Complications of Posterior Fusion for Atlantoaxial Instability in Children With Down Syndrome
Article information
Abstract
Objective
To clarify the complications of posterior fusion for atlantoaxial instability (AAI) in children with Down syndrome and to discuss the significance of surgical intervention.
Methods
Twenty pediatric patients with Down syndrome underwent posterior fusion for AAI between February 2000 and September 2018 (age, 6.1±1.9 years). C1–2 or C1–3 fusion and occipitocervical fusion were performed in 14 and 6 patients, respectively. The past medical history, operation time, estimated blood loss (EBL), duration of Halo vest immobilization, postoperative follow-up period, and intra- and perioperative complications were examined.
Results
The operation time was 257.9±55.6 minutes, and the EBL was 101.6±77.9 mL. Complications related to the operation occurred in 6 patients (30.0%). They included 1 major complication (5.0%): hydrocephalus at 3 months postoperatively, possibly related to an intraoperative dural tear. Other surgery-related complications included 3 cases of superficial infections, 1 case of bone graft donor site deep infection, 1 case of C2 pedicle fracture, 1 case of Halo ring dislocation, 1 case of pseudoarthrosis that required revision surgery, and 1 case of temporary neurological deficit after Halo removal at 2 months postoperatively. Complications unrelated to the operation included 2 cases of respiratory infections and 1 case of implant loosening due to a fall at 9 months postoperatively.
Conclusion
The complication rate of upper cervical fusion in patients with Down syndrome remained high; however, major complications decreased substantially. Improved intra- and perioperative management facilitates successful surgical intervention for upper cervical instability in pediatric patients with Down syndrome.
INTRODUCTION
Atlantoaxial instability (AAI) occurs in 14.6%–22.2% of individuals with Down syndrome [1-4], which is more frequent than that in normal children and results from ligament laxity and odontoid dysplasia [3]. Surgical treatment of AAI in children with Down syndrome is challenging because of the small bony structures, anatomical variety, and high complication rate. Posterior arthrodesis of the upper cervical spine in patients with Down syndrome had 73.3%–100% of complications in the 1990s [5,6]. While surgeries have been recommended in AAI patients with associated neurological symptoms, prophylactic arthrodesis for asymptomatic cases has been controversial [7-10]. However, perioperative management, including radiographic evaluations, surgical techniques with spinal instrumentation, and anesthesia, has progressed markedly, enabling safer surgery. After posterior fusion with C1–2 transarticular screws was first reported in 1992 [11], C1 lateral mass screws and C2 pedicle screws have been developed and utilized [12,13]. These techniques have been applied in pediatric patients and have demonstrated improved stabilization and fusion rate [14-18]. Although several reports have shown acceptable outcomes in pediatric upper cervical spine surgeries since 2000 [15,16,19-22], they included small populations of Down syndrome. Therefore, the complication rate is difficult to estimate. The purpose of this study was to clarify the complications of posterior fusion for AAI in children with Down syndrome and the significance of surgical intervention.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board (IRB) of Kobe University Graduate School of Medicine (IRB No. B190002). Written informed consent was obtained from each patient and family. Further, they were informed that data from the cases would be submitted for publication and gave their consent. This study was conducted following the principles of the Declaration of Helsinki and with the laws and regulations of Japan.
A total of 20 pediatric patients with Down syndrome underwent posterior fusion for AAI in the authors’ hospitals between February 2000 and September 2018 (7 men and 13 women; age, 6.1±1.9 [3–9] years) (Table 1). Prior to surgery, a combination of lateral cervical radiography, computed tomography (CT), and magnetic resonance imaging (MRI) were performed. The surgical indication was an atlantodental interval (ADI) larger than 7.0 mm with smaller space available for the cord (SAC) than 10.0 mm and os odontoideum even without symptoms. All screws and plates were placed under fluoroscopic guidance. The constructs included C1 lateral mass screws, C2 or C3 pedicle screws, C2 laminar screws, C2 or C3 hooks, rectangular rods with sublaminar wiring, and occipital plates.
The past medical history, operation time, estimated blood loss (EBL), duration of postoperative Halo vest immobilization, postoperative follow-up period, and intra- and perioperative complications of these patients were examined. Values are expressed as the mean±standard deviation. Fisher exact test was used to assess the complication rate between rod-wiring/hook constructs and rod-screw constructs.
