Spinal Tuberculosis: Always Understand, Often Prevent, Sometime Cure
Article information
To the editor,
As an old global epidemic, tuberculosis (TB) has been threatening human lives for thousands of years. Still today, about 2 billion people are infected with TB, and 1.7 million deaths occur each year worldwide [1]. In addition, many TB patients are undiagnosed or not reported [2]. Spine is the most common site of extrapulmonary TB, accounting for 50% of skeletal TB [3]. Spinal TB caused by mycobacterium tuberculosis (Mtb) which typically spreads via hematogenous path, and then erodes the vertebral body from anterior to posterior. Spinal TB has a characteristic loss of bone density in anterior part of vertebra at first, which tends to create a kyphotic deformity historically named as Pott disease. The intervertebral disc is often the last to be affected, which differs from a typical pyogenic infection. This is often distinguished with the use of magnetic resonance imaging. Spinal TB can be confirmed by histological cultures and laboratory testing.
The typical symptoms and signs of patients infected with TB include fatigue, back pain, weight loss, night sweats, and fevers. Spinal TB generally has an insidious progression with 3 major clinical features: cold abscess, neurologic deficits, and a kyphotic deformity [4]. Compression of the neurological elements from either an abscess or from the kyphotic deformity, often leads to neurologic deficits. In adults with spinal TB, the kyphotic deformity is commonly less than 30°. In children patients, kyphosis may continue to progress during the course of disease, leading to a much larger deformity. This population may require a more timely surgery. Globally, TB is a major cause of death and disability among children, especially in low-income and middle-income countries, yet children have often been neglected in TB control efforts [5].
To prevent relevant complications, spinal TB requires prompt antitubercular chemotherapy, but delays are more commonplace compared with pulmonary TB [6]. Preventive therapy for the susceptible is an effective strategy to eliminate this disease [7]. People with high-risk factors including immunodeficiency (such as human immunodeficiency virus [HIV] coinfection), malnutrition, and overcrowded living conditions, tend to be at higher risk of TB. Adolescents with spinal TB are an at-risk group for contracting and spreading TB in school. Treatment and prevention of spread, can include some social distancing, relative isolation, and the wearing of a facemask. Throughout this process, psychosocial support should not be ignored. The most widely used regimen to prevent TB is isoniazid for 6–12 months, while rifampicin or rifapentine combined isoniazid for 3 months can also be used. Furthermore, a 90% reduction in the risk of TB development among contacts that were provided by fluoroquinolone [7]. In high-burden countries, preventive therapy is usually limited to spinal TB patients with HIV. In low-burden countries, it can be used for immigrants and latent patients. To avoid cross-infection in suspected patients, the wearing of a surgical mask can become a vitally important part of disease control. Recently, vaccination and detection with whole genome sequencing (WGS) were included in the preventive strategies. Immunization with Bacillus Calmette-Guérin vaccine can protect infants, children, and adults from TB infection. Due to the higher confidence in strain identity, rapid detection of drug resistance with WGS may be available for outbreak investigations.
The understanding of tuberculotic epidemiology and pathophysiology continues to evolve and refine TB treatment. Therapeutic strategies for spinal TB include holistic treatment for TB, and local therapy for spine. The both approaches are related. Holistic antituberculous medication is the cornerstone that consists of isoniazid, rifampicin, pyrazinamide, and ethambutol given for 2 months, followed by isoniazid and rifampicin managed for an additional 4 months [7]. World Health Organization (WHO) recommends that TB patient should be offered with daily fixed-dose combinations [8]. The medical managements of adults and children with spinal TB are almost identical except the dosing of medications. Surgery is a supplementary therapy for patients with neurological deficits, kyphosis greater than 60°, or for pediatric patients with “spine-at-risk” signs. Local debridement for cold abscess, decompression for neurologic deficits, and realignment for kyphosis could be performed for selected patients with spinal TB (Fig. 1). In our experience, spinal instrumentation with the use of titanium cages, plates, and screws, can stabilize and correct the spinal deformity, without the risk of graft rejection or inflammatory response [9].
