Telemedicine in Neurosurgery: Standardizing the Spinal Physical Examination Using A Modified Delphi Method
Article information
Abstract
Objective
The use of telemedicine has dramatically increased due to the coronavirus disease 2019 pandemic. Many neurosurgeons are now using telemedicine technologies for preoperative evaluations and routine outpatient visits. Our goal was to standardize the telemedicine motor neurologic examination, summarize the evidence surrounding clinical use of telehealth technologies, and discuss financial and legal considerations.
Methods
We identified a 12-member panel composed of spine surgeons, fellows, and senior residents at a single institution. We created an initial telehealth strength examination protocol based on published data and developed 10 agree/disagree statements summarizing the protocol. A blinded Delphi method was utilized to build consensus for each statement, defined as > 80% agreement and no significant disagreement using a 2-way binomial test (significance threshold of p < 0.05). Any statement that did not meet consensus was edited and iteratively resubmitted to the panel until consensus was achieved. In the final round, the panel was unblinded and the protocol was finalized.
Results
After the first round, 4/10 statements failed to meet consensus (< 80% agreement, and p = 0.031, p = 0.031, p = 0.003, and p = 0.031 statistical disagreement, respectively). The disagreement pertained to grading of strength of the upper (3/10 statements) and lower extremities (1/10 statement). The amended statements clarified strength grading, achieved consensus (> 80% agreement, p > 0.05 disagreement), and were used to create the final telehealth strength examination protocol.
Conclusion
The resulting protocol was used in our clinic to standardize the telehealth strength examination. This protocol, as well as our summary of telehealth clinical practice, should aid neurosurgical clinics in integrating telemedicine modalities into their practice.
INTRODUCTION
Telemedicine, also known as telehealth, involves the communication of medical information through electronic systems for the delivery of health care, education, and health administration [1]. Potential benefits of telemedicine technologies include providing access to care for patients without a local provider, reducing patient wait and travel times, and decreasing health care costs. Telemedicine has been steadily increasing in use, especially as associated technologies continue to improve [1,2]. In 2016, the Department of Health and Human Services (HHS) estimated that 60% of health care institutions in the United States used some sort of telemedicine modality, although use remained relatively limited due to lack of patient interest as well as concerns surrounding billing, regulatory and medicolegal matters [1,3]. The coronavirus disease 2019 (COVID-19) pandemic and associated social distancing measures have brought renewed attention to the use of telemedicine in the United States. The HHS has subsequently relaxed regulatory requirements for telemedicine to encourage its use during the pandemic and reduce patient exposure to health care facilities [4]; telemedicine is now an integral part of many health care systems across the country. The use of telemedicine for clinical care will likely remain prevalent throughout the United States given the long-term need for social restrictions [5].
As a result, neurosurgeons are now faced with the reality of using telemedicine modalities to provide outpatient care, such as in a neurosurgical spine clinic, to minimize the risk of virus transmission. Although new federal policies have increased the accessibility of telemedicine technologies, a number of challenges remain. Primary amongst these is the lack of standardized tele-neurologic examination maneuvers, which is crucial in assessing and following neurosurgical patients. While previous studies have highlighted the reliability of the neurologic exam performed over telehealth technologies, they frequently require the use of an assistant [6-9]. Thus, as patients increasingly attend telehealth visits from their home in order to avoid health care facilities, there is a significant need for a standardized in-home neurologic exam. An additional challenge to the implementation of telehealth technologies in neurosurgical clinics is the lack of familiarity with the clinical evidence surrounding their use as well as unique financial and liability considerations.
To help address these concerns, we (1) describe a standard tele-neurologic examination, based on available evidence in the literature and (2) create a consensus-based tele-strength examination protocol, as this is one of the most challenging parts of a tele-neurologic examination. We then highlight the utility of our protocol through a clinical case of a lumbar disc herniation leading to foot drop that was observed during a telehealth visit using our examination maneuvers. Finally, we discuss the clinical evidence surrounding outpatient neurosurgical telehealth visits, financial and legal considerations, and COVID-19 specific changes.