RESULTS
C1–2 or C1–3 fusion and occipitocervical (O-C) fusion were performed in 14 and 6 patients, respectively. All patients underwent primary surgeries performed by a single surgeon. Preoperative ADI was 7.6±1.5 mm and SAC was 9.0±2.1 mm. Lateral radiography revealed 1 case of odontoid hypoplasia and the other 19 of os odontoideum. One patient had a hypoplastic posterior arch of the atlas. None of the patients had subaxial instability according to the lateral flexion-extension images. No patients presented abnormal neurological findings preoperatively.
Seventeen patients had past medical history of cardiovascular diseases, such as atrial septal defect (ASD), endocardial cushion defect, patent ductus arteriosus, and ventricular septal defect (VSD); however, their cardiac functions were maintained to tolerate general anesthesia. Hypoacusis or serous otitis media was found in 5; dysopia, 4; and gastrointestinal anomalies in 3 patients. One patient had recurrent pneumonia and bronchitis, although no congenital anomalies were diagnosed in the respiratory system (Table 1).
The operation time was 257.9±55.6 minutes (182–365 minutes) (Fig. 1A), and the EBL was 101.6±77.9 mL (22–330 mL) (Fig. 1B). None of the patients required a transfusion. Postoperative Halo immobilization was applied for 56.1±23.7 days (0–90 days) (Fig. 1C). The postoperative follow-up period was 9.1±4.8 years (2.0–19.8 years).
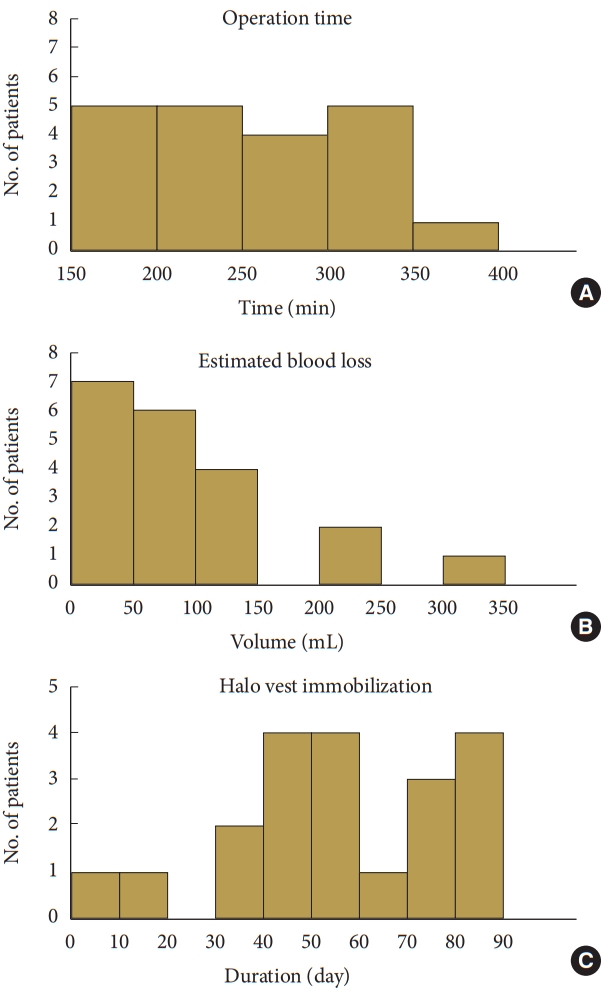
Distribution of intraoperative data and postoperative Halo immobilization. (A) Operation time. (B) Intraoperative estimated blood loss. (C) Duration of Halo vest immobilization.
Complications related to the operation occurred in 6 patients (30.0%) (Table 2). They included one major complication in 1 patient (5.0%): hydrocephalus at 3 months postoperatively, possibly related to an intraoperative dural tear. Other complications included 3 cases of superficial surgical site infections, 1 case of deep infection in the bone graft donor site (iliac crest), 1 case of C2 pedicle fracture, 1 case of Halo ring dislocation at postoperative day 1, 1 case of pseudoarthrosis resulting in a revision surgery, and 1 case of temporary neurological deficit after Halo removal at 2 months postoperatively for an unknown reason. The case with pseudoarthrosis (case 1) had no postoperative complications in the revision surgery, which was not included in this study, and achieved bone union after the second surgery. The other 19 cases obtained bone union within 12 months. The complications that were indirectly related to the operation included 2 cases of respiratory infections and 1 case of implant loosening due to a fall at 9 months postoperatively (Table 3). No permanent or severe neurological complications related to surgery and perioperative death were observed. During the follow-up, no subaxial malalignment significant adjacent disc degeneration, kyphotic changes, or hardware failure were observed.
