracture “gap” of 2 mm or more was found to be significantly associated with fusion failure (p = 0.0172). Patient age (p = 0.8236) and fracture displacement (p = 0.5762) were not found to be significantly associated with fusion failure [25].
According to the literature review, the WFNS Spine Committee proposed and voted upon the statements as follows:
Statement 1: In adult patients with odontoid fractures AADI > 3 mm indicates TAL disruption and instability in C1–2, while AADI ≥ 5 mm implies transverse ligament and accessory stabilizing ligaments ruptured. This statement reached a full 100% consensus.
Statement 2: Advanced age, long duration, and preoperative separation of odontoid fracture > 4 mm are predisposing factors for fracture nonunion after posterior C1 lateral mass screw combined with C2 pedicle/laminar screw fixation for type II odontoid fracture. This statement reached a full 100% consensus.
Statement 3: For anterior odontoid screw fixation, the interval from injury to operation and fracture “gap” are significantly associated with fusion failure. This statement reached a strong consensus (yes: 91%; no: 9%).
6. Hangman Fractures: Classification and Management
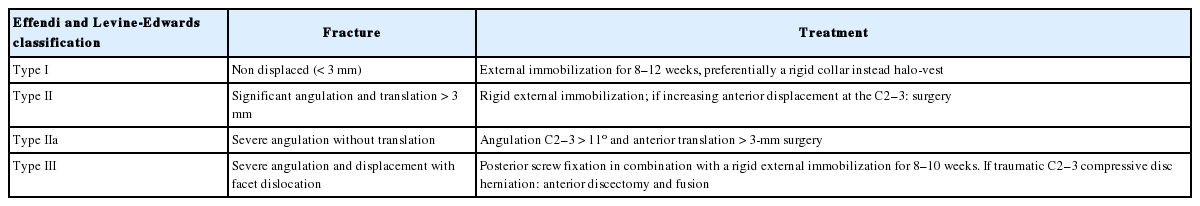
The classification systems proposed by Effendi et al., based on x-rays and clinical course, and modified by Levine and Edwards, based on the mechanism of injury, provide a clinically reasonable guideline for successful management of Hangman’s fractures. However, the surgical indications and the type of surgery for Hangman’s fracture are still controversial, particularly for type II and type III according to Levine and Edwards [26].
A PubMed search with the following keyword “Hangman’s fracture” focused on “classification and treatment”. All case reports were excluded. Most of the 20 studies retrieved were level III of evidence.
From the systematic review published by Murphy et al. [27] in 2017, among 548 fractures, 46 (8.4%) were type I, 228 (41.6%) were type II, 89 (16.2%) were type IIA, 35 (6.4%) were type III and 150 (27.4%) were not broken down by fracture type.
As reported by Li et al. [26] on their systematic review, most of patients with type I, Effendi type II, and Levine-Edwards type II fractures were treated conservatively, whereas the proportion of nonoperative patients in Levine-Edwards types IIa and III fractures were much smaller.
Another systematic review, including 25 studies, indicates a lower nonunion rate in surgical treatments compared to conservative treatment and no difference in mortality between treatments. As a consequence, treatment failure is less likely in surgical treatment (0.12%) than in nonsurgical treatment (0.71%). Both an anterior and a posterior approach result in high rate of fusion, and neither approach seems to be superior. The limitations of this review are the lack of analysis by fracture type, the absence of patient-reported outcome, and the poor data for halo because of application in more unstable fractures. Nonsurgical management is recommended for type I fractures with external immobilization for 8–12 weeks, preferentially a rigid collar instead of halo-vest due to its complications. For unstable type II fractures surgery is recommended, if the x-ray demonstrates an increasing anterior displacement at the C2–3 level in spite of rigid external immobilization. Further conditions necessitating surgical therapy include the dislocated type IIa fractures (angulation > 8° and anterior translation > 3 mm) and dislocated type II fractures (anterior translation > 3 mm). Type III Hangman’s fractures, lesions combined with a traumatic C2–3 disk herniation compromising the spinal cord, and established nonunions may also require surgery. Posterior screw fixation is not sufficient in cases of a traumatic disk herniation compromising the spinal cord. In this instance, an anterior C2–3 discectomy and fusion with optional plating is recommended. Type III fractures without traumatic disk herniation (excluded by CT or MRI) can be treated with posterior screw fixation in combination with a rigid external immobilization for 8–10 weeks in order to allow healing of the ligamentous system and to preserve the mobility of the C2-C3 segment (Table 5) [27].
