Regional Anesthesia for Lumbar Spine Surgery: Can It Be a Standard in the Future?
Article information
Abstract
This paper is an overview of various features of regional anesthesia (RA) and aims to introduce spine surgeons unfamiliar with RA. RA is commonly used for procedures that involve the lower extremities, perineum, pelvic girdle, or lower abdomen. However, general anesthesia (GA) is preferred and most commonly used for lumbar spine surgery. Spinal anesthesia (SA) and epidural anesthesia (EA) are the most commonly used RA methods, and a combined method of SA and EA (CSE). Compared to GA, RA offers numerous benefits including reduced intraoperative blood loss, arterial and venous thrombosis, pulmonary embolism, perioperative cardiac ischemic incidents, renal failure, hypoxic episodes in the postanesthetic care unit, postoperative morbidity and mortality, and decreased incidence of cognitive dysfunction. In spine surgery, RA is associated with lower pain scores, postoperative nausea and vomiting, positioning injuries, shorter anesthesia time, and higher patient satisfaction. Currently, RA is mostly used in short lumbar spine surgeries. However, recent findings illustrate the possibility of applying RA in spinal tumors and spinal fusion. Various researches reveal that SA is an effective alternative to GA with lower minor complications incidence. Comprehensive insight on RA will promote spine surgery under RA, thereby broadening the horizon of spine surgery under RA.
INTRODUCTION
Regional anesthesia (RA), which includes epidural anesthesia (EA) via catheter infusion and spinal anesthesia (SA) via singleshot injection, is commonly used for procedures of known duration that involve the lower extremities, perineum, pelvic girdle, or lower abdomen [1-8]. The literature notes numerous advantages of RA over general anesthesia (GA), including favorable perioperative hemodynamic stability, reduced mortality, intraoperative blood loss, arterial and venous thrombosis, pulmonary embolism, myocardial infarction, renal failure, and decreased incidence of cognitive dysfunction [9-15].
Even though RA is widely accepted in other fields, the use of RA during elective lumbar surgery failed to gain wide acceptance [1-5,16]. GA is the preferred and most commonly used anesthesia technique for lumbar spine surgery such as microdiscectomy or lumbar decompression [1,7,17-20]. This may be due to greater acceptance by patients, the ability to easily extend the duration of an operation using GA, and/or anesthesiologist preference for GA because of a more secure airway establishment during the prone position [5,21]. Also to consider RA, it is important to assess the nature and duration of surgery, patient comorbidities, the ease of spinal insertion (i.e., positioning and spinal pathology), and the relative benefits and risks to the individual. Nonetheless, RA has been reported to be a safe and effective as GA for lumbar spine surgery of short duration [1-5,7,15,22-26]. Considering the wide usage of RA in other surgical fields, RA can have many applications in lumbar spine surgery.
This paper is an overview of various features of RA. Our knowledge of RA for spine surgery is largely based on very limited data. The aim of the study was to introduce spine surgeons unfamiliar with RA and to promote lumbar spine surgery under RA. We will discuss RA from a spine surgeon’s point of view, rather than giving specifics about the anesthesia itself.
WHAT IS REGIONAL ANESTHESIA?
RA, also called neuraxial anesthesia, can be used while you are awake or in combination with sedation or GA. SA (via single-shot injection) and EA (via epidural catheter) are the most commonly used RA methods. SA is also called a spinal block, subarachnoid block, intradural block, and intrathecal block. It is a form of neuraxial RA involving the injection of a local anesthetic and/or opioid into the subarachnoid space. The local anesthetic and/or opioid injected into the cerebrospinal fluid (CSF) provides anesthesia, analgesia, and motor and sensory blockade. Otherwise, EA injects analgesics and local anesthetics through a catheter placed into the epidural space. The injection can result in a loss of sensation including pain by blocking the transmission of signals through nerve fibers in or near the spinal cord. EA can be used both during and after surgery for pain management.