To clarify the difference of complication rate between the construct type, we compared 3 cases with rod-wiring/hook constructs and 17 cases with rod-screw constructs. Surgery-related complication was observed in 2 cases with rod-wiring/hook constructs and 4 with rod-screw constructs (p=0.20). Surgery-unrelated complication was found in 1 with rod-wiring/hook constructs and 2 with rod-screw constructs (p=0.40).
1. Illustrative cases
1) Case 8
A 6-year-old girl was diagnosed with AAI by a pediatrician; however, she did not present any symptoms of cervical myelopathy or radiculopathy. She underwent cardiac surgery for ASD and VSD at 5 months of age, and her cardiac function was maintained. Lateral radiography indicated that AAI and the atlas were irreducible even at the extension position (Fig. 2A). We performed C1–2 fusion with C1 lateral mass screws and C2 pedicle screws, transplanting a bone graft from the right iliac crest (Fig. 2B). Because this case had an irreducible atlas, we gently release and loosen C1–2 facet joints followed by gradual reduction with C1 lateral mass screws and C2 pedicle screws. Upon reduction, the assistant surgeon carefully pushes the C2 spinous process, and the primary surgeon tightens the screws and rods. The lateral mass screw successfully reduced the dislocation of C1 and enabled the preservation of the posterior arch of the atlas. The operation time was 296 minutes, and the EBL was 330 mL. No intraoperative and postoperative complications were observed. After the application of the Halo vest for 2 months, followed by a cervical collar for 8 months, bone union was achieved. At the latest follow-up, 6 years postoperatively, no deterioration was found in clinical symptoms and radiographic features (Fig. 2C).
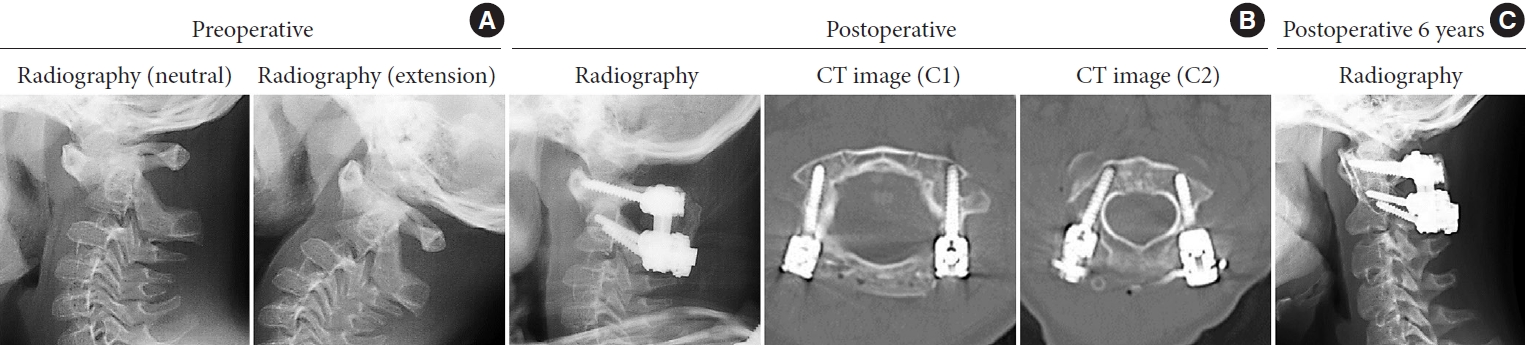
Case 8. Six-year-old girl. (A) Preoperative lateral radiograph of the cervical spine at neutral and extension positions. C1 was irreducible even at the extension position. (B) Postoperative lateral radiography and computed tomography (CT) reconstruction of C1 and C2. Successful reduction of C1 and appropriate insertion of screws are shown. (C) Lateral radiograph at the latest follow-up at 6 years postoperatively. No instrument-related abnormal findings and subaxial deformity were found.