MATERIALS AND METHODS
1. Literature Review, Quantifying Telehealth Visits
We first performed a literature search to find all spine surgery and neurosurgery articles pertaining to the telehealth neurological examination, as well as billing and coding practices for telemedicine. We found that there were not enough articles to formulate a formal meta-analysis, and therefore used our literature search to create protocol for the Delphi method. Regarding billing, it was not possible to obtain a meta-analysis for 2 reasons: (1) there was an overall lack of published data addressing the billing of the telemedicine in neurosurgery and (2) the COVID-19 pandemic resulted in Centers for Medicare and Medicaid Services (CMS) waiver 1135 (starting March 6, 2020; corona virus waiver) that temporarily reduced restrictions surrounding telehealth care. Thus, the current uncertainty of the permanence of this waiver, combined with the paucity of literature pertaining to neurosurgery clinic visits, precluded a systematic review of telehealth billing. Instead, we summarize current billing practices in the discussion. To better understand the role of telehealth in our patient population, we quantified the number of patients seen in-clinic since the start of the pandemic on a day-by-day basis.
2. Delphi Method
The Delphi Method was used to create a consensus-based tele-strength examination [10,11]. Twelve neurological surgeons (7 spine surgeons, 2 fellows, and 3 senior residents) at our institution were given a 10-item online survey (SurveyMonkey) relating to specific aspects of the tele-strength examination. Surgeons could either “agree” or “disagree” with a given statement. Responses to the initial survey were collected and analyzed. Participants were blinded to each other’s responses and to the identity of the other members of the panel. Consensus was defined ahead of time using 2 criteria: (1) > 80% agreement of the panel for a particular question and (2) an exact binomial statistical test against the expected hypothesis of 95% agreement using a 2-tailed p-value threshold of p < 0.05. All statements failing to meet consensus were analyzed, and direct feedback from disagreeing surgeons was sought. Questions failing to meet consensus were then modified and resubmitted to the expert panel in a second round of the Delphi method. After consensus for all statements was achieved, the final protocol was drafted and sent to the members of the panel. Panel members were unblinded for this portion of the Delphi method. The protocol was then finalized with direct panel member communication to each other.
3. Statistical Methods
All statistical methods were carried out in Matlab (version release 2017b, Mathworks, Inc., Natick, MA, USA) using custom software to implement the 2-sided exact binomial test, as well as the plotting function.
RESULTS
1. Rate of Telehealth Visits During the COVID-19 Pandemic
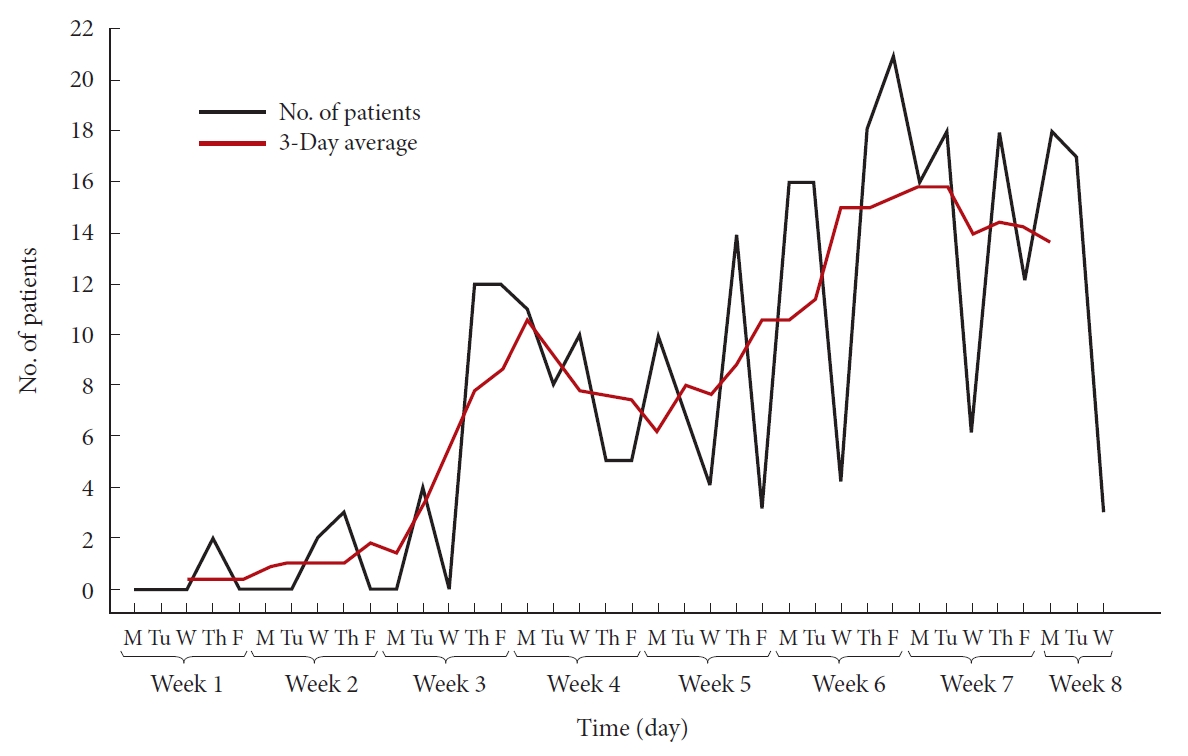