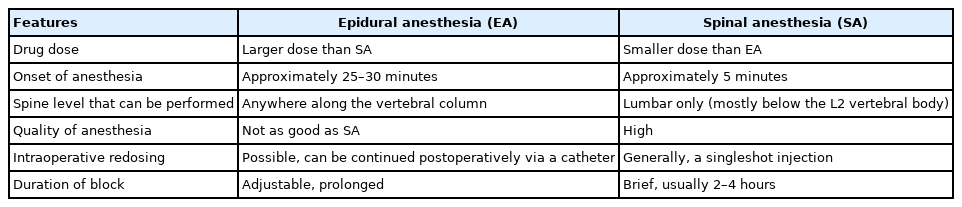
DIFFERENCES BETWEEN EPIDURAL ANESTHESIA AND SPINAL ANESTHESIA
The similarities between SA and EA often confuse people that they are the same anesthetic techniques. Important differences are summarized in Table 1. Generally, EA requires a larger drug dose than SA. The onset of analgesia is slower with EA (> 20 minutes) than SA (< 5 minutes), which also causes a more gradual decrease in blood pressure. EA can be performed anywhere along the vertebral column including cervical, thoracic, lumbar, and sacral vertebrae. For EA, the epidural catheters are punctured at least 2 intervertebral levels above the surgical level (e.g., for the L5–S1 at the L3–4 intervertebral space) [27]. Adequate anesthesia was considered usually at the T6–10 for spinal surgery. EA can perform an epidural block postoperatively through an already inserted epidural catheter. SA is mostly performed below the second lumbar vertebral body to avoid piercing the spinal cord and consequently damaging the spinal cord. SA wears off in a cephalad to caudad direction, thus sacral levels will last longer than thoracic. The anesthetic effect of SA after a single-shot injection usually lasts about 2–4 hours.
There is also a method of combined SA and EA (CSE) [28]. It is a method that pursuits the reliability of SA and the flexibility of EA simultaneously. The dose of local anesthetics for SA can be reduced so that the spinal level of sensory block is lowered, and adverse effects can be reduced. The advantage of CSE is the ability to use a low dose of intrathecal local anesthetic, with the preparation that the epidural catheter may be used to extend the block if necessary. This allows surgeons not to be chased during anesthesia, helping surgeons to focus on the operation itself.
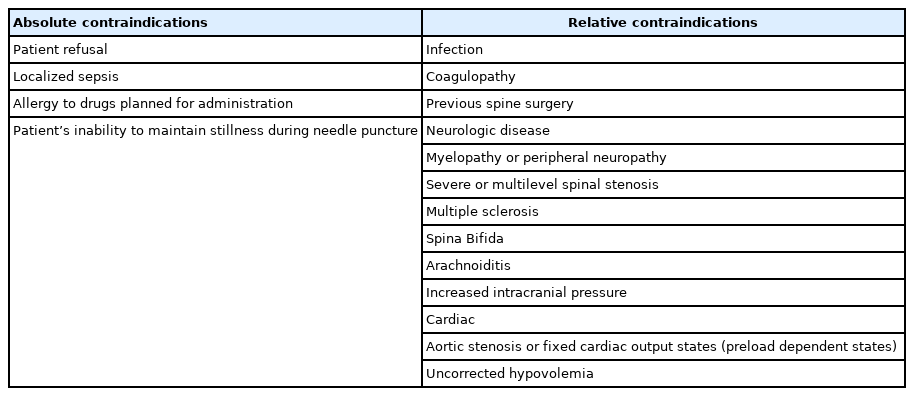
CONTRAINDICATIONS TO REGIONAL ANESTHESIA
There are few contraindications to RA and are summarized in Table 2 [2,4,17,23,24,29,30]. The most important absolute contraindication is patient refusal. Surgeons, as well as anesthesiologists, should be concerned about the patient’s anxiety. Others include localized infection and allergy to drugs planned to be administered for the anesthesia. A patient’s inability to stay still during needle puncture, which may lead to traumatic injury to the neural structures [31], as well as increased intracranial pressure, which may cause brainstem herniation [32], should be accounted as absolute contraindications to RA.
Patients with coagulopathy including taking antiplatelets/anticoagulants are relatively contraindicated due to the risk of an epidural hematoma. The history of previous lumbar spine surgery also increases the risk of nerve damage due to anatomical changes and epidural adhesions. The spread of local anesthetics may be restricted by scar tissue. Undetermined neurological disease is a relative contraindication. Demyelinating diseases such as multiple sclerosis (MS) should be careful when considering RA due to their increased susceptibility to local anesthetic toxicity. However, there is no clear evidence that RA exacerbates the neurological symptoms of MS [33]. It is safe not to undergo RA if it deviates from the normal anatomical vertebral structure. Traditionally, RA has been considered contraindicated in patients with preload (volume) dependent states such as aortic stenosis due to the risk of acute decompensation in response to decreased systemic vascular resistance. The patients with hypovolemia may exhibit an exaggerated hypotensive response to the vasodilatory effects of RA which results in a sympathectomy 2–6 dermatomes above the sensory block.