According to the literature review, the WFNS Spine Committee proposed and voted upon the statements as follows:
Statement 1: For Hangman’s fracture upright x-ray performed under medical supervision may be useful besides CT scan. This statement reached a full 100% consensus.
Statement 2: For Levine IIA Hangman’s fracture surgery is recommended. This statement reached a full 100% consensus.
Statement 3: Levine type III Hangman’s fracture may require both anterior and posterior surgery. This statement reached a strong consensus (yes: 89%; no: 11%).
Statement 4: Conservative treatment for Hangman’s fracture should be performed with a rigid collar instead of halo-vest due to its complications. This statement reached a full 100% consensus.
7. Combined Atlas and Axis Fractures: Classification and Management
In 2002, the expert-based guidelines sponsored by the Joint Section on Disorders of the Spine and Peripheral Nerves of American Association of Neurological Surgeons, supported by class III medical evidence, recommended the management of combination C1–2 fractures based on the fracture characteristics of the axis fracture [28]. In order to update clinical evidence on the topic, a PubMed literature search for the last 10 years was undertaken using Medical Subject Headings in combination with “vertebral fracture”, “atlas”, “axis,” and “human.” This strategy yielded 268 references, from which 65 manuscripts, providing class III medical evidence, were reviewed.
In their systematic review of 47 reports, including a total of 1,078 patients with cervical spine fractures, Longo et al. [19] identified 50 patients with combination C1–2 fracture injuries (4.6%).
The paper of Maserati et al. [4], reporting on Dickman et al. experience, identified an incidence of neurological deficit of 12% at admission, compared with isolated incidence of C1 (0%) or C2 (2%). According to Dickman’s classification of Combined Atlas and Axis Fractures, 40% of C2 fractures were type II, 28% were miscellaneous C2 body, 20% were type III and 12% were Hangman. Regarding the type of C1 fractures, these were multiple ring (40%), posterior ring (28%), unilateral ring (24%), and lateral mass (8%).
As stated by Ryken et al. [29], there is no class I or class II evidence addressing the management of patients with combination atlas and axis fractures. Most, if not all, of the articles reviewed describe case series or case reports containing class III evidence supporting a variety of treatment strategies for these complex fractures. The treatment of combined atlas-axis fractures based primarily on the specific characteristics of the axis fracture is advised.
Overall, nonoperative therapy was the initial management strategy in 20 of 25 patients (84%), with halo orthosis or suboccipital-mandibular immobilizer (SOMI) brace, for a median duration of 12 weeks, achieving stability and fusion in 19 of 20 patients (95%). External immobilization failed in 1 patient, with an initial AADI of 5 mm who was treated with posterior C1–2 fusion. External immobilization with the halo-vest, SOMI, and Minerva devices of most C1–2 combination fractures is safe and effective, despite a decreased rate of bone union (class III evidence). Four patients were treated with early surgical stabilization and fusion based on an AADI> 5 mm. All patients treated surgically achieved stability using a posterior fusion technique (100%) [4].
In the report of Longo et al. [19] of those patients treated with a halo-vest, 42% died compared with a 20% mortality rate among patients not treated in a halo device (p = 0.03). The incidence of major complications in the halo-treated group was 66% when compared with 36% in the non-halo group (p = 0.003). Clearly, morbidity and mortality appear to be magnified with the use of a halo immobilization device.
C1-type II odontoid combination fractures generated the most controversy. Fractures with AADI < 5 mm (n = 6) have been successfully managed with rigid immobilization (halo, SOMI, Minerva) with 83% success rate (n = 5/6) [4]. However, fractures with AADI > 5 mm had also been successfully managed with early surgical stabilization and fusion. If instability is present in this subtype of fractures, as denoted by an AADI > 5 mm, a high failure rate with external immobilization alone should be expected [4].
