Utilization of S1 Foraminal Hooks for Augmentation of S1 Screws in Adult Spinal Deformity Surgery: Comparative Study With Iliac Screws
Article information
Abstract
Objective
To compare the outcomes of S1 foraminal hooks and iliac screws regarding fusion rate at the lumbosacral junction and protective effects on S1 screws.
Methods
From January 2017 to December 2019, consecutive patients who underwent long fusions (uppermost instrumented vertebra at or above L1) to the sacrum for adult spinal deformity were enrolled. Patients were divided into S1 foraminal hook group and iliac screw group. Radiographic parameters and the incidence of pseudarthrosis and instrument failure at the lumbosacral junction were compared between the groups.
Results
Twenty-nine patients (male:female = 1:28) with a mean age of 73.6±6.8 years were evaluated. Sixteen patients (55.2%) had S1 foraminal hook fixation and 13 patients (44.8%) had iliac screw fixation. Lumbar lordosis, sacral slope, and sagittal vertical axis did not differ between the groups preoperatively and postoperatively. The rate of L5/S1 pseudarthrosis was significantly higher in S1 foraminal hook group (5 of 16, 31.3%), compared to iliac screw group (0 of 13, 0%; p=0.048). Instrument failure at the lumbosacral junction trended toward a higher rate in S1 foraminal hook group (6 of 16, 37.5%) than in iliac screw group (1 of 13, 7.7%), without statistical significance (p=0.09). Proximal junctional kyphosis/failure occurred less often in S1 foraminal hook group (2 of 16, 12.5%) than in iliac screw group (3 of 13, 30.8%) without statistical significance (p=0.36).
Conclusion
Treatment with S1 foraminal hooks achieved equivalent satisfactory sagittal correction with proportioned alignment compared to that with iliac screws. However, S1 foraminal hooks did not provide enough structural support to the lumbosacral junction in long fusions to the sacrum.
INTRODUCTION
Failure of S1 screw fixation and distal pseudarthrosis are common complications following long fusions to the sacrum [1-9]. To address these problems, extending fixation to the ilium became a common practice in long fusions to the sacrum in order to provide a strong distal foundation to sustain the cantilever forces above and reduce strain on the sacrum [10,11].
However, pelvic fixation remains challenging and is associated with substantial rates of complications [2,8,9,12-14]. Furthermore, pelvic fixation involves longer lever arm and stiffer construct, which can increase the risk of proximal junctional kyphosis (PJK) [15,16]. Elimination of the most caudal motion segment by instrumentation is another potential concern because rotational and translational movement exists at the sacroiliac joint (SIJ) [17].
Laminar hooks or sacral foraminal hooks have been utilized for a long time since the Harrington rod system was invented [18-20]. With the advancement of modern pedicle screw instrumentation, however, hooks have lost their popularity. Although some experimental studies have reported increased pullout strength by laminar or foraminal hooks, no clinical studies regarding the utility of hooks in conjunction with a pedicle screw system have been reported [21-23]. We have utilized S1 foraminal hooks as an alternative to iliac screws in long-level fusion surgery to the sacrum. We hypothesized that S1 foraminal hooks could protect S1 screws and provide structural support to the lumbosacral junction comparable to those of iliac screws with preservation of the mobile segment of the SIJ and shortened the construct.
The purpose of this study was to compare the surgical outcomes of S1 foraminal hooks and iliac screws regarding fusion rate at the lumbosacral junction and the protective effects on S1 screws. Also, the correction amount of sagittal alignment was compared between the 2 instruments.
MATERIALS AND METHODS
From January 2017 to December 2019, consecutive patients who underwent long-level instrumentation and fusion to the sacrum for adult spinal deformity were enrolled. Long-level instrumentation was defined as an uppermost instrumented vertebra at or above L1 (at least 6 segments of instrumentation). Patients were divided into 2 groups by mode of augmentation of S1 screws, that is, the S1 foraminal hook group and iliac screw group. Patients who underwent previous fusion surgery across L5/S1 or surgery for infectious disease (including pyogenic spondylitis and tuberculous spondylitis) or trauma were excluded from the study. Patients who did not complete at least 1 year of follow-up were also excluded. Finally, 29 patients were included in the present study.
