Prioritization of Realignment Associated With Superior Clinical Outcomes for Cervical Deformity Patients
Article information
Abstract
Objective
To prioritize the cervical parameter targets for alignment.
Methods
Included: cervical deformity (CD) patients (C2–7 Cobb angle > 10°, cervical lordosis > 10°, cervical sagittal vertical axis [cSVA] > 4 cm, or chin-brow vertical angle > 25°) with full baseline (BL) and 1-year (1Y) radiographic parameters and Neck Disability Index (NDI) scores; patients with cervical [C] or cervicothoracic [CT] Primary Driver Ames type. Patients with BL Ames classified as low CD for both parameters of cSVA (< 4 cm) and T1 slope minus cervical lordosis (TS–CL) (< 15°) were excluded. Patients assessed: meeting minimum clinically important differences (MCID) for NDI (< -15 ΔNDI). Ratios of correction were found for regional parameters categorized by primary Ames driver (C or CT). Decision tree analysis assessed cutoffs for differences associated with meeting NDI MCID at 1Y.
Results
Seventy-seven CD patients (mean age, 62.1 years; 64% female; body mass index, 28.8 kg/m2). Forty-one point six percent of patients met MCID for NDI. A backwards linear regression model including radiographic differences as predictors from BL to 1Y for meeting MCID for NDI demonstrated an R2 of 0.820 (p=0.032) included TS–CL, cSVA, McGregor’s slope (MGS), C2 sacral slope, C2–T3 angle, C2–T3 SVA, cervical lordosis. By primary Ames driver, 67.5% of patients were C, and 32.5% CT. Ratios of change in predictors for MCID NDI patients for C and CT were not significant between the 2 groups (p>0.050). Decision tree analysis determined cutoffs for radiographic change, prioritizing in the following order: ≥ 42.5° C2–T3 angle, > 35.4° cervical lordosis, < -31.76° C2 slope, < -11.57-mm cSVA, < -2.16° MGS, > -30.8-mm C2–T3 SVA, and ≤ -33.6° TS–CL.
Conclusion
Certain ratios of correction of cervical parameters contribute to improving neck disability. Prioritizing these radiographic alignment parameters may help optimize patient-reported outcomes for patients undergoing CD surgery.
INTRODUCTION
Incidence of adult cervical deformity (CD) as a distinct clinical diagnosis is rising, along with the literature concentrating on methodology for appropriately assessing the disease [1]. As the condition is often associated with major disability and neurologic compromise, surgical correction of malalignment and addressment of symptoms are often warranted [2,3]. Numerous studies have demonstrated radiographic alignment and achievement of sagittal balance as significant drivers of health-related quality of life (HRQoL) improvement in deformity patients, not specific to the cervical spine [4-6]. Moreover, studies investigating the connection between cervical alignment parameters and HRQoL outcomes are limited.
Restoration of cervical sagittal alignment involves neural element decompression and/or fusion of the cervical and caudal spinal regions, often invasive in nature and poses risks for major complications and poor patient-reported outcomes [7]. Many patients are unable to undergo these major, invasive CD corrective procedures due to deformity severity, old age, comorbidities, and severe frailty status. And, often baseline characteristics (body mass index [BMI], age, Charlson Comorbidity Index [CCI] score, frailty score) imply increased risk for certain postoperative complications and decline in HRQoL outcomes [8,9]. Alignmentadjustments have been explored in the adult spinal deformity (ASD) population. Lafage et al. [10] proposed a modified version of the validated SRS-Schwab ASD classification accounting for varying age ranges. More rigorous alignment objectives were determined to be warranted for younger patients, while less rigorous alignment objectives for elderly patients, in order to achieve normative HRQoL scores for each age population [10]. This alignment specificity for the individual patient needs to be considered in order to optimize patient-reported outcomes.
Explicitly, when assessing deformity specific to the cervical spine, a standardized classification system of deformity severity is in its preliminary stages. The most well-known classification was created by Ames and the International Spine Study Group, but it has yet to be formally validated with connection to HRQoL outcomes [11-13]. Little is known regarding the order of addressing correction of certain cervical alignment parameters for peak improvement in postoperative patient-reported outcomes [14,15]. Using a prospective multicenter collection of CD surgical patients, this study investigated the prioritization of cervical alignment parameters and their minimal degree of correction that contributes to optimal quality of life.