C1-type III odontoid combination fractures (n = 5) were successfully treated with halo immobilization for an average of 12 weeks [4].
For the management of C1-Hangman’s combination fractures, semirigid or rigid external immobilizations have been successful in most patients. In spite of that, the paper by Fielding et al. [30], that included 15 patients with combination C1-Hangman fractures, considered that when the combination Hangman fracture was associated with C2–3 angulation, these injuries were unstable. Surgical stabilization and fusion were recommended as conservative treatment was associated with an 85% nonunion rate [27].
In the paper of Maserati et al. [4], from Dickman et al. series, reporting 7 patients with combination C1–2 body fractures, indicated that all were successfully treated with either halo or SOMI immobilization.
In conclusion, there is no high-class evidence for the treatment of combined atlas-axis fractures. External immobilization can be used for most cases of combined atlas and axis fractures. However, the increased morbidity and mortality of halo-vest immobilization in the elderly, increased rate of pseudoarthrosis in type 2 odontoid fractures, and patient preferences need to be carefully considered. The specific characteristics of the axis fracture combined with the atlas fracture might be a key consideration for surgical fusion (Table 6). Operative management of stabilization and fusion should be considered for cases of combined atlas-type 2 odontoid fractures with an atlantodental interval of ≥ 5 mm and atlas-Hangman’s fracture with C2–3 angulation of ≥ 11° or failure of external immobilization (level III of evidence). For surgical approaches, the posterior C1–2 fusion techniques or anterior odontoid screw fixation are recommended (Table 6). If a fracture of posterior arch of C1 or gross C1–2 instability is present, extension to occipital bone may be required [28].
According to the literature review, the WFNS Spine Committee proposed and voted upon the statements as follows:
Statement 1: There is not high-class evidence of the treatment of combination atlas-axis fractures. This statement reached a strong consensus (yes: 89%; no: 11%).
Statement 2: External immobilization is used in most of the cases of C1–2 combination fractures. This statement reached a full 100% consensus.
Statement 3: We should consider surgical treatment for cases of C1-type II odontoid combination fractures with an anterior atlantodental interval of ≥ 5 mm and C1-Hangman’s fracture with C2–3 angulation ≥ 11°. This statement reached a full 100% consensus.
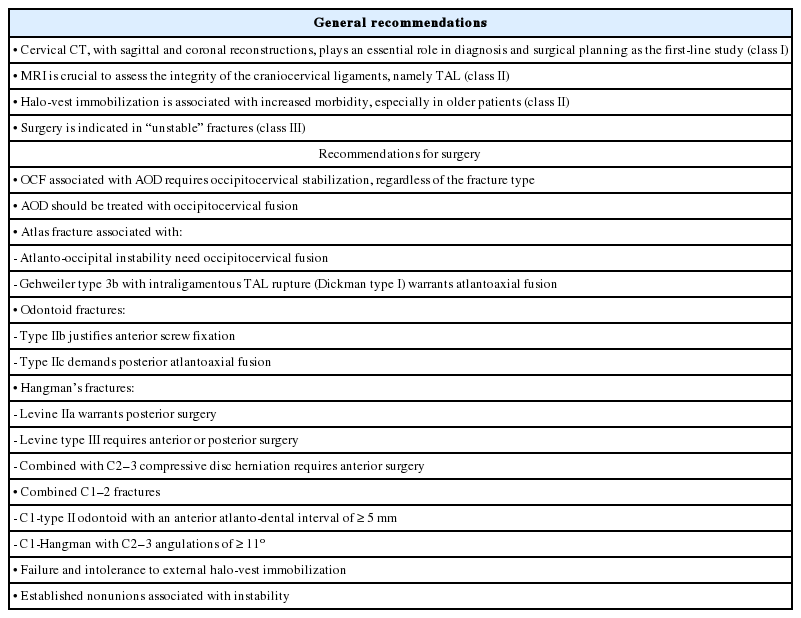
CONCLUSIONS
The above-mentioned statements are the frame of the WFNS Spine Committee recommendations and are based on an extensive review of the best medical evidence published over the last 10 years. They have been voted by a group of experts and ratified in a double session consensus conference. The recommendations are summarized in Table 7. Regarding the classification systems for AOD and combined C1–2 fractures, the emergence of new management-oriented classifications instead of anatomical- or mechanistic-based ones is of uttermost importance. There is also a need for randomized controlled trial studies to clear controversial management (conservative vs. surgery or anterior vs. posterior surgery) of fractures, such as: Gehweiler type 3b (Dickman type II) C1, Levine type II and III C2 Hangman’s, C1-type II odontoid and C1-Hangman’s with abnormal C2–3 angulations.