All patients underwent a staged operation that was a posterior approach for instrumentation and facetectomy and/or laminectomy in the first stage and an oblique retroperitoneal approach followed by oblique lateral interbody fusion (OLIF) and posterior rod assembly in the second stage. In the case of OLIF for L5/S1 due to complex vascular anatomy or retroperitoneal adhesion, a posterior lumbar interbody fusion (PLIF) was done alternatively. In the S1 foraminal hook group, hooks were placed at the first dorsal sacral foramen in an upward fashion, after foraminal preparation with a hook trial (Fig. 1). All procedures were performed by a single surgeon at one academic institution.

A 66-year-old woman who underwent fusion from T10 to the sacrum with S1 foraminal hooks. (A) Preoperative x-ray showed lumbar kyphosis and severe sagittal imbalance. (B) Follow-up x-ray showed correction of sagittal imbalance with proportional global alignment. (C and D) She achieved distal fusion without instrument failure at the lumbosacral junction. Note the S1 foraminal hooks anchored at the first dorsal foramina (thick arrow). LL, lumbar lordosis; SS, sacral slope; PI, pelvic incidence; SVA, sagittal vertical axis; GAP, global alignment and proportion.
Clinical data, including sex, age, body mass index, period of follow-up, comorbidities, American Society of Anesthesiologists physical status classification, and primary or revision surgery status (any lumbar surgeries except the lumbosacral junction), length of hospital stay, and operative details were collected retrospectively through medical chart review. Spinopelvic parameters including pelvic incidence (PI), lumbar lordosis (LL), sacral slope (SS), sagittal vertical axis (SVA), and proximal junctional angle (PJA) were obtained from the picture archiving - and communication system. Postoperative values were measured by standing x-ray at an early postoperative period (from 4 to 6 weeks postoperatively) and the last visit. LL was defined as the angle between the superior endplate of L1 and S1. We calculated the global alignment and proportion (GAP) score, which were further categorized as proportioned, moderately disproportioned, and severely disproportioned [24]. The PJA was defined as the angle between the caudal endplate of the uppermost instrumented vertebrae and the cephalad endplate of the 2 supraadjacent vertebrae above those vertebrae. PJK was defined as a PJA of at least 10° greater than the early preoperative value. Proximal junctional failure (PJF) was defined as a fracture of uppermost instrumented vertebrae (UIV) or UIV+1, a pullout of instrumentation at UIV, and/or sagittal subluxation [24]. The stability of the S1 screws was determined by the incidence of pseudarthrosis at the L5/S1 level and instrument failure (including pullout, periprosthetic halo, or instrument fracture) around S1 screws. The instrument failures of the iliac screws were also assessed separately. Three-dimensional reconstructed computed tomography as well as x-ray were conducted in all patients to determine pseudarthrosis and instrument failure at the lumbosacral junction.
For statistical analyses, we used IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA). A chi-square test or Fisher exact test was used for dichotomous data analysis. A t-test or Mann-Whitney test was employed to analyze differences in categorical variables. A p-value of less than 0.05 was considered statistically significant.
This study was approved by the Institutional Review Board (IRB) of Kyung Hee University Hospital at Gangdong (IRB No. KHNMC 2021-01-032).
