Cervical Lordosis Ratio as a Novel Predictor for the Loss of Cervical Lordosis After Laminoplasty
Article information
Abstract
Objective
Maintaining cervical lordosis (CL) after laminoplasty is important for indirect decompression of the spinal cord. This study aimed to identify preoperative dynamic radiographic predictors for the loss of CL after laminoplasty.
Methods
We retrospectively analyzed 141 consecutive patients who underwent cervical laminoplasty for cervical myelopathy. The following radiographic parameters were measured before surgery and at 1 year of follow-up: CL, C7 slope, C2–7 sagittal vertical axis (SVA), C2–7 range of motion (ROM), CL in flexion, CL in extension, ROM of flexion (Flex ROM), and ROM of extension. The CL ratio (CLR) was defined as 100 × Flex ROM/C2–7 ROM. ΔCL was defined as postoperative CL minus preoperative CL. Patients were classified into 2 groups: group K (kyphotic change group, ΔCL ≤ -10) and group C (control group, ΔCL > -10).
Results
The patient population comprised 94 men and 47 women (mean age, 70.9 ± 9.4 years), with 24 patients (17.0%) classified into group K. CL, C7 slope, and CLR were significantly higher in group K than in group C. The groups did not significantly differ in age, sex, C2–7 SVA, and C2–7 ROM. On multivariable analysis, the CLR was significantly associated with postoperative kyphotic changes. On receiver-operating characteristic curve analysis (area under the curve = 0.717, p < 0.001), the cutoff value for CLR was 68.9%, with sensitivity and specificity of 87.5% and 57.3%, respectively.
Conclusion
The CLR, reflecting the balance between flexion and extension mobility, was identified as a novel predictor for CL loss after laminoplasty, with a cutoff value of 68.9%.
INTRODUCTION
Cervical laminoplasty is used to treat cervical myelopathy caused by cervical spondylotic myelopathy (CSM) or ossification of the posterior longitudinal ligament (OPLL). Cervical laminoplasty is an effective posterior surgical method for spinal cord decompression, preserving the motion segments and relatively good long-term results reported [1-3]. The decompression effects of this procedure comprise direct posterior decompression and indirect anterior decompression by a posterior shift of the spinal cord [4,5]. The cervical spine alignment should be lordotic to obtain the indirect decompression effect; thus, maintaining postoperative cervical lordosis (CL) is important. Kyphotic cervical alignment may lead to poor postoperative clinical outcomes [6]. However, cervical laminoplasty, as posterior decompression surgery, can cause injury to the posterior neck muscle-ligament complex; therefore, preoperative CL is not maintained postoperatively in some cases [7,8].
Several reports have described preoperative predictors of the loss of CL after laminoplasty [9-17]. Recently, the T1 slope has been reported to be an important factor for predicting postoperative kyphosis as the kyphotic alignment change was greater in patients with a high T1 slope [9,10,12]. Other studies have focused on whole-spine alignment parameters for predicting postoperative kyphotic changes [16]. However, studies evaluating dynamic radiographic parameters are limited.
Therefore, the purpose of this study was to evaluate preoperative dynamic cervical sagittal alignment parameters as potential risk factors for the loss of CL after laminoplasty and determine the cutoff value for the identified risk factor(s). We focused on preoperative radiographic parameters in neutral, extension, and flexion positions.
MATERIALS AND METHODS
1. Patient Enrollment
This study was approved by the Institutional Review Board of Clinical Research Center Kurashiki Central Hospital (No. 3449). We retrospectively reviewed 383 consecutive patients who underwent cervical laminoplasty at our institution between December 2012 and May 2019. Patients diagnosed with CSM or OPLL who underwent cervical laminoplasty from C3 to C6 and completed a 1-year follow-up visit were included. The exclusion criteria were as follows: a history of previous cervical surgery (N = 10), combined with instrumentation (N = 36) and foraminotomy (N = 25), decompression levels including C1 or thoracic spine levels, or use of more selective methods (e.g., C4 to C6) (N = 95), inappropriate radiographic data (N = 33), and follow-up period < 1 year (N = 43). Finally, 141 patients were enrolled in the study. Data regarding demographic variables, including age, sex, body mass index (BMI), and diagnosis (CSM or OPLL), were collected.