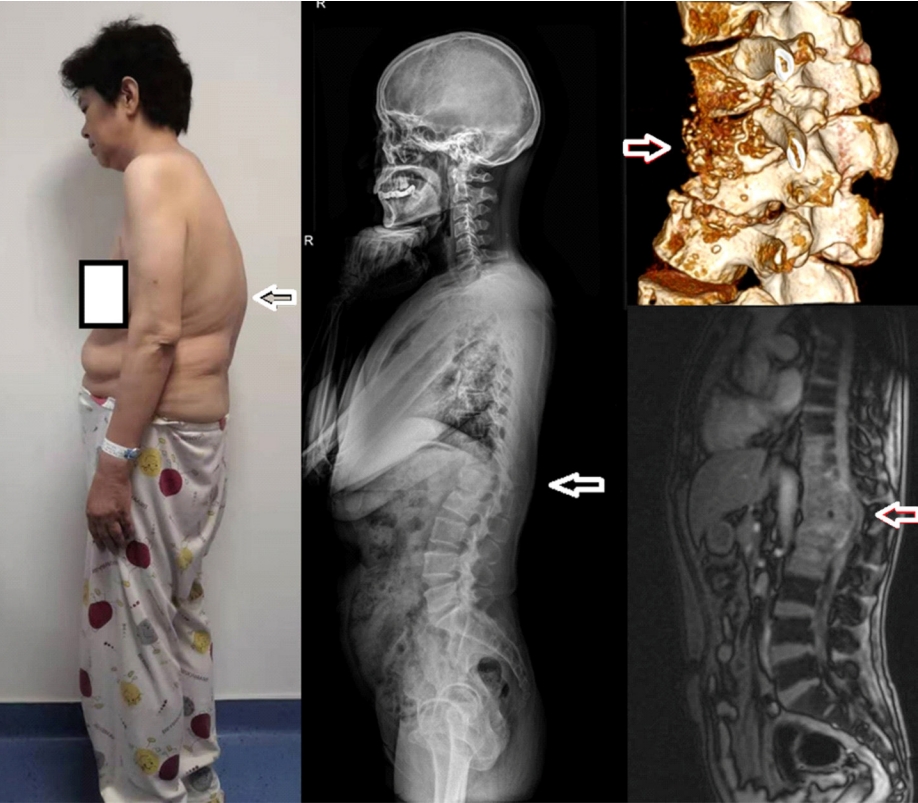
A patient with kyphotic spinal tuberculosis (white arrows indicate tuberculotic lesions). The written informed consent had been received from the patient for publication.
Drug-resistant TB is a threat that leads to high mortality and one third of deaths in patients with TB worldwide [10]. The incidence of rifampicin-resistant TB is increasing in Russia, Myanmar, China, and South Africa [11]. The WHO updated guidelines have recommended a multiple drug resistance regimen for TB treatment [12]. And WHO suggests fluoroquinolones to cure patients with isoniazid-resistant TB. In addition, the combination of bedaquiline, pretomanid, and linezolid treating patients with drug-resistant TB led to a favorable outcome after 6-month therapy (90% had the favorable outcomes) [13]. However, whether infected patients can clear Mtb is still unclear, as between 1% and 11% of patients with TB immunoreactivity continue to carry viable bacteria capable of recurring disease [14]. The critical principle for treating TB is to obtain culture samples to make an optimal regimen. But even when the diagnosis is achieved in developing countries, treatment adherence is still difficult to be maintained in long-term. Germicidal ultraviolet irradiation is an affordable assistance method to treat spinal TB. Another problem is that serious adverse drug reaction may interrupt therapeutic course. Fortunately, bedaquiline and delamanid are being used to change the care of people with all forms of TB. In addition, usage of vaccine against TB can offer a wonderful protection [15].
To understand the natural history of spinal tuberculotic infections, preventive and therapeutic strategies need to be developed to adequately contain and treat this challenging disease. Newer rapid nucleic acid tests facilitate to diagnose spinal TB. Community-based interventions are efficient to prevent disease’s outbreak. Anti-TB chemotherapy, nutritional support, and favorable public health are critical to reduce the trigger of spinal TB. In addition, an in-depth psychotherapy should be provided throughout therapeutic course because patients with productive cough, hemoptysis, and spinal kyphosis tend to be self-contemptuous and scared. Also, a multidisciplinary approach should be developed for tuberculotic diagnosis and treatment, which involving epidemiologists, pharmacologists, spine surgeons, and radiologists.
Notes
The authors have nothing to disclose.