RESULTS
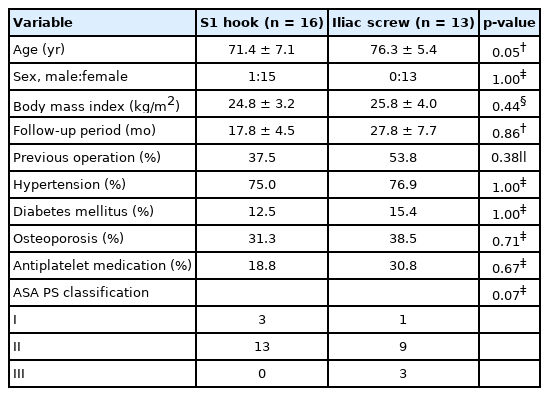
Data from 29 patients (1 man and 28 women) with a mean age of 73.6±6.8 years were evaluated (Table 1). The mean follow-up period was 48.1±22.4 months. Thirteen patients (44.8%) had a history of previous spinal surgery. Regarding the mode of sacropelvic fixation, 16 patients (55.2%) had S1 foraminal hook fixation, and 13 patients (44.8%) had iliac screw fixation. Age, sex, body mass index, length of follow-up, comorbidities, and previous operation history did not differ significantly between the 2 groups.
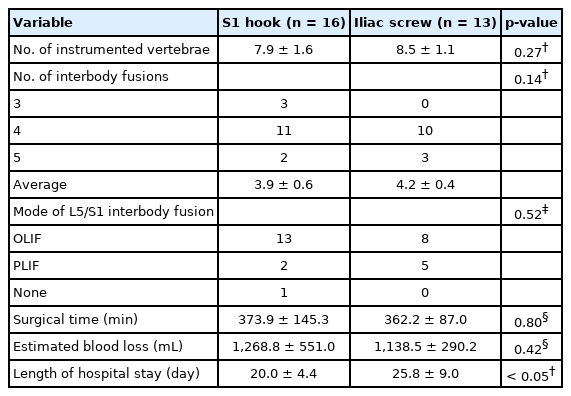
The operative details are summarized in Table 2. The mean number of instrumented vertebrae was 8.1±1.4, with a mean level of interbody fusion of 4.1±0.5. The most common mode of interbody fusion at the lumbosacral junction was OLIF (n=21, 72.4%), followed by PLIF (n=7, 24.1%). The S1 foraminal hook group and iliac screw group did not show significant differences in terms of the number of instrumented vertebrae (7.9±1.6 vs. 8.5±1.1, p=0.27), level of interbody fusion (3.9±0.6 vs. 4.2±0.4, p=0.14), mode of interbody fusion at the lumbosacral junction (OLIF in 81.3% vs. 61.5%, p=0.52), operation time (373.9±145.3 minutes vs. 362.2±87.0 minutes, p=0.80), and surgical bleeding (1,268.8±551.0 vs. 1,138.5±290.2, p=0.42). The mean length of hospital stays was significantly longer in the iliac screw group (25.8±9.0 days) than in the S1 hook group (20.0±4.4 days, p=0.049).
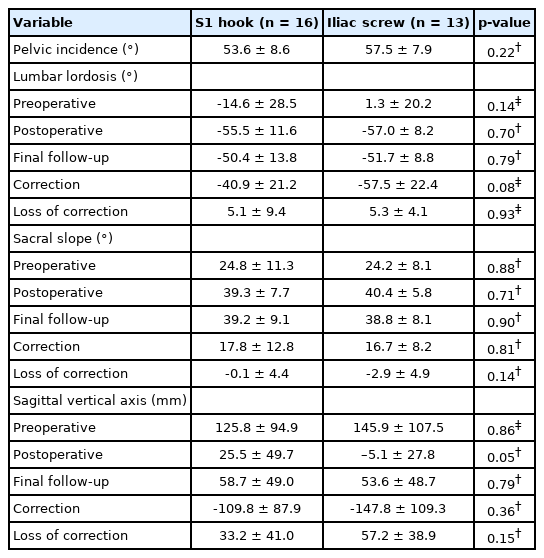
The radiographic outcomes are summarized in Table 3. For all patients, the mean PI was 55.3°±8.4°. The mean preoperative LL was -7.3°±25.8°, which was corrected to -56.2°±10.1°. Preoperative LL (-14.6°±28.5° vs. 1.3±20.2, p=0.14), and postoperative LL (-55.5°±11.6° vs. -57.0°±8.2°, p=0.70) did not differ between the groups. The correction amount of LL was greater in the iliac screw group (-57.5°±22.4°) compared to that of the S1 hook group (-40.9°±21.2°); however, the difference was not statistically significant (p=0.08). Regarding SS, the preoperative value (24.8°±11.3° vs. 24.2°±8.1°, p=0.88) and postoperative value (39.3°±7.7° vs. 40.4°±5.8°, p=0.71) did not show significant differences. Also, the correction amount of SS was not different between the groups (17.8°±12.8° vs. 16.7°±8.2°, p=0.81). Regarding the SVA, the preoperative value (125.8±94.9 mm vs. 145.9±107.5 mm, p=0.86) and postoperative value (25.5±49.7 mm vs. -5.1±27.8 mm, p=0.05) did not differ between the groups. Also, the amount of correction (-109.8±87.9 mm vs. -147.8±109.3 mm, p=0.36) of the SVA did not differ between the groups.