Additionally, there are contraindications specific to spine surgery patients. Severe or multilevel spinal stenosis, near completetotal myelographic block, or myelographic demonstration of arachnoiditis is contraindicated [24].
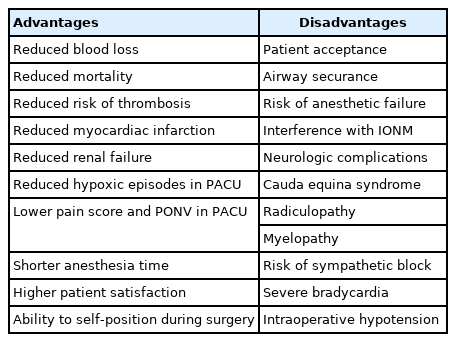
ADVANTAGES OF REGIONAL ANESTHESIA
The pros and cons of RA are summarized in Table 3. Compared to GA, RA is associated with reduced intraoperative blood loss [12,13,34,35], reduced mortality, arterial and venous thrombosis, pulmonary embolism, perioperative cardiac ischemic incidents, renal failure, and hypoxic episodes in the postanesthetic care unit (PACU) [9,10,36]. Though there are conflicting results, RA is associated with lower postoperative morbidity and mortality compared with GA [10,37], and decreased incidence of cognitive dysfunction [11].
In the case of spine surgery, RA is associated with lower pain scores during PACU stay, shorter anesthesia time, and higher levels of patient satisfaction than GA after spinal surgery [1]. Multiple studies show RA is associated with decreased incidence of postoperative nausea and vomiting [3,21,23,38,39], due to its reduced systemic side effects and less cerebral-targeted drug action [3]. RA offers the patient self-position in prone cases. This is likely to reduce the chance of positioning injuries, such as brachial plexus injury, complications related to head malposition, such as pressure necrosis of the face, blindness, and pressure sores [5,21,23]. Further, SA is more time-efficient than GA. The use of SA for lumbar spine surgery showed 19 minutes of shorter anesthesia time compared to GA [7]. By using continuous EA, the patient can manage postoperative pain via epidural analgesia, which provides better pain control and lower stress response [39].
DISADVANTAGES OF REGIONAL ANESTHESIA
There are concerns in using neuraxial anesthesia in patients with spinal pathology. There are decreased patient acceptance and a problem with securing the airway [5,21]. There is a need for multiple attempts and risk of failure due to anatomical changes, either induced by previous interventions or pre-existing. It was reported that patients with spine pathology are prone to experience paresthesia during SA conduction [40]. It is challenging for the patient to maintain a prone position for a long duration while awake, so GA is preferred in procedures lasting more than 2 hours or with excessive blood loss [5]. If an awake patient should move during the procedure, the nerve could be injured. Though these problems have never been reported, it is hard to denounce the possibility [3,13,23,38]. Intraoperative neuromonitoring is obsolete with RA since it interferes with voltage-gated sodium channels in neural synapses, reducing neuro-axis transmission [4].
Serious neurologic complications are rare, but RA has a risk of cauda equina syndrome and invariably results in permanent neurologic deficit [41]. RA occasionally causes neurologic sequelae such as radiculopathy or myelopathy and in patients with severe spinal stenosis not undergoing lumbar surgery, SA has been associated with an increased risk of new neurologic deficit [42].
RA can cause blockade of thoracic sympathetic fibers originating at T1–5, leading to the development of severe bradycardia or intraoperative hypotension [43]. The upper sensory level should be at T10 or higher to provide adequate anesthesia. However, high levels of motor block are poorly tolerated in the prone position due to lack of abdominal muscle strength and the inability to breathe deeply against increased abdominal pressure [5]. Due to these reasons, surgery higher than T10 is not recommended under neuraxial anesthesia.