2. Surgical Procedures
The muscles attached to the C2 and C7 spinous processes were preserved, while the C3 to C6 laminae were exposed. Double-door laminoplasty [18] was performed from C3 to C6. Hydroxyapatite spacers were placed in the laminar spread from C4 to C6. A spacer could not be placed at C3 because the C2 spinous process was obstructed; however, the C3 lamina was passively maintained spread apart along the C4 lamina. Partial laminectomy was performed at the lower edge of the C2 lamina and the upper edge of the C7 lamina, avoiding damage to the muscle attached to the C2 and C7 spinous processes. Local bone was grafted into the gutter. Postoperatively, patients wore a soft neck collar for several days.
3. Radiographic Parameters
Cervical lateral radiographs were taken in neutral, flexion, and extension positions before surgery and at the 1-year follow-up visit. For radiographs in the neutral position, patients were instructed to stand comfortably and look forward, and CL, C7 slope, and the C2–7 sagittal vertical axis (SVA) were measured (Fig. 1). CL was defined as the angle formed by the inferior end-plates of C2 and C7. The C7 slope was defined as the angle formed by the inferior end-plate of C7 and the horizontal line. C2–7 SVA was defined as the distance between the vertical line from the center of the C2 body and the posterosuperior corner of the C7 body.
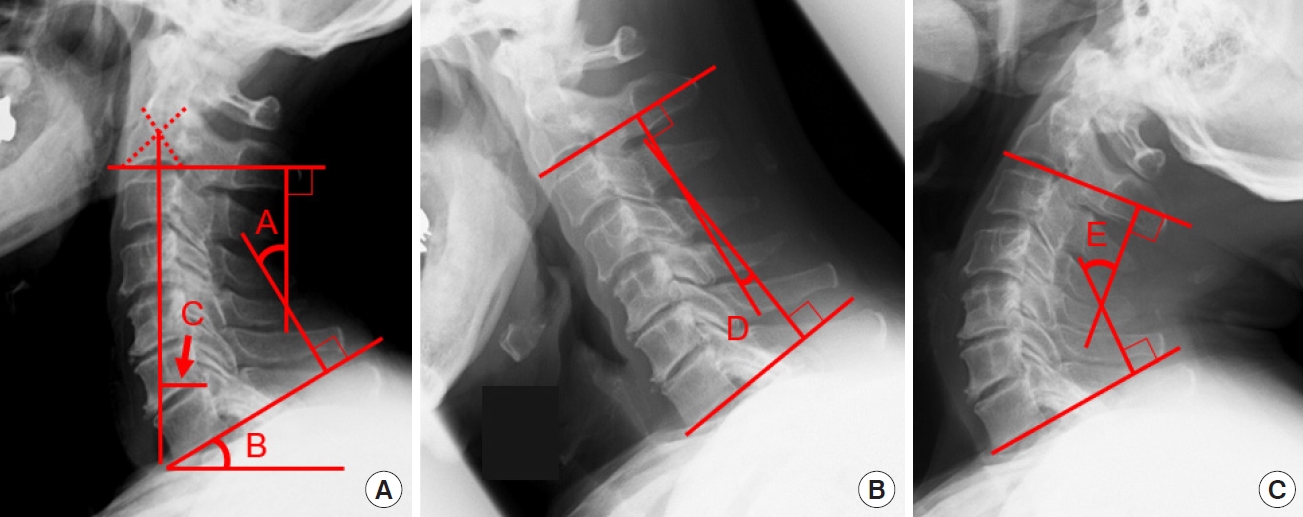
CL (A), C7 slope (B), and C2–7 SVA (C) were measured in the neutral position. Flex CL (D) and Ext CL (E) were measured with the patients in maximal flexion and extension, respectively. CL, cervical lordosis; SVA, sagittal vertical axis; Flex CL, CL in flexion; Ext CL, CL in extension.