MATERIALS AND METHODS
1. Data Source and Inclusion Criteria
This was a retrospective cohorts study of a prospective, multicenter International Spine Study Group (ISSG) database of CD patients enrolled from 2013–2018 at 13 participating centers around the United States. Institutional Review Board approval was required protocol by each site and informed patient consent was obtained. Patients enrolled in the database were greater than 18 years with evidence of one of the following CD baseline radiographic parameters: cervical kyphosis (C2–7 Cobb angle > 10°), cervical scoliosis (C2–7 coronal Cobb angle > 10°), C2–7 sagittal vertical axis (SVA) > 40 mm, or chin-brow vertical angle (CBVA) > 25°. Database exclusion criteria comprised of patients with spinal deformity of neuromuscular etiology, presence of active infection, or malignancy. The study inclusion criteria required complete baseline (BL) and 1-year (1Y) radiographic measurements and the HRQoL measure, Neck Disability Index (NDI), as well as demonstrated cervical or cervicothoracic Ames sagittal deformity driver descriptor. The Ames deformity driver consists of 5 categories, detailing the primary driver of cervical deformity as follows: C, a primary sagittal deformity apex in cervical spine; CT, a primary sagittal deformity apex at the cervicothoracic junction; T, primary sagittal deformity apex in the thoracic spine; S, a primary coronal deformity (C2–7 Cobb angle greater than or equal to 15); and CVJ, a primary craniovertebral junction deformity. In order to analyze a more homogenous CD population, patients were excluded if they were categorized with another Ames driver (thoracic [T], coronal [S]) or were classified as a low Ames CD modifier for both the parameters of cervical SVA (cSVA) (< 4 cm) and T1 slope minus cervical lordosis (TS–CL) (< 15°).
2. Data Collection, Radiographic, and HRQoL Assessment
Patient demographic and clinical data assessed patient age, sex, BMI, and CCI. Operative factors assessed: surgical approach, levels fused, operative time, and estimated blood loss (EBL). Full-length free-standing lateral spine radiographs were used to assess the patient population at BL and 1Y. Radiographs were analyzed with SpineView (ENSAM, Laboratory of Biomechanics, Paris, France) software according to the literature [16-18]. Radiographic parameters assessed included cSVA, C2–7 lordosis, TS–CL, CBVA, McGregor’s slope (MGS), C2–T3 SVA, C2–T3 angle, C2 slope. The health-related-quality of life questionnaire utilized in this study was the NDI administered by each of the participating centers.
3. Statistical Analysis
Descriptive analyses determined demographic, clinical, and surgical data. Frequency analysis evaluated categorical variables with chi-square analysis determining significant variance of expected versus observed values. Patients were assessed based on meeting the minimal clinically important difference (MCID) for NDI scores at 1nyear (< -15 ΔNDI) [19]. Proportion (%) and difference of correction from preoperative measurement to 1 year were calculated for the following regional parameters: cSVA, CL, T1 Slope, TS–CL, CBVA, MGS, C2–T3 SVA, C2–T3 angle, and C2 slope. Backwards linear regression model including the radiographic differences (1Y–BL) as predictors for meeting MCID for NDI found the parameters that contributed the greatest variation (with a significantly large R2 value). The radiographic measures included in the model were then assessed for proportion of correction stratified by C or CT Ames primary driver type. Analysis of variance compared the C and T ratios for any significant differences. Decision tree analysis determined cutoff values of the radiographic difference variables included in the backwards regression model, accomplished through iteration of multivariate regression equations. Radiographic change cutoffs were prioritized based upon their ordinal regression values when entered as sole predictors for meeting MCID for NDI through binary logistic regressions. All statistical analyses were performed using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA) and R-statistical package (www.r-project.org). All analyses were 2-sided and the level of significance was set to < 0.05.