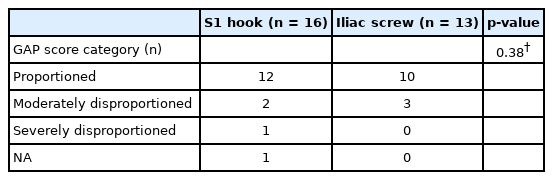
Postoperative GAP scores were calculated and compared between the groups (Table 4). In total, most cases (22 of 29, 75.9%) were classified into the proportioned category, followed by the moderately disproportioned (5 of 29, 17.2%), and severely disproportioned (1 of 29, 3.4%) categories. The GAP score was not available for one patient who could not sustain an upright position. GAP scores did not differ significantly between the 2 groups (p=0.30).
The incidence of pseudarthrosis and mechanical complications at the lumbosacral junction are summarized in Table 5. In total, the rates of pseudarthrosis and instrumentation failure at the lumbosacral junction were 17.2% (5 of 29) and 24.1% (7 of 29), respectively. All cases of instrument failure at the lumbosacral junction were S1 screw loosening (Fig. 2). There were no cases of screw pullout or instrument fracture. The incidence of PJK/PJF was 20.7% (6 of 29). Significantly more patients suffered from L5/S1 pseudarthrosis in the S1 foraminal hook group (5 of 16, 31.3%) than in the iliac screw group (0 of 13, 0%; p=0.048). Instrument failure at the lumbosacral junction showed a trend toward greater frequency in patients with S1 foraminal hooks (6 of 16, 37.5%) than in those with iliac screws (1 of 13, 7.7%); however, the difference did not reach statistical significance (p=0.09). There were 4 patients (30.8%) with failure of iliac screws (periprosthetic halo in 3 patients and set screw extraction in 1 patient) among 13 patients. The rate of PJK or PJF was lower in patients with S1 foraminal hooks (2 of 16, 12.5%) than in those with iliac screws (3 of 13, 30.8%), without statistical significance (p=0.36). Among patients with iliac screws, 2 patients underwent additional surgery due to bilateral rod fractures and 1 patient refused revision surgery for PJK. In patients with S1 foraminal hooks, however, no patient underwent revision surgery until the last follow-up. The rates of revision surgery did not reach statistical significance (p=0.19).