Fig. 1 demonstrates the number of patients that were seen using telehealth over an 8-week period at our spine clinic, including before the county’s COVID-19 shelter-in-place order (week 1), immediately following the shelter-in-place order (weeks 2–3), and after the shelter-in-place order until the time of writing (weeks 4–8). In order to protect patient identity, exact dates are not shown. As seen, telehealth visits increased in our spine clinic by 10 times following the shelter-in-place order (~0–1 patient per day before the pandemic compared to 10–16 patients per day after the pandemic, Fig. 1).
2. Delphi Method
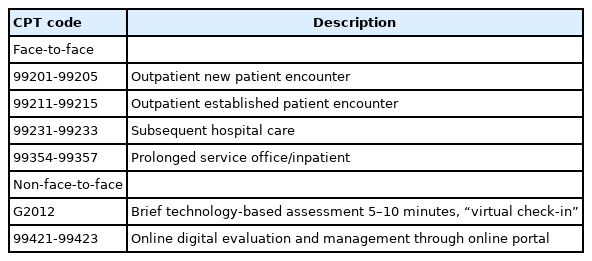
Fig. 2 highlights the results of the first round of the Delphi method. In the first round, 5 statements pertained to the upper extremity, 5 to the lower extremity, and 1 to the use of a weight in the exam. More specifically, statement 1 established that the physical exam should be performed with a known item with a standardized weight. Statements 2–6 described strength testing of the upper extremities, specifically the deltoids, biceps, triceps, wrist extension, grip, and hand intrinsic muscles, respectively. Statements 6–11 then pertained to strength testing of the lower extremities, specifically the iliopsoas, quadriceps, hamstrings, foot dorsiflexion, and foot plantar flexion, respectively. Following completion of the first round, statements 2, 4, 6, and 8 failed to reach consensus (p = 0.031, p = 0.031, p = 0.003, and p = 0.03, respectively).
Percentage of agreement on Delphi consensus statements regarding spine physical exam maneuvers in round 1 (A) and round 2 (B). The consensus threshold was 80% (red dashed line); 95% consensus, used as an expected outcome in 2 tailed binomial testing of significant disagreement, is indicated by the green dashed line. The green asterisk indicates statements that had significant disagreement.
We subsequently progressed to the second round of the Delphi method. First, we modified the statements that did not achieve consensus and resubmitted those statements to the panel. We found that the majority of the disagreement in the first round involved how to grade strength using the known object; specifically, that a 5/5 full strength exam is not possible to test over telemedicine. With that feedback, we created new statement that defined strength grading on a 4-point scale (0, no movement; 1, movement not against gravity; 3, movement against gravity; and 4, movement against resistance, and modified the strength testing of muscle groups accordingly (Fig. 2B). After this modification, all statements achieved consensus.
Finally, we used the consensus statements from the Delphi rounds to create the finalized protocol (Fig. 3). This protocol fits on one printed page and can be used by the surgeon or advanced practitioner when completing the muscle strength physical examination over telemedicine.