RESULTS
1. Overall Cohort Patient Characteristics
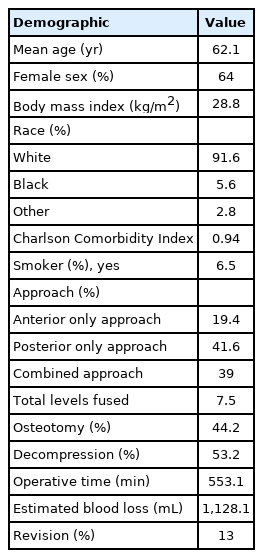
Seventy-seven CD patients with complete radiographic and HRQoL data met inclusion criteria for Ames driver descriptors of C or CT. Twelve patients with S or T Ames driver descriptors were excluded. Mean patient age was 62.1 years, mean BMI of 28.8 kg/m2, with 64% of the cohort as female. The average CCI score was 0.94. By approach, these CD patients underwent majorly posterior surgeries (41.6%), while 39% had combined approaches and 19.4% anterior. Forty-four point two percent of patients underwent osteotomies and 53.2% decompression. Average levels fused was 7.5 (posterior, 8.3; anterior, 3.5). The mean total operative time was 553.1 minutes, with an EBL of 1,128.1 mL. Thirty-two patients (41.6%) met MCID for NDI. Ten patients (13%) had a revision procedure. Table 1 summarizes the demographic and basic surgical factors for the cohort.
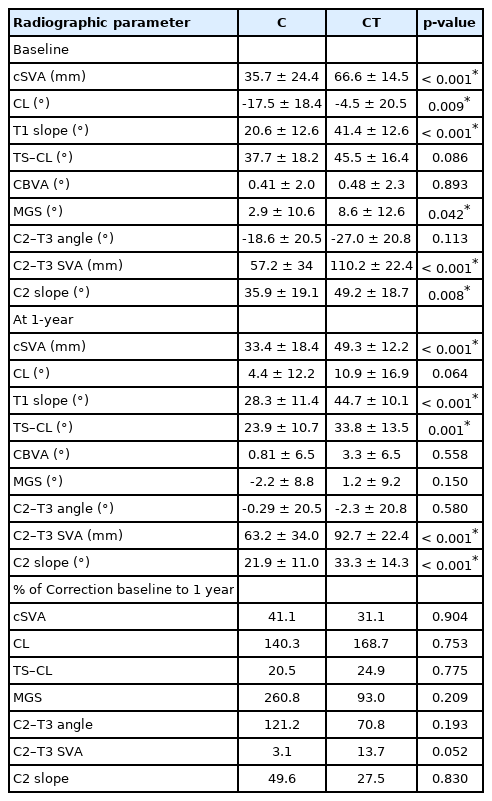
2. Baseline and 1-Year Radiographic Parameters Between C and CT Ames Drivers
Between C and CT groups, there were significant differences for both baseline and 1-year cohort means of cSVA, T1 Slope, C2–T3 SVA, and C2 slope. CT patients exhibited significantly greater malalignment at baseline for cSVA (66.6 mm vs. 35.7 mm, p<0.001), T1 slope (41.4° vs. 20.6°, p<0.001), C2–T3 SVA (110.2 mm vs. 57.2 mm, p<0.001), as well as MGS (p=0.042) and C2 slope (p=0.008). C driver patients had greater CL malalignment preoperatively (-17.5° vs. -4.5°). At 1-year CT patients remained significantly more malaligned in cSVA, T1 slope, C2–T3 SVA, and C2 slope (all p<0.001) (Table 2).
3. Radiographic Corrective Measures Predictive of Meeting MCID for NDI
A backwards linear regression model found the following radiographic differences as predictors of meeting MCID for NDI from baseline to 1 year: TS–CL, cSVA, MGS, C2 slope, C2–T3 angle, C2–T3 SVA and CL demonstrated the greatest variation contributing to MCID for NDI with an R2 of 0.820 (p=0.032). When assessing individual Ames driver type cohorts, C driver patients demonstrated an R2 value of 0.844 (p=0.029) without inclusion of the TS–CL or C2–T3 SVA parameter. CT patients had an R2 value of 0.778 (p=0.025), without the TS–CL angle.
4. Ratios (%) of Correction in Predictors by Ames Driver
Ratios of change in predictors for MCID NDI patients (BL-1Y) for C driver patients: 260.8% MGS, 140.3% CL, 121.2% C2–T3 angle, 49.6% C2 slope, 41.1% cSVA, 20.5% TS–CL, 3.1% C2–T3 SVA. Correction in CT driver patients included: 168.7% CL, 93% MGS, 70.8% C2–T3 angle, 31.1% cSVA, 27.5% C2 slope, 24.9% TS–CL, 13.7% C2–T3 SVA. The ratios of radiographic differences were not significant between the C and CT driver groups (p>0.050) (Table 2).