2) Case 9
A 4-year-old girl was diagnosed with AAI by a pediatrician, although she did not have any neurological symptoms. She underwent surgery for ASD at 6 months of age and her cardiac function was assessed to tolerate general anesthesia and cervical surgery. Lateral radiography indicated that AAI and the atlas were overreduced, that is posterior subluxation, at the extension position (Fig. 3A). We performed C1–2 fusion with C1 lateral mass screws and C2 pedicle screws, transplanting a bone graft from the right iliac crest (Fig. 3B). In the cases of os odontoideum with posterior subluxation of atlas, os odontoideum protrudes into the spinal canal. Therefore, overreduction could result in cord compression and we have made a careful and mild reduction of the atlas. Because a dural tear occurred during the surgery, the tear was repaired using Prolene sutures. The operation time was 365 minutes, and the EBL was 120 mL. Although slight superficial infection and protracted wound healing with subcutaneous accumulation of cerebrospinal fluid (CSF) were observed, no other complications were found until Halo removal at 2 months postoperatively. Four days after Halo removal, she developed a convulsive seizure. Brain CT showed hydrocephalus and ventriculoperitoneal shunting was performed immediately. Hydrocephalus gradually resolved (Fig. 3C). After the application of a cervical collar for 10 months, bone union was achieved. At the latest follow-up, 6 years postoperatively, no deterioration was found in clinical symptoms and radiographic features (Fig. 3D).

Case 9. Four-year-old girl. (A) Preoperative lateral radiograph of the cervical spine at neutral and extension positions. C1 was overreduced (posterior subluxation) at the extension position. (B) Postoperative lateral radiography and computed tomography (CT) reconstruction of C1 and C2. Appropriate C1 reduction and screw insertion are shown. (C) Brain CT images after the diagnosis of hydrocephalus. Dilated cerebral ventricles were found, and ventriculoperitoneal shunting was performed. Hydrocephalus resolved after 3 months. (D) Lateral radiograph at the latest follow-up at 6 years postoperatively. No instrument-related abnormal findings and subaxial deformity were found.
DISCUSSION
The surgery-related complication rate of upper cervical fusion in pediatric patients with Down syndrome remained high at 30.0%. However, the percentage of major complications decreased substantially (5.0%), and no life-threatening or surgery-related severe neurological complications occurred. The overall complication rate in the current study was comparable to that reported in adult patients with rheumatoid arthritis (8.1%–41.8%) [23-25]. A strength of this study was relatively large population treated by a single surgeon, while a review/meta-analysis article has been published including various backgrounds and treatments [26].
Neurological complications are occasionally unpredictable; however, they can be minimized by the development of management approaches, such as preoperative imaging, intraoperative fluoroscopic guidance or navigation, and neurophysiological monitoring [26]. One patient (case 3) showed temporary muscle weakness in the right upper and lower limbs after Halo removal at 3 months postoperatively. However, the cause of muscle weakness could not be identified, even with image inspection. This late-phase neurological complication can only be recognized and handled by careful postoperative observation. Hydrocephalus, found in case 9, is not a common complication of spinal surgery. Several cases have been reported as late complications: 1 month after a C2 dumbbell tumor resection [27], 10 months after lumbar decompression and fusion [28], and 5 months after a stab injury to the upper cervical spine [29]. They do not appear to be specific to Down syndrome but are related to dural tear and repair. In case 9, the detailed cause of hydrocephalus is unclear. However, the patient exhibited dural tear followed by subcutaneous accumulation of CSF without any neurological symptoms under Halo vest immobilization and developed a convulsive seizure after Halo removal at postoperative 2 months. Thus, we estimated that dural tear and CSF leakage could be related to hydrocephalus. Once a dural tear is recognized, careful and long-term postoperative follow-up is warranted for symptoms, such as headache, nausea, and convulsions. In cases 3 and 9, these complications were observed immediately after Halo removal. Complications related to Halo vest immobilization are frequent in children [30,31], most of which are pin site infections and loosening. Although neurological complications immediately after Halo removal has not been reported or elucidated, the sudden change in the axial pressure or alignment could have triggered the complications in our cases. The reason why we apply Halo vest immobilization is the difficulty in rest due to mental retardation and the demand for rigid fixation in the light of systemic joint laxity in Down syndrome. We applied Halo vest for 3 months when only hooks and wiring are available. However, after using lateral mass/pedicle screws, we have shortened the duration; as short as 1 month. We regard Halo vest as a support for bone union in patients with Down syndrome.