For radiographs in the flexion and extension positions, patients either flexed or extended the cervical spine as much as possible, and CL in flexion (Flex CL) and extension (Ext CL) was measured (Fig. 1). The C2–7 range of motion (ROM) was calculated as Ext CL – Flex CL. ROM of flexion (Flex ROM) was calculated as CL – Flex CL, whereas ROM of extension (Ext ROM) was calculated as Ext CL – CL. The CL ratio (CLR) was defined as 100 × Flex ROM/C2–7 ROM (Fig. 2).
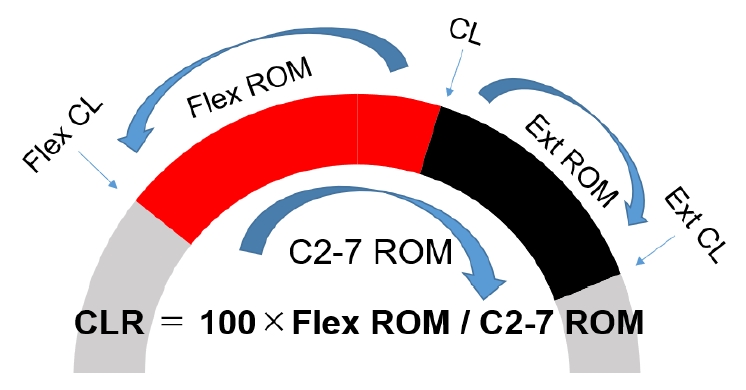
The CLR was defined as 100 × Flex ROM/C2-7 ROM. CL, cervical lordosis; CLR, CL ratio; Flex CL, CL in flexion; Ext CL, CL in extension; ROM, range of motion; Flex ROM, ROM of flexion; Ext ROM, ROM of extension.
ΔCL was defined as postoperative CL – preoperative CL. Patients were classified into the following 2 groups based on the ΔCL: group K (kyphotic change group, ΔCL ≤ -10) and group C (control group, ΔCL > -10).
4. Clinical Parameters
Clinical outcomes were evaluated using the Japanese Orthopedic Association (JOA) score before surgery and at the 1-year follow-up visit. The recovery rate was calculated based on the Hirabayashi method as follows: JOA recovery rate= 100× (postoperative JOA – preoperative JOA)/(17 – preoperative JOA) [19].
5. Statistical Analysis
Data are presented as the mean ± standard deviation unless otherwise specified. Spearman rank-order correlation analysis was used to evaluate the relationships between the CLR, ΔCL, and other preoperative parameters. Differences between groups K and C were evaluated using the chi-square test and Mann-Whitney U-test for categorical and continuous variables, respectively. To identify the risk factors for postoperative kyphotic change, a multivariable logistic regression analysis was performed. Receiver-operating characteristic (ROC) curve analysis was used to determine the optimal cutoff value, defined as the point corresponding to the maximum sum of the sensitivity and specificity. Values of p < 0.05 were considered statistically significant, and JMP Pro 14 (SAS Institute Inc., Cary, NC, USA) was used for all analyses.
RESULTS
1. Demographic, Radiographic, and Clinical Data
In total, 141 patients (mean age, 70.9 ± 9.4 years; 94 males, 47 females) were enrolled in this study. The overall demographic, radiographic, and clinical data are summarized in Table 1.
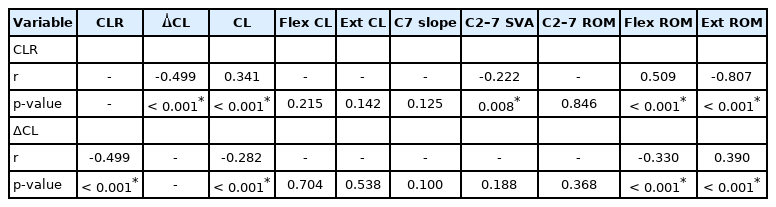
2. Correlations Between the CLR, ΔCL, and Other Preoperative Radiographic Parameters
The correlations between the CLR, ΔCL, and other preoperative radiographic parameters are shown in Table 2. ΔCL was correlated with the CLR (r = -0.499, p < 0.001), CL (r = -0.282, p < 0.001), Flex ROM (r = -0.330, p < 0.001), and Ext ROM (r = 0.390, p < 0.001). In patients with a higher preoperative CL or CLR, greater kyphotic alignment change was observed postoperatively. Similarly, the CLR was correlated with CL (r = 0.341, p < 0.001), C2-7 SVA (r = -0.222, p = 0.008), Flex ROM (r = 0.509, p < 0.001), and Ext ROM (r = -0.807, p < 0.001). Patients with a higher preoperative CLR had higher CL and lower C2–7 SVA. No significant correlations were observed between the other evaluated parameters.