5. Prioritization of Realignment Parameters and Their Corrective Cutoff Values
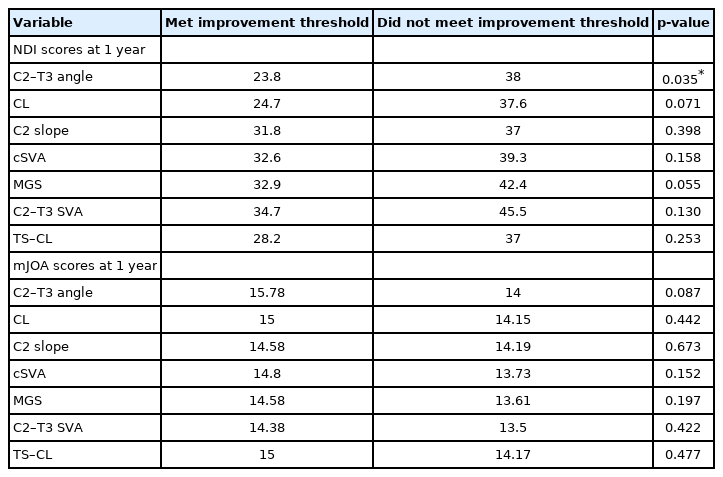
Decision tree analysis determined cutoffs for radiographic change, prioritizing in the following order (based upon ordinal regression values): a correction ≥ 42.5° C2–T3 angle (odds ratio [OR], 5.667; 95% confidence interval [CI], 1.074–29.891; p=0.041), > 35.4° CL (OR, 4.636; 95% CI, 0.857–25.071; p=0.075), < -31.76° C2 slope (OR, 3.2; 95% CI, 0.852–12.026; p=0.085), <-11.57-mm cSVA (OR, 3.185; 95% CI, 1.137–8.917; p=0.027), < -2.16° MGS (OR, 2.724; 95% CI, 0.971–7.636; p=0.057), > -30.8-mm C2–T3 SVA (OR, 0.462), and ≤ -33.6° TS–CL (OR, 0.271) (Table 3).
6. HRQoLs for Patients With Ideal Prioritization
Patients who met thresholds for recommended cervical parameter prioritization trended toward improvement in both NDI and modified Japanese Orthopedic Association (mJOA) scale for all measurements at 1 year (Table 4).
7. Case Examples
Fig. 1 shows the baseline and 1-year lateral cervical and whole spine radiographs of a 72-year-old female (BMI, 33.3 kg/m2) and a history of diabetes mellitus and osteopenia who underwent CD corrective surgery. She presented with cervical type Ames driver. According to proposed CD prioritization guidelines, this patient did not meet proposed prioritization correction thresholds for C2–T3 angle (-1.60°), CL (+11.9°), C2 slope (-0.54°), cSVA (-2.03 mm), MGS (+4.11°), and TS–CL (-0.69°). She did meet the threshold for C2–T3 SVA (+16.8 mm). The patient had a 1-year NDI score of 46, did not meet MCID for NDI, and patient-reported mJOA score of 15.
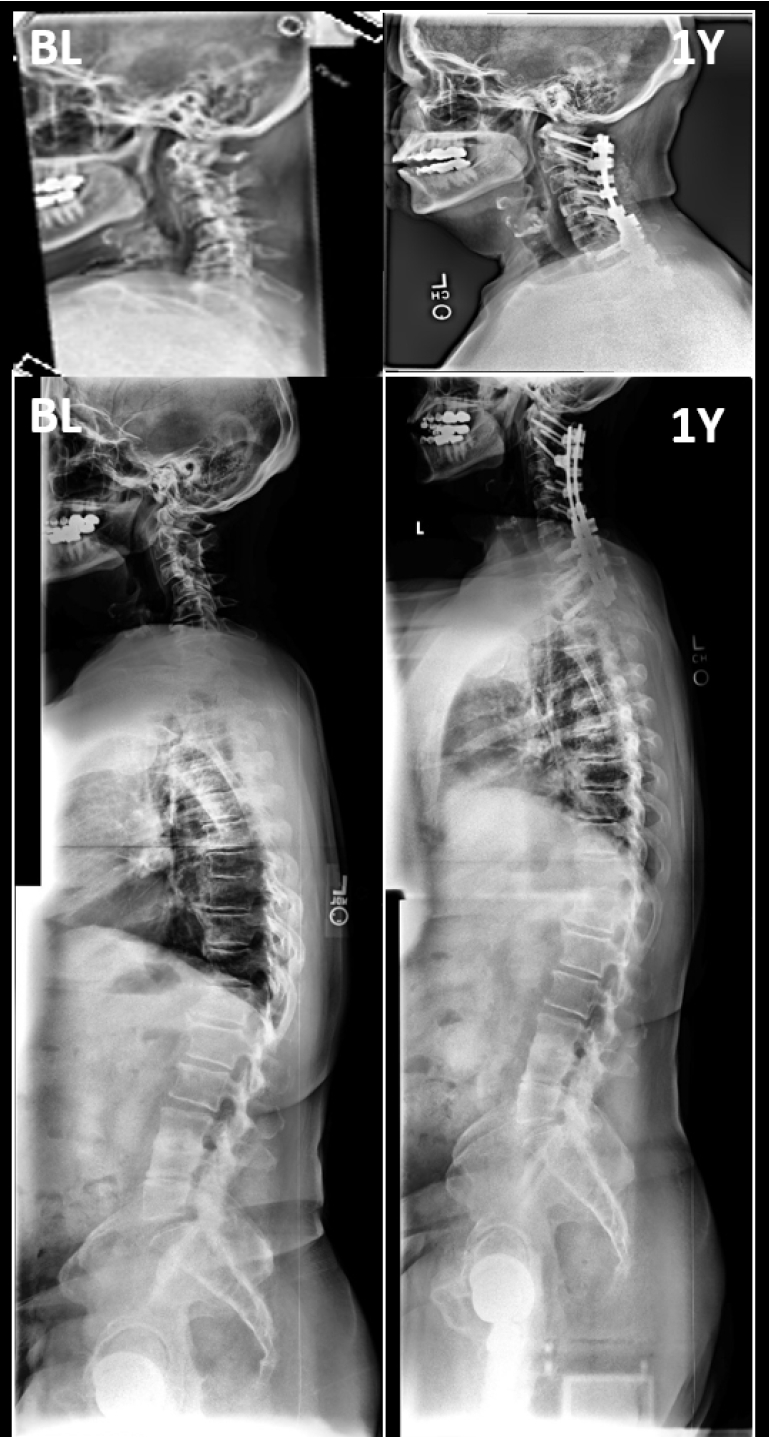
Baseline (BL) and 1-year (1Y) cervical and whole spine radiographs of a 72-year-old female who did not meet proposed radiographic prioritization of alignment.