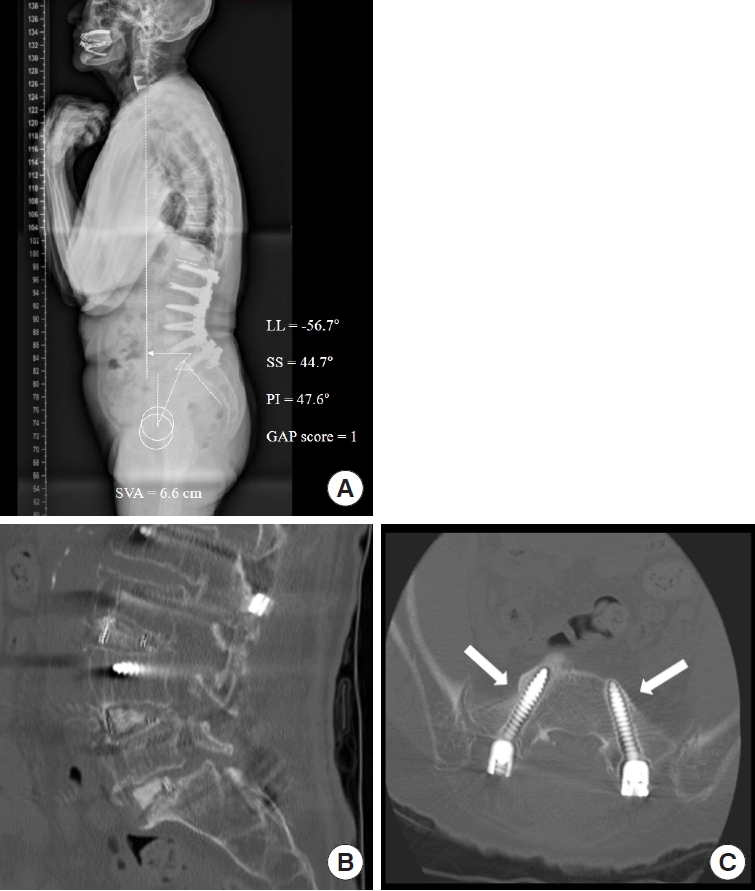
A 79-year-old woman who underwent fusion from L1 to the sacrum with S1 foraminal hooks. (A) Follow-up x-ray showed mild residual sagittal imbalance (SVA=6.6 cm). (B and C) Computed tomography revealed L5/S1 pseudarthrosis and a periprosthetic halo (thick arrows) was identified around the S1 screws. LL, lumbar lordosis; SS, sacral slope; PI, pelvic incidence; SVA, sagittal vertical axis; GAP, global alignment and proportion.
DISCUSSION
In this study, we evaluated the outcomes of augmentation methods using S1 screws (S1 foraminal hook and iliac screws) in long fusions to the sacrum. In terms of correction of spinopelvic parameters, including LL, SS, and SVA, the results of S1 foraminal hooks seemed acceptable and comparable to those of iliac screws. Also, regarding parameters associated with GAP scores, the results did not differ between the groups. Therefore, utilization of S1 hooks resulted in proportional global alignments as well as corrections of the sagittal curve that were comparable to those of iliac screws. However, S1 foraminal hooks were associated with significantly higher rates of L5/S1 pseudarthrosis (31.3% vs. 0%, p=0.048) and an insignificant trend toward higher instrument failure rates (37.5% vs. 7.7%, p=0.09) compared to iliac screws. Regarding structural support to S1 screws, therefore, utilization of S1 foraminal hooks seemed to provide insufficient structural support to the lumbosacral junction.
Pseudarthrosis and instrument failure at the lumbosacral junction are well-known complications of long fusions to the sacrum. To address these problems, recent studies have recommended several methods to reduce the pseudarthrosis rate, including bicortical S1 screws, additional pelvic fixation, and anterior column support at the lumbosacral junction [10,11,25]. In recent years, iliac screw fixation and S2 alar-iliac screw fixation have been considered common procedures for pelvic fixation [25].
The routine conduction of pelvic fixation for augmentation of S1 screws often ignores or thinks less of the segmental motion of SIJ. However, SIJ is the most caudal mobile segment with 1° to 4° of rotation and 1 to 3 mm translation, known as nutation and counternutation [26-30]. Therefore, following a long fusion surgery that eliminates segmental motion through the lumbosacral area, the SIJ becomes the only mobile segment. The residual motion of SIJ following long fusions, including sacropelvic fixation, could lead to failure of iliac screws [25,31]. The reported rates of iliac screw failure ranges from 7.2% to 52% of patients, which is consistent with our findings (4 of 13, 30.8%) [1,9,25,31,32].