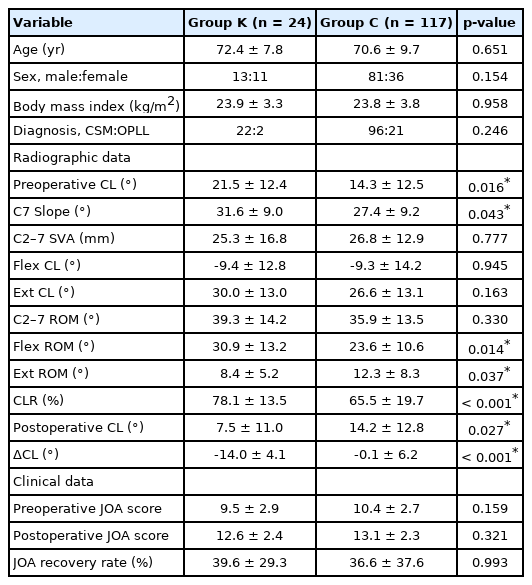
3. Comparison of Each Variable According to the Postoperative Loss of CL
Postoperative loss of CL (ΔCL ≤ -10) occurred in 24 patients (17.0%; i.e., group K). The differences between groups K and C are summarized in Table 3. The groups did not significantly differ in age, sex, BMI, and diagnosis. The preoperative CL was higher (21.5 ± 12.4 vs. 14.3 ± 12.5, p = 0.016) and the postoperative CL was lower (7.5 ± 11.0 vs. 14.2 ± 12.8, p = 0.027) in group K than in group C. Accordingly, ΔCL was lower in group C than in group K (-14.0 ± 4.1 vs. -0.1 ± 6.2, p < 0.001).
The C7 slope, CLR, Flex ROM, and Ext ROM significantly differed between groups K and C. The C7 slope (31.6 ± 9.0 vs. 27.4 ± 9.2, p = 0.043), CLR (78.1 ± 13.5 vs. 65.5 ± 19.7, p < 0.001), and Flex ROM (30.9 ± 13.2 vs. 23.6 ± 10.6, p = 0.014) were higher and Ext ROM (8.4 ± 5.2 vs. 12.3 ± 8.3, p = 0.037) was lower in group K than in group C. No significant differences were observed in the other radiographic parameters. Preoperative JOA, postoperative JOA, and JOA recovery rates did not significantly differ between groups K and C.
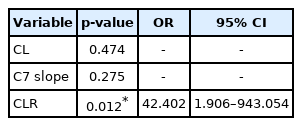
4. Risk Factors for Postoperative Kyphotic Change
Multivariable logistic regression analysis was performed to estimate the odds ratio for the postoperative loss of CL (ΔCL ≤ -10) according to 3 preoperative radiographic parameters: CL, C7 slope, and CLR (Table 4). Among the dynamic radiographic factors (CLR, Flex CL, Ext CL, C2–7 ROM, Flex ROM, and Ext ROM), the CLR with the most significant correlation with ΔCL and the smallest p-value on comparison of group K with group C were applied in the multivariable analysis. The CLR was observed to be an independent risk factor for the postoperative loss of CL (p = 0.012; odds ratio, 42.402; 95% confidence interval, 1.906–943.054). The scatterplot in Fig. 3 shows the relationship between ΔCL and CLR. Patients with a higher CLR tended to lose their preoperative CL after surgery considerably. In the ROC curve analysis for the prediction of ΔCL ≤ -10 (area under the curve [AUC]=0.717, p < 0.001), the cutoff value for CLR was 68.9%, with a sensitivity of 87.5% and a specificity of 57.3% (Fig. 4).