Fig. 2 shows the baseline and 1-year lateral cervical and whole spine radiographs of a 61-year-old male (28.97 kg/m2) who underwent CD corrective surgery. He presented with cervical type Ames driver. According to proposed CD prioritization guidelines, this patient did meet all proposed prioritization correction thresholds for C2–T3 angle (+76.1°), CL (+67.9°), C2 slope (-44.9°), cSVA (-11.9 mm), MGS (-10.8°), C2–T3 SVA (+11.7 mm), and TS–CL (-45.8°). The patient had a 1-year NDI score of 11.1, met MCID for NDI, and patient-reported mJOA score of 18.
DISCUSSION
High-risk cohorts undergoing treatment of adult CD include patients with advanced age, obesity, greater comorbidity burden, and severe frailty status. While classification systems, such as the one created by Ames and the ISSG, provide correction guidelines for the representative majority of CD patients, operating on patients with preoperative presentation of increased risk for poor outcomes has facilitated the need for a prioritization of alignment scheme for CD surgery [13]. Therefore, the goal for this analysis was to establish an order of targeting alignment parameters and their projected minimal corrective degree to benefit operative decision-making and inherently improve HRQoL outcome management.
Utilizing a CD prospective multicenter database and biplanar stereoradiography, allowing for the acquisition of full-body imaging in the weight-bearing position, our analysis determined that prioritizing regional cervical radiographic alignment parameters in a certain order to a specific degree optimized reaching the MCID in a patient’s self-reported neck disability. Despite regional driver of CD (cervical or cervicothoracic), radiographic correction for patients who reached MCID for NDI were similar. The prioritization of parameters are as follows: C2–T3 angle, C2–7 lordosis, C2 slope, cSVA, MGS, C2–T3 SVA, and, lastly, TS–CL.