Previous studies reported lumbar stiffness following lumbar fusion could restrict activities of daily living (ADL) of patients [33-36]. Kimura et al. [35] demonstrated that as the number of fused segments increased, the number of limitations in ADL increased. Although the impact of sacropelvic fixation on ADL is inconclusive, no studies have been conducted on direct comparisons between sacral fixation and pelvic fixation [34,36,37]. We speculate that pelvic fixation across the SIJ may further restrict ADL by sacrificing the entire mobile segment; thus S1 foraminal hooks can be utilized as an alternative to the iliac screws. Although sufficient and proportioned correction of sagittal alignment was produced, S1 foraminal hooks did not provide enough structural support at the lumbosacral junction, which was inferred from higher rates of pseudarthrosis.
We suggest a possible explanation for the inferior stability of S1 foraminal hooks. First, S1 foraminal hooks have biomechanically inherent vulnerability because the implant must stand behind the lumbosacral pivot point. As McCord et al. [38] described previously, the more anterior position of the construct achieved with respect to the lumbosacral pivot point, the more stable the construct. Theoretically, S1 foraminal hooks tend to move apart from the pivot point during flexion, resulting in decreased resistance against pullout strength [39]. Utilizing S1 foraminal hooks, however, we achieved an equivalent sagittal realignment by cantilever force without any case of S1 screw or S1 foraminal hook pullout. Moreover, the loss of sagittal correction did not differ between groups in terms of LL (5.1°±9.4° vs. 5.3°±4.1°, p=0.93) and SVA (33.2±41.0 mm vs. 57.2±38.9 mm, p=0.15). Previous researchers also demonstrated that utilizing hooks could increase the bending stiffness of the construct and pullout strength of S1 screws in experimental studies [22,23]. Therefore, we assume S1 foraminal hooks could protect S1 screws at least in terms of pullout strength. Second, variable types of functional loading exist on the transverse plane and coronal plane as well as sagittal plane to the spinal column. Even if S1 foraminal hooks, by their claws, could resist the pullout strength during stress on the sagittal plane [21-23], they could hardly resist the toggling moments, unlike the iliac screws, because only a part of the surface maintains bone to hardware contact. Therefore, the inability of S1 foraminal hooks to resist 3-dimensional functional loading could be the cause of failure to achieve sufficient stability at the lumbosacral junction.
It is interesting that the incidence of PJK/PJF was lower in the S1 hook group (12.5%), compared to that of iliac screw group (30.8%), although the difference did not reach statistical significance (p=0.36). A longer and stiffer construct is known to result in a higher prevalence of PJK owing to increased range of motion and higher stress at the adjacent segment [16,40-42]. In addition to sacral fixation, iliac fixation was described as a distinct risk factor for PJK by Bridwell et al. [15]. We think that utilizing S1 foraminal hooks, instead of iliac screws, may protect adjacent segment degeneration and subsequent PJK by reducing the length and stiffness of the construct. The relationship between S1 foraminal hooks and PJK, however, is beyond the scope of this study.
This study is limited by its retrospective nature and lack of randomization. The enrolled population was small with a short follow-up period. Because there were beginning cases of OLIF at the L5/S1 level, surgical results could be biased because of technical problems such as incomplete endplate preparation or cage positioning. Lastly, the lack of patient-reported clinical outcomes is another weakness. Although this study focused on the radiographic outcomes of S1 foraminal hooks, future studies assessing clinical outcomes with larger populations and longer follow-up periods are necessary.
CONCLUSION
We compared the surgical outcomes of S1 foraminal hooks and iliac screws in long fusions to the sacrum. S1 foraminal hooks achieved equivalent satisfactory correction of the sagittal alignment with proportioned global alignment compared to iliac screws. However, S1 foraminal hooks showed a significantly higher rate of L5/S1 pseudarthrosis and a trend toward higher rates of instrument failure without statistical significance compared to those of iliac screws. Utilization of S1 foraminal hooks seemed to have insufficient structural support to the lumbosacral junction in long fusions to the sacrum.
Notes
The authors have nothing to disclose.