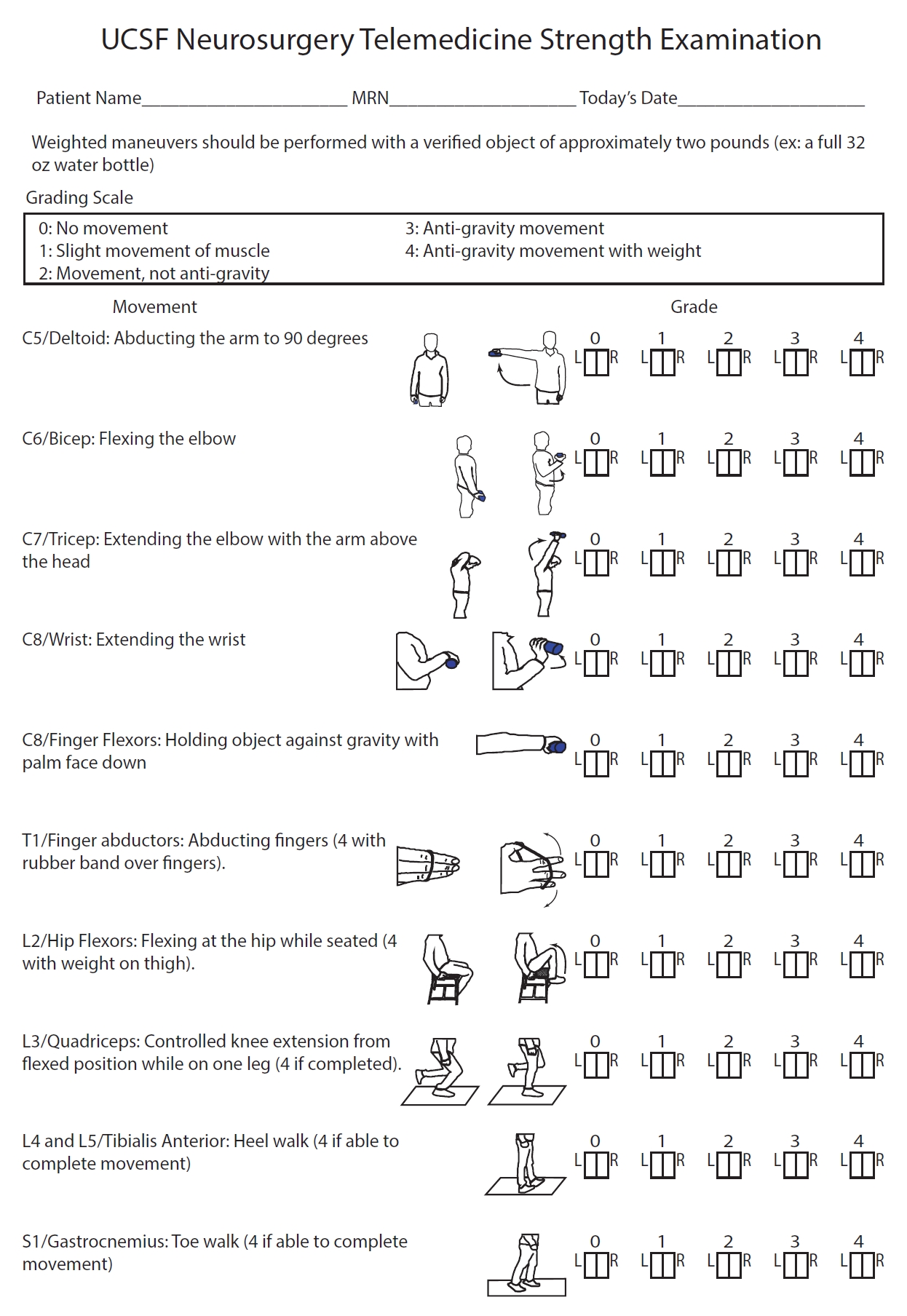
A consensus-based tele-strength examination as a result of our modified Delphi method. UCSF, University of California, San Francisco.
In addition to the spine-specific motor physical examination, we also list in Table 1 a standard neurological examination. The examination techniques were extracted from both neurosurgery and neurology publications [6-9,12]. We utilized these results and clinical experience to produce a template for a general telemedicine neurologic exam in neurosurgical patients (Table 1). The general neurological examination should be used to supplement the motor examination (Fig. 3) as needed. Fig. 4 depicts a simulated patient example of the spine telemedicine motor examination being performed over an audio/visual communication system.