RECOMMENDATIONS
1. Radiologic Assessment of Upper Cervical Trauma
• In patients with history and physical examination findings suspecting with cervical spinal trauma, cervical CT plays an integral role in diagnosis and surgical planning as the first-line study for screening of the cervical spine.
• AADI > 3 mm or PADI < 13 mm indicate a possible TAL disruption and instability in C1–2.
• Before placement of screws at upper cervical spines in patients with cervical trauma, preoperative 3D CT scanning should be performed to rule out anatomical bony abnormalities.
2. Occipital Condyle Fractures: Classification and Management
• Classification system proposed by Mueller et al. may be preferable in the management of OCF.
• CT imaging should better be used to establish the diagnosis and management of OCF.
• MRI, in addition to CT scan, is recommended to assess the integrity of the craniocervical ligaments for determining the stability of OCF.
• Conservative treatment should be preferred to surgical treatment in OCFs without AOD.
3. AOD Injury
• CT can be enough to define CCI in patients with suspicion of AOD.
• In case of severe TBI, lower cranial nerves deficit and/or spinal cord injury an AOD may be suspected.
• Cervical traction is not recommended for AOD.
• Patients with AOD should be operated for occipitocervical fixation, as the general condition of the patients is stable.
4. Isolated C1 Fractures: Classification and Management
• Treatment of isolated fractures of atlas should be based on CT and MRI criteria, in order to define the fracture type and the integrity of the TAL.
• The majority of atlas fractures is stable and is successfully managed conservatively.
• Surgical indications for atlas fracture are atlanto-occipital instability, an intraligamentous rupture of the TAL, and any “unstable” atlas fracture.
5. Odontoid Fractures: Classification and Management
• In adult patients with odontoid fractures, AADI > 3 mm indicates TAL disruption and instability in C1–2, while AADI ≥ 5 mm implies transverse ligament and accessory stabilizing ligaments ruptured.
• Advanced age, long duration, and preoperative separation of odontoid fracture > 4 mm are predisposing factors for fracture nonunion after posterior C1 lateral mass screw combined with C2 pedicle/laminar screw fixation for type II odontoid fracture.
• For anterior odontoid screw fixation, the interval from injury to operation and fracture “gap” are significantly associated with fusion failure.
6. Hangman Fractures: Classification and Management
• For Hangman’s fracture, upright x-ray performed under medical supervision may be useful besides CT scan.
• For Levine IIA Hangman’s fracture surgery is recommended. This statement reached a full 100% consensus.
• Levine type III Hangman’s fracture may require both anterior and posterior surgery.
• Conservative treatment for Hangman’s fracture should be performed with a rigid collar instead of halo-vest due to its complications.
7. Combined Atlas and Axis Fractures: Classification and Management
• There is not high-class evidence of the treatment of combination atlas-axis fractures.
• External immobilization is used in most of the cases of C1–2 combination fractures.
• We should consider surgical treatment for cases of C1-type II odontoid combination fractures with an AADI of ≥ 5 mm and C1-Hangman’s fracture.
Notes
The authors have nothing to disclose.
Acknowledgements
We would like to thank Ms. Sonia Macedo for kindly editing and reviewing this manuscript for English language.