CURRENT UTILIZATION OF REGIONAL ANESTHESIA IN SPINAL SURGERY
A recent meta-analysis on this matter analyzed previous randomized studies [3]. RA is mostly used in lumbar spine surgery, especially in microdiscectomy and lumbar decompression. As described above, neuraxial anesthesia in spine surgery is limited to T10, due to strenuous breathing and the possibility of thoracic sympathetic blockade, which can lead to severe bradycardia or intraoperative hypotension [5,43]. Also, the use of RA illustrating lumbar fusion was very limited in literature. However, more recent evidence proposes the possibility of applying RA in other spinal surgeries. In their preliminary paper, Ogrenci et al. [44] focused on the possibility of using SA in spinal tumor surgery in elderly patients. Tumorectomy and fusion of the spinal columns were performed in the patient group. Cheng and Chen [45] illustrated the use of RA in thoracic spinal stenosis patients. Percutaneous endoscopic thoracic decompression was performed under local anesthesia in patients with lower thoracic lesions. However, they did not specify the anesthetic methods. Several studies, including a randomized controlled trial, used regional anesthesia to perform minimally invasive transforaminal interbody fusion and showed a positive outcome [46-48]. More recent evidence shows RA can be used in revision surgery for lumbar pseudoarthrosis in a patient with a high risk for GA [49].
DISCUSSION
The use of RA for lumbar spine surgery has been strongly debated. Yet RA is a safe and efficacious technique for lumbar spine surgery [13,21,50]. The literature regarding spinal anesthesia used for lumbar decompression is largely supportive, suggesting spinal anesthetic is at least comparable with general anesthesia in terms of safety and efficacy and that it may be superior to general anesthesia in some ways [7,21]. A retrospective review investigated the outcomes of elective lumbar spine surgery under SA to GA [38]. The study demonstrated SA is an effective alternative to GA and had lower minor complications incidence.
Compared to GA, RA showed favorable hemodynamic status, reduced blood loss, and postoperative analgesic requirements in randomized controlled trials (RCTs) [13,24,27,35]. Studies show reduced blood loss in patients undergoing spine surgery with RA [12,13,24,27,34,35]. This is most likely due to a combination of sympathetic blockade, producing vasodilation and hypotension, coupled with lower intra-thoracic pressure generated by spontaneous breathing by patients [21]. In the case of an intraoperative laceration of the dura (with consecutive loss of CSF), no alteration of the SA effect happens. The receptors are blocked just after the injection, so a loss of CSF does not reduce the SA effect.
Previous researcher [38] found deep venous thrombosis was significantly more common in patients who had undergone GA than RA. Reduced thrombo-embolic complications have also been reported in spine surgery patients receiving RA. This is probably related to either faster mobility and/or modulation of the hypercoagulable state that occurs and persists after major surgery, and the preventive effect of RA in postoperative inhibition of fibrinolysis [38,51].
In terms of mortality, Guay et al. [37] reported a systematic review comparing GA and RA, illustrating a lower mortality rate by approximately 2.5% in surgery with an intermediate-to-high cardiac risk, and the risk of perioperative pneumonia. In an overview of randomized trials, mortality was reduced by a third in patients under RA [9].
There are conflicting results on lower postoperative pain score [13,17,24,27,30,50]. However, recent RCT showed a strong association with lower pain scores during PACU stay, lower postoperative nausea and vomiting, and high levels of patient and surgeon satisfaction after RA [1,2,24].
On the other hand, RA is believed to increase the risk of sympathetic block causing severe bradycardia or intraoperative hypotension, or risk of causing cauda equina syndrome or other neurologic complications such as radiculopathy and myelopathy [41,42]. The lumbosacral roots are vulnerable to direct exposure to large doses of anesthetics and neurotoxic properties of local anesthetics may lead to irreversible neuron damage if less diluted within the CSF [52]. There is a widespread acceptance of GA in spine patients and anesthesiologists prefer GA since a secure airway can be achieved in prone position [5,21].