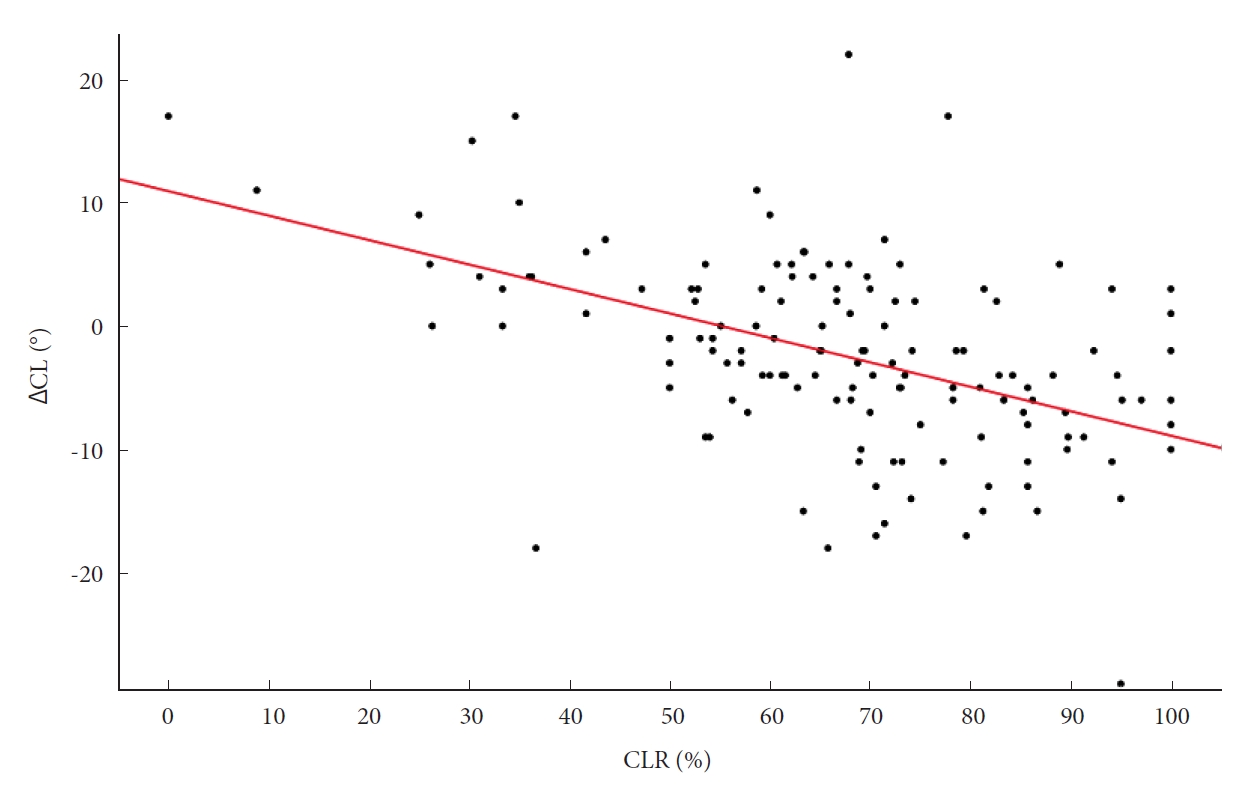
Scatterplot showing the relationship between ΔCL and CLR. Patients with a higher CLR tended to considerably lose their preoperative CL after surgery (r = -0.499, p < 0.001). CL, cervical lordosis; ΔCL, postoperative CL – preoperative CL; CLR, CL ratio.