First, we found that the C2–T3 angle should be corrected. This angle connects each of the regions of the spine, by incorporating the unequivocal relationship between the cervical and thoracolumbar spine morphology [20-22]. By prioritizing next the C2–7 lordosis correction, the natural cervical curvature is addressed secondarily. Cervical kyphosis is a major radiographic presentation of CD, with a strong connection to clinical impact, so direct correction to parameters encompassing the curve is imperative for improved patient-reported outcomes [20]. In a previous study by Passias et al. [23], the preoperative cervical degree of lordotic compensation and higher C2–T3 angle were identified as risk factors for sagittal malalignment and decline in HRQoL outcomes after thoracolumbar surgery. With prioritization of the lordosis of the spine, combined with the cervicothoracic junction as a site of transition between the highly mobile cervical and rigid thoracic systems, we can address the inherent relationship between cervical sagittal malalignment and clinical measures of disability [24].
The third parameter to prioritize in correction of CD is the C2 slope. We found that correction of this radiographic measurement, led to increased neck disability improvement [25]. This parameter is a singular CD factor, a mathematical approximation of the mismatch between T1 slope and cervical lordosis [26]. By factoring in the occipitocervical spine, the C2 slope accounts for an additional aspect of radiographic alignment improvement and should be prioritized accordingly.
Then, the cSVA was found to be prioritized. The restoration of this parameter has been correlated with improved postoperative outcomes and prevention of disability [27]. It incorporates a global assessment of CD by measuring the distance between the C2 and C7 plumblines [28]. Tang et al. [29] suggested that an increasing cervical SVA is a cause for clinical concern of cervical malalignment, as > 40 mm was correlated with worse NDI outcomes. As one of the main objectives of CD surgery is the maintenance or restoration of horizontal gaze, the next parameter to prioritize was found to be MGS [30]. By correcting this angle, the symptoms of inability to look straight ahead or lie down flat that contribute to overall disability can be addressed. Another parameter appreciating cervical sagittal alignment is the C2–T3 SVA, which was found to be 6th measure of prioritization. Prioritizing the 2 large measures of cervical sagittal alignment (C2–C7 SVA and C2–T3 SVA), accounting for the alignment of subjacent segments, including the thoracolumbar spine and pelvis, along with horizontal gaze measurement, the global outlook of the spine is assessed.
Lastly, the mismatch between T1 slope and CL parameter was prioritized. This relationship accounts for the intrinsic compensation of T1 slope on the CL to balance the head over the thoracic inlet and maintain the physiological neck tilting [31,32]. The measure accounts for the patient’s center of gravity, and contributes to overall cervical integration into global alignment.
Through the combination of regional cervical radiographic factors, we found that prioritizing the lordosis of the cervical spine (through C2–C7 and C2–T2), followed by occipitocervical incorporation (C2 slope) global assessment (cSVA, C2–T3 SVA, TS–CL), and horizontal improvement (MGS). This proposed prioritization involves the innate interdependence of the spine: cervical lordosis depends on both thoracic kyphosis and lumbar lordosis. With the distinct diagnosis of CD, cervical lordosis adaptation is due to the cervical spinal segment changes relative to the global spine to attempt to maintain the head over the pelvis and horizontal gaze [28]. Addressing the intertwined cervical parameters in a specific order to a certain degree of correction can contribute to improved patient-reported neck disability.
Our study is not without limitations, including the retrospective nature of this study and the small number of patients. While the multicenter methodology used for database construction increases the generalizability of our findings, the data analyzed for the purposes of this study may be skewed toward more complex cases. Another limitation lies in the heterogeneous nature of the patient population in regards to cervical procedure and complexity, which may have been accounted for by removing thoracic and coronal Ames type CD drivers. The method of radiographic measurement is also not without limitation. Although the measurements were standardized to be taken with the patient standing in a relaxed position looking forward, these images remain as a representation of a point in time and are not reflective of force plate of dynamic motion studies. However, the horizontal gaze tends to stay stable and lower extremities ted to affect lumbo-pelvic alignment the most. Future studies should investigate the proposed prioritization and thresholds on a prospective trial with a larger, homogenous population of patients undergoing CD corrective surgery.
CONCLUSION
Certain ratios of correction of cervical parameters contribute to improving neck disability. Specific cutoffs of radiographic differences from baseline to 1 year were found prioritizing C2–T3 angle, followed by cervical lordosis, C2 slope, C2–7 plumb line, MGS, C2–T3 SVA, and TS–CL all strongly associated with meeting the MCID for the NDI score. Prioritizing these radiographic alignment parameters may help optimize patient-reported outcomes for patients undergoing CD surgery.
Notes
The authors have nothing to disclose.
Acknowledgements
The International Spine Study Group (ISSG) is funded through research grants from DePuy Synthes and individual donations.