1. Suitable Patients and Surgeries
Factors favoring the use of RA over GA are relatively limited in current literature. In general, RA is considered feasible in patients undergoing surgeries with a duration of less than 2 hours and with less predicted blood loss [53]. Currently, RA is most widely used and deemed acceptable in decompressive lumbar surgeries. RA is a better alternative for patients with risk for GA-related complications. Currently, patients with medical comorbidities with an American Society of Anesthesiologists (ASA) physical status classification grade of III or IV are not considered eligible for spinal surgery under GA. It has been shown that when major medical comorbidities are present, performing spinal surgery under RA is a safe and effective alternative to GA [54].
2. Future Application of Regional Anesthesia
Despite some drawbacks, the results point to the likelihood that RA can be widely used in elderly patients. The average life expectancy is increasing with the development of medical technology and the number of geriatric populations who require surgical treatment is increasing accordingly. Due to a lack of physiologic reserve, elderly patients are exposed to higher anesthetic risk. Nevertheless, as physical activity contributes to multiple aspects of the quality of life, more surgical treatment can be required for elderly patients to pursue active physical activity. Therefore, an anesthetic method with low anesthetic risk is enticing to the geriatric population.
A recent study evaluated the risks of GA in patients 66 or older undergoing spinal surgery. Deyo et al. [55] reported a 3.1% (984 out of 32,152 patients) of major medical complications, including cardiorespiratory arrest, acute myocardial infarction, respiratory failure, pulmonary embolism, pneumonia, and stroke. Similarly, another investigator [4] reported major complications of 3.5% (2 out of 56 patients) in patients 70 or older undergoing spinal surgery with RA. Older patients are more susceptible to hypoxemic episodes during recovery. Patients who undergo RA are associated with a lower risk for hypoxemia than GA [36].
Many surgeons wonder about using RA in a procedure lasting more than 2 hours [5], but a recent study demonstrated surgical time exceeding 3 hours in 5 of their cases, illustrating the possibility of longer periods of surgery than previously thought [4]. A more recent article suggested that it is feasible to use SA in lumbar spinal tumors in elderly patients with the ASA physical status classification grade III or IV scores who are at high risk of GA [44]. These studies substantiate the possibility of widening the spectrum of using RA in lumbar spine surgery.
A decline in cognition in elderly patients is associated with postoperative delirium [56]. In a randomized controlled study, reduced depth of anesthesia decreased the incidence of postoperative delirium [11]. It is possible to reduce cognitive decline in elderly patients by decreasing the incidence of postoperative delirium using RA instead of GA.
However, there are extra precautions regarding RA in elderly patients. Advanced age is associated with increased block height. In elderly patients, CSF volume decreases, and specific gravity increases. CSF volume is an important factor contributing to the spread of SA and is negatively correlated [18]. Nerve roots are more sensitive to local anesthetics in the geriatric population.
There have been numerous attempts to apply RA in various fields of spinal surgery, especially in minimally invasive surgeries [46,47,49]. Researchers showed a possibility of using RA including, but not limited to, a revision spinal fusion [49], robotic minimally invasive fusion [47], and spinal tumors [44]. Also, a randomized controlled study depicted the successful use of continuous EA in lumbar endoscopic surgery, which can be used without time limit, unlike other methods of RA, and as a postoperative epidural analgesia [46]. In terms of outcome, a recent large-scale study using a national registry showed the type of anesthesia does not affect the outcomes of lumbar decompressions or lumbar fusion [57].
In the institution of the senior authors, SA is used as a standard procedure in elective, noninstrumented lumbar spine surgery. Previous spine surgeries as well as antiplatelet therapy are not regarded as a contraindication. A retrospective evaluation of 473 cases showed that per case 19 minutes of anesthesia time could be saved using SA without increasing the risk of complications [7].
CONCLUSION
In short, the neuraxis anesthesia technique for lumbar spine surgery is gaining acceptance and is a viable option, especially in the geriatric population. It offers advantages over GA but some concerns must be taken into consideration. Nevertheless, concerns can be avoided with caution and mostly theoretical. When deciding which anesthetic method to use, the surgeon must consider the benefits and the risks. The surgeon should bear in mind that the general outcome of spinal surgery using RA has no significant difference with optimal selection of patient and surgery. Hence optimal planning between the surgeon and the patient is crucial. Although not all patients and procedures are adequate to use RA, there is no concrete evidence to be hesitant about using RA. Further work should concentrate on enhancing the quality of RA use by reducing anticipated complications and broadening the spectrum of its clinical use.
Notes
The authors have nothing to disclose.