DISCUSSION
1. Overview of Telemedicine in Surgical and Neurosurgical Clinical Practice
Routine outpatient visits, including preoperative assessment and monitoring of chronic conditions, are key areas in which telemedicine has been shown to be safe, time-saving, and cost effective. One of the leaders of telemedicine in the United States, the Department of Veterans Affairs (VA) has highlighted the applicability of telemedicine technologies for routine outpatient visits beginning in the 1990s, with continued growth since that time [13]. However, there is limited published data from the VA on their telemedicine experience with regard to surgical subspecialties. A 2018 pilot study investigating the use of telemedicine by the Connecticut VA plastic surgery department demonstrated high patient satisfaction among 41 patients who were seen using telemedicine technology [14]. Beyond the VA, preoperative assessment of patients via telemedicine has been shown to be accurate with regards to diagnosis and treatment planning in both pediatric surgery [15] and oral and maxillofacial surgery [16] with no significant difference in outcomes and reduced cost. Studies within neurology have also demonstrated the feasibility of telemedicine in the evaluation and monitoring of neurologic diseases such as epilepsy [17], movement disorders [18,19], and dementia [20,21].
While literature regarding nonneurosurgical subspecialties and neurology is more plentiful, the application of telemedicine has also been sparsely described in the neurosurgical literature. James [22] describes their experience with the formation of a pediatric neurosurgical telemedicine clinic for routine outpatient visits from 2011–2016. Subsequent analysis of the clinic’s socioeconomic impact revealed significant time and cost savings in excess of $233 per family [23]. Similarly, Mendez et al. [24] highlighted the feasibility of using a remote-presence robot for the programming of neuromodulation devices, with comparable outcomes relative to in-person visits. While the described studies are promising, additional investigations evaluating cost and clinical outcomes associated with telemedicine for outpatient care across neurosurgical subspecialties are needed.
Telemedicine technologies have also been described in the routine postoperative care of patients across surgical subspecialties for over a decade [25]. Studies from urology [26] to orthopedic surgery [27]. have demonstrated equivalent or improved efficacy and safety of telemedicine visits when compared to those in the clinic. A systematic review of telemedicine in postsurgical care found a slight increase in complications with telemedicine use (2.8% [7 of 254] vs. 0.4% [1 of 242]); however, there was also no significant difference in postoperative complications in any individual study [25]. Studies performed specifically within neurosurgery have also demonstrated the safety and cost-effectiveness of telemedicine in postoperative care [28-31]. International studies have also demonstrated reduced travel time, cost-effectiveness, and cost-saving associated with the use of Skype teleconferences (Skype Technologies S.A.R.L, Luxembourg City, Luxembourg) in the postoperative management of patients [28,31]. It is also possible that simple postoperative procedures, such as suture removal [32], may be directed using telemedicine, although further investigation is needed.