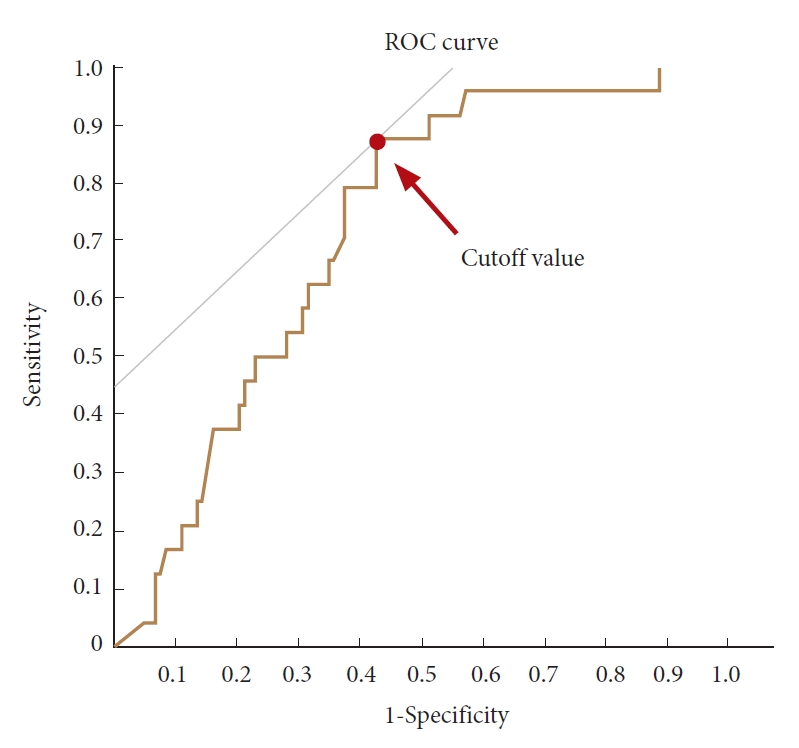
ROC curve analysis for the prediction of ΔCL ≤-10 (area under the curve = 0.717, p < 0.001). The cutoff value for the CLR was 68.9%, with a sensitivity of 87.5% and a specificity of 57.3%. CL, cervical lordosis; ΔCL, postoperative CL – preoperative CL; CLR, CL ratio; ROC, receiver-operating characteristic.
CLR (AUC=0.717) was more useful as a predictor than CL (AUC=0.657), C7 slope (AUC=0.631), Flex ROM (AUC=0.659), and Ext ROM (AUC=0.635). CLR was nonnormally distributed, and it did not show significant correlations with age (p = 0.572), sex (p = 0.962), BMI (p = 0.374), and diagnosis (p = 0.744).
DISCUSSION
Cervical laminoplasty is an effective surgical procedure for cervical myelopathy. In this surgical method, posterior compression factors are directly removed and the posterior spinal cord shifts, thus providing indirect decompression effects [4,5]. To obtain this indirect decompression effect, cervical lordotic alignment is important. Therefore, cervical alignment, before and after laminoplasty, is considered to affect clinical outcomes. However, the alignment and ROM of the cervical spine have been reported to change with laminoplasty. For example, Machino et al. [20] reported that the C2–7 Cobb angle became 1.8° more lordotic in the neutral position, 5.9° more lordotic in the flexion position, and 0.6° more kyphotic in the extension position, and the ROM was reduced to 87.9% after surgery. In some cases, the cervical alignment became kyphotic after laminoplasty despite preoperatively maintaining CL. Thus, the preoperative prediction of the loss of CL after surgery would be useful for obtaining good clinical outcomes by laminoplasty.
Various risk factors have been reported for kyphotic alignment change after laminoplasty [9-17]. For example, Machino et al. [15] reported that the cutoff value of the preoperative C2–7 lordosis angle for the prediction of postlaminoplasty kyphosis was 7° in patients with CSM without a preoperative kyphotic angle. Additionally, Sakai et al. [13] reported that a greater center of gravity of the head – C7 SVA (cutoff value, 42 mm) and advanced age (cutoff value, 75 years) were risk factors for kyphotic deformities after laminoplasty in patients without preoperative cervical kyphotic alignment. In contrast, Matsuoka et al. [16] focused on the global spinal alignment and reported that in patients without preoperative cervical and global spinal sagittal imbalance, a small C7 SVA accompanied by lumbar hyperlordosis was the characteristic alignment leading to postoperative cervical kyphosis after laminoplasty. Recently, the T1 slope has been discussed as a predictor of postoperative kyphotic alignment change [9-12]. Kim et al. [9] reported that patients with a high T1 slope had greater kyphotic alignment change after cervical laminoplasty at the 2-year follow-up; the authors hypothesized that kyphotic alignment change by posterior structural injury after laminoplasty was more marked in patients with a high T1 slope. In another study, Kim et al. [10] reported that patients with OPLL and a higher T1 slope had more lordotic curvature before surgery and demonstrated a greater loss of CL at the 2-year follow-up. However, Cho et al. [11] reported that the degree of aggravation did not correlate with the preoperative T1 slope and that most clinical parameters improved regardless of the preoperative T1 slope.