Pseudoarthrosis may be a major concern in fusion surgery for Down syndrome. For successful bone union, rigid fixation and substantial bone grafting are required [10], in which C1 lateral mass screws play a key role. The C1 lateral mass screws not only facilitate improved stabilization but also enable reduction of the dislocated atlas. This results in the preservation of the posterior arch of the atlas, which is a precious bed for bone grafting, as shown in case 8. A recent meta-analysis showed that screw fixation for pediatric AAI in patients with Down syndrome significantly reduced the loss of reduction or pseudoarthrosis [26]. Segal et al. [5] reported that 10 pediatric patients with Down syndrome had cervical or O-C fusion with modified Gallie technique, resulting in 100% surgery-related complications. Among their cases, 7 of 10 patients exhibited graft absorption and/or hardware failure, which could be related to insufficient fixation. Doyle et al. [6] reported 15 patients with Down syndrome, including 9 pediatric cases. In their study, 10 of 15 patients showed nonunion and/or loss of reduction, which could be caused by a lack of rigid fixation. In our cases, especially after adopting C1 lateral mass screw, we consider that rigid fixation has been achieved owing to advance in the cervical instrumentation and the surgical techniques. This may be one reason for lower complication rate. Stabilization with C1 lateral mass screws helps avoid O-C fusion and maintain the O-C motion segment. Initially, we selected C1–2 fusion if the atlas was reducible at extension position of lateral radiography and O-C fusion if it was irreducible. However, after demonstrating that C1 lateral mass screws can reduce the irreducible atlas, we apply O-C fusion only for the cases in which C1 lateral mass screws cannot be inserted. We extended the fusion to C3 when we used hook/wiring or C2 was not available as an anchor due to anatomical reasons. After we started using C1 lateral mass screws for pediatric patients in 2009, no pseudoarthrosis was found in C1–2 fusion cases. However, rigid fixation in children can affect the growth of the C2 vertebral body and fused-disc height, as well as the subaxial alignment [22,32,33]. Although there were no cases with postoperative subaxial malalignment in our study, radiographic evaluation should be carefully continued.
Another concern is infection. Four surgical site infections, including 3 superficial infections and 1 deep infection, and 3 respiratory infections were found in our patients. Postoperative infection may be related to immunodeficiency in patients with Down syndrome [34], which is not easy to prevent completely. The most optimal efforts should be careful observation and appropriate treatment once the infection is recognized.
A radiographic guideline, suggested in 2005, stated that surgical intervention is required when the ADI is > 9.9 mm or the ADI is 4.5–10 mm with neurological deficit and evidence of spinal cord compression on MRI [35]. In this guideline, high-risk activities, such as gymnastics and soccer, were restricted when the ADI was higher than 4.5 mm even without neurological abnormalities, which indicated that even low-energy head injury could damage the spinal cord in these patients. While the incidence of symptomatic AAI is 10.0%–17.5% in all pediatric AAI patients with Down syndrome [3,8], it is difficult to predict the progressive widening of the ADI and the appearance of neurological deficits due to the lack of evidence in the natural course of AAI. Therefore, careful radiographic follow-up and physical assessment are required. Furthermore, we recommend early surgical intervention even without symptoms; our current surgical indication for AAI in pediatric patients with Down syndrome is an ADI larger than 7.0 mm with symptoms or an ADI larger than 7.0 mm with smaller SAC than 10.0 mm and os odontoideum without symptoms. We regard os odontoideum as a possible indicator of severe AAI. The cases with os odontoideum could have posterior subluxation at extension position as shown in case 9, which is sometimes difficult to point out. Because anterior arch rides on the axis at extension in posterior subluxation, careful interpretation of radiography is warranted. A high complication rate may have been the main reason why patients with Down syndrome are hesitant to undergo surgery. However, our results demonstrated that the rate is no longer extremely high compared to that in patients with other comorbidities such as rheumatoid arthritis.
This study has several limitations. First, the study has a retrospective design. Second, although O-C fusions and C1–2 fusions may differ in terms of their surgical invasion or stress for patients, we included them together. This difference could affect the incidence or severity of the complications. While we did not find specific complications to O-C fusions or C1–2 fusions, this difference could affect the incidence or severity of the complications.
CONCLUSION
While careful preoperative preparation and postoperative observation are undoubtedly needed, improved intra- and perioperative management can facilitate successful surgical intervention for upper cervical instability in pediatric patients with Down syndrome. Although the overall complication rate of upper cervical fusion in Down syndrome remains high, clinicians should not hesitate to select surgical intervention.
Notes
The authors have nothing to disclose.