2. Financial and Legal Considerations
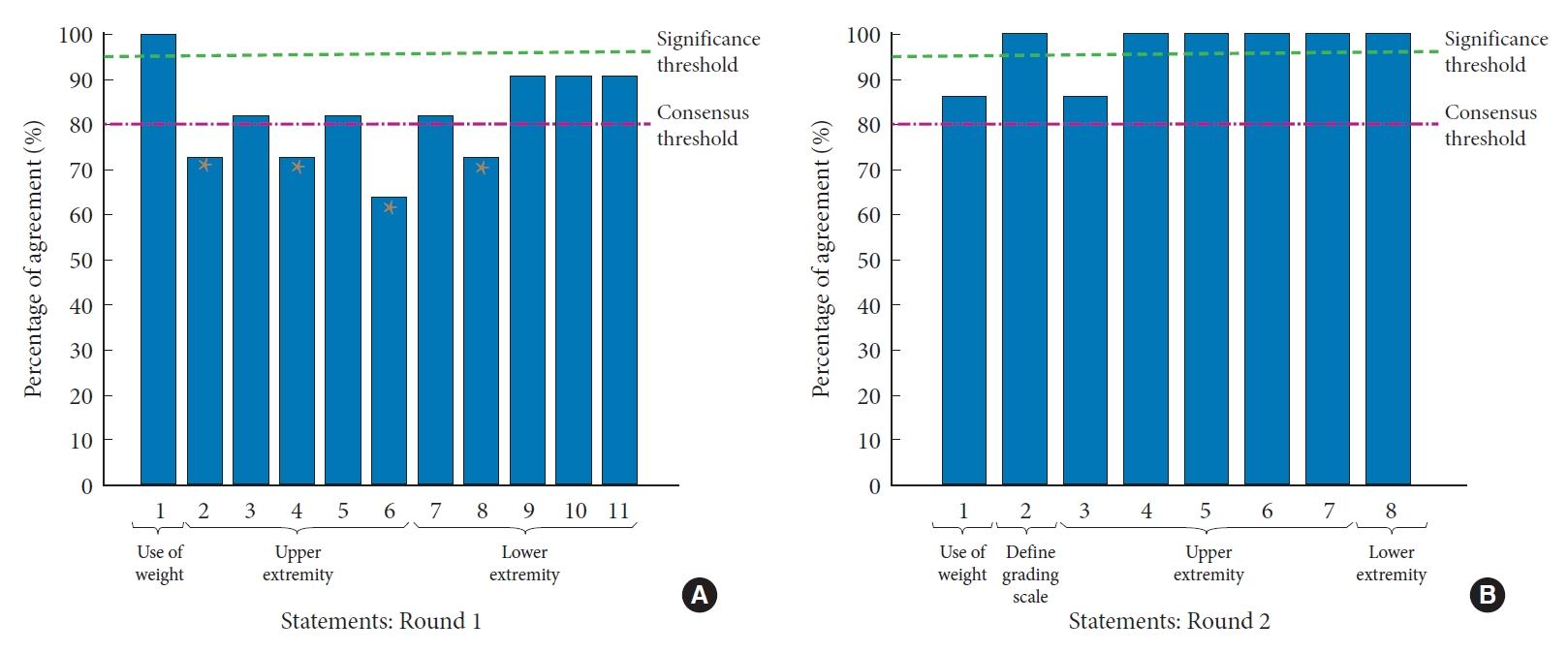
Prior to the COVID-19 pandemic, the use of telehealth in the United States was limited by concerns regarding reimbursement as well as federal and state regulations surrounding patient privacy, physician licensure, and liability [1,3]. There was confusion regarding what constituted a “tele-visit” as well, with different definitions, coding requirements and reimbursement rates for provider-patient electronic communication. As an example, Table 2 shows traditional current procedural terminology codes associated with telephonic, patient-initiated interactions. As providers seek to adapt to the pandemic, the HHS has expanded telemedicine coverage and relaxed regulations surrounding telemedicine in an effort to increase patient access to care without the need to travel to a health care facility [4,33,34]. While the regulatory situation remains fluid, there have been key changes that affect the clinical practice of neurosurgery.
A turning point in the use of telemedicine modalities for clinical care was the President’s initial declaration of a public health emergency on January 31st, 2020. Subsequently, the federal government, including the HHS and CMS began implementing policies to increase access to telehealth visits for patients. Early changes targeted the coverage of telemedicine, including telehealth visits (defined as using synchronous audio and video technologies to replace visits that usually occur in-person), Virtual Check-Ins (brief communication, including over a telephone, usually patient-initiated but can also be initiated by the provider), and E-Visits (non-face-to-face patient-initiated communications via online patient portal) (Table 3 [33]). Historically, Medicare telehealth visits and virtual check-ins were limited to established patients in rural settings, with restrictions on the frequency of visits [35,36].
Initially, coverage was not extended to telehealth visits with patients in their own homes [35]. On March 6, 2020, however, CMS expanded coverage for telehealth via an 1,135 waiver. The waiver removed geographic and visit frequency restrictions on reimbursement. In addition, coverage was expanded to a variety of office and hospital visits performed via telehealth technologies, including visits with patients at their homes, with equal reimbursement as a regular in-person visit. Also included in this waiver are initial patient evaluations in the hospital and emergency department as well as observation status, which previously were not eligible for telehealth coding and payment. This applies to both new and established patients for the duration of the COVID-19 public health emergency [33]. Although many private insurance payers have follow suit with similar policies, there remains variability in reimbursement guidelines between private insurance plans as well as from state to state Medicaid programs. Nevertheless, the actions taken by CMS with regards to telehealth visit reimbursements have increased the financial viability of using these technologies for patient care. It is unknown how long these waivers will last once the COVID pandemic has resolved but there has been a dramatic surge in their popularity during this crisis [33].