We evaluated both static alignment and dynamic image parameters to identify useful predictors for postoperative kyphotic alignment change. Lee et al. [17] reported extension function (EF, Ext ROM) as a new predictor of the loss of CL; no significant kyphotic changes occurred after laminoplasty when the EF was greater than or equal to 14°. The authors hypothesized that the function of the posterior neck muscle-ligament complex was represented by the EF [17]. Suk et al. [14] reported that one of the preoperative factors affecting postoperative kyphosis is a kyphotic angle during flexion that is larger than the lordotic angle during extension. We proposed a new factor, the CLR, as an index reflecting the location of the neutral cervical position within the range of the extension and flexion motion. This implies that patients with a higher CLR have a large flexion ROM and small extension ROM because the neutral position is closer to the maximum extension. The degree of extension mobility indicates the function of the posterior neck muscle-ligament complex and is considered an inhibiting factor of kyphotic alignment change [17]. Additionally, poor flexion mobility is also considered to indicate that cervical kyphosis is inhibited by structural factors, such as bone, ligament, or muscle. Therefore, both Flex ROM and Ext ROM are important factors. This new factor, the CLR, is a useful and simple index for expressing the balance between flexion and extension mobility.
For cases wherein cervical kyphotic change after laminoplasty is predicted, the indications for laminectomy and fusion or anterior cervical diskectomy and fusion (ACDF) should be considered. However, in this study, no significant differences were observed in clinical outcomes between the kyphotic change and control groups. One reason for this may be that the postoperative CL angle in the kyphotic change group was +7.5° on average, and lordotic alignment was maintained in most cases. Alignment changes were considered insufficient to worsen the clinical outcomes, even in the kyphotic change group. As reflected in the cervical laminoplasty procedures of our institution, we consider that preservation of the posterior neck muscle-ligament complex is important; therefore, the paravertebral muscles attached to the C2 and C7 spinous processes are preserved, even with multilevel stenosis, including C2/3 or C6/7. Supposedly, this minimally invasive surgical procedure contributed to the noninferior clinical outcomes in the kyphotic change group. Takeshita et al. [21] reported that subaxial laminoplasty maintained the cervical alignment; however, if laminoplasty included C2, the alignment worsened. Iizuka et al. [22] reported that preservation of the muscles attached to the C2 spinous process prevented significant changes in cervical alignment after laminoplasty.
This study has several limitations. First, because our study was retrospective, a selection bias may exist. Second, a total of 43 cases were lost to follow-up at 1 year. Third, as the follow-up period was 1 year, the long-term prognosis is unknown. Fourth, we could not evaluate the global spinal alignment. Fifth, clinical outcomes were only evaluated by the JOA score. Possibly, the clinical outcomes could be evaluated in a more detailed manner by incorporating other evaluation systems, such as a visual analog scale or the Neck Disability Index. Finally, since this study did not compare surgical techniques (laminoplasty, laminectomy and fusion, ACDF), the optimal surgical procedure could not be indicated based on postoperative kyphotic changes. Hence, this is a theme that should be clarified by future research.
CONCLUSION
We identified a new factor, the CLR, for predicting the loss of CL after laminoplasty. The CLR is a useful and simple index for expressing the balance between flexion and extension mobility. The cutoff value for the CLR was 68.9%.
Notes
The authors have nothing to disclose.