In an effort to increase telehealth accessibility, the Office for Civil Rights at HHS has determined that essentially any patient-facing audio/visual communication method (e.g., Zoom, Skype, Apple FaceTime) can be used for telehealth visits. While these modalities are not considered Health Insurance Portability and Accountability Act compliant by HHS, the agency has temporarily suspended enforcement of noncompliance with these rules. However, this exemption does not include the use of public facing modalities (e.g., TikTok, Facebook Live) [37]. Similarly, Medicare and Medicaid licensure requirements have been relaxed. Thus, physicians can practice, including telehealth visits, outside of the state they are licensed in, although state-specific regulations should be considered as well [38]. The Drug Enforcement Administration has also reduced restrictions, allowing providers to prescribe medications following a telehealth visit [39]. While these policies increase patient and physician access to telehealth visits, their long-term fate and the liability to the physician remain to be determined.
As the use of telemedicine visits grows, so to have concerns regarding associated physician malpractice and liability [40]. Fogel and Kvedar [41] performed a search of legal databases for medical malpractice suits associated with direct-to-consumer telemedicine and found no cases. This is likely due to the relatively low numbers of telemedicine visits [41,42]. Additionally, telehealth visits frequently involve outpatient visits that have relatively low malpractice risk [41,43]. Nevertheless, telehealth-specific malpractice considerations include the need for informed consent of the patient as well as ensuring the security and privacy of communication devices [43,44]. Measures to increase the security of a telemedicine visit vary depending on the service being used, but include the use of a password to access the visit, disallowing participants to join before the host, utilization of a virtual waiting room and preventing additional users from joining the visit once it has started. In addition, physicians should consider that essentially any telecommunication with a patient, regardless of how short, is considered professional advice [45] and establishes the patient-physician relationship, a requisite for professional liability. Thus, while telemedicine does not currently seem to be associated with increased rates of malpractice suits, neurosurgeons should take adequate precautions as we continue to learn more about telehealth practice.
3. Limitations
The most significant limitations of the protocol in Fig. 3 are (1) development at a single-center and (2) lack of prospective validation of this technique. However, given the highly extenuating circumstances involving the COVID-19 pandemic, the use of telemedicine is rapidly rising. It is thus useful to compare institutional protocols during this time, leaving the prospective validation of such protocols to future studies. Similarly, the general tele-neurologic exam in Table 1 requires additional validation, especially as cranial nerve abnormalities can be subtle and difficult to detect over visual/audio communication systems. Rather, Table 1 should serve as a guide to the literature surrounding general tele-neurologic exam maneuvers to supplement our consensus bases tele-strength protocol (Fig. 3) as needed. Despite these limitations, we believe the standardized physical examination maneuvers in our tele-neurologic examination and tele-strength protocols can act as a template for neurosurgical providers in their telehealth clinics, improving the efficacy and reliability of their tele-physical exams. To our knowledge, this is the first study to provide a consensus-based tele-strength examination.
However, there remains paucity of neurosurgical specific data surrounding the clinical applicability of these technologies as well as the performance and reliability of the tele-neurologic exam; additional research is required to determine best practices, including the sensitivity and specificity of telehealth-specific examination maneuvers. As a result, telemedicine examinations should still be interpreted with caution as their ability to replicate in-person findings has not been fully elucidated. Telemedicine is a newer modality of patient care, especially for spine surgeons, and does not completely replace in-clinic visits at this time. Rather, it should be used in the appropriate clinical scenarios, such as low-risk outpatient visits, and to protect patients from the risk associated with in-person visits to health care facilities. Future studies providing guidelines surrounding which types of patient visits are most amenable to telemedicine are warranted. Patient feedback on telemedicine visits should also be gathered and incorporated into clinical practice. Despite these limitations, telemedicine for neurosurgery will likely continue to play a role in the care of patients even after the COVID-19 pandemic has resolved, particularly as technologies continue to improve. Exciting future applications include telepathology [46], tele-surgical collaboration [47], and even the remote performance of surgical procedures [48].
CONCLUSION
We present a standardized tele-neurological examination and consensus-based tele-strength examination that was created using a formalized Delphi method to build consensus among a panel of spine neurological surgeons. We also provide a brief overview of the clinical evidence surrounding telehealth visits in neurosurgery as well as financial and legal considerations to aid neurosurgeons venturing into telehealth practice.
Notes
The authors have nothing to disclose.