Pearls and Pitfalls of Oblique Lateral Interbody Fusion: A Comprehensive Narrative Review
Article information
Abstract
Lumbar degenerative disease is a common problem in an aging society. Oblique lateral interbody fusion (OLIF) is a minimally invasive surgical (MIS) technique that utilizes a retroperitoneal antepsoas corridor to treat lumbar degenerative disease. OLIF has theoretical advantages over other lumbar fusion techniques, such as a lower risk of lumbar plexus injury than direct lateral interbody fusion (DLIF). Previous studies have reported favorable clinical and radiological outcomes of OLIF in various lumbar degenerative diseases. The use of OLIF is increasing, and evidence on OLIF is growing in the literature. The indications for OLIF are also expanding with the help of recent technical developments, including stereotactic navigation systems and robotics. In this review, we present current evidence on OLIF for the treatment of lumbar degenerative disease, focusing on the expansion of surgical indications and recent advancements in the OLIF procedure.
INTRODUCTION
Lumbar degenerative disease is a common age-related condition that causes pain and disability. A recent study reported an overall prevalence of degenerative spinal disease of 27.3%, which increased with age [1]. In this aging society, the rate of lumbar surgery has also steadily increased over time, with a clear benefit of reducing pain and improving quality of life in patients with lumbar degenerative disease [2,3]. Among various surgical procedures, lumbar interbody fusion is a widely accepted and effective technique for the treatment of lumbar degenerative disease and has been more utilized than other fusion techniques, such as instrumented posterolateral fusion, recently [4,5].
Individual techniques of lumbar interbody fusion differ in the surgical approach to the intervertebral disc (IVD) space; these techniques include posterior lumbar interbody fusion (PLIF), transforaminal lumbar interbody fusion (TLIF), anterior interbody fusion (ALIF), direct lateral interbody fusion (DLIF), and oblique lateral interbody fusion (OLIF) (Fig. 1). In the treatment of spinal stenosis, ALIF, DLIF, and OLIF can be categorized as indirect decompression techniques. Indirect decompression improves spinal stenosis through disc height restoration, spondylolisthesis reduction, segmental stabilization, and gradual remodeling of the spinal canal (Fig. 2), instead of directly removing compressive lesions. Previous studies have demonstrated radiological evidence of indirect decompression in these lumbar interbody fusion techniques [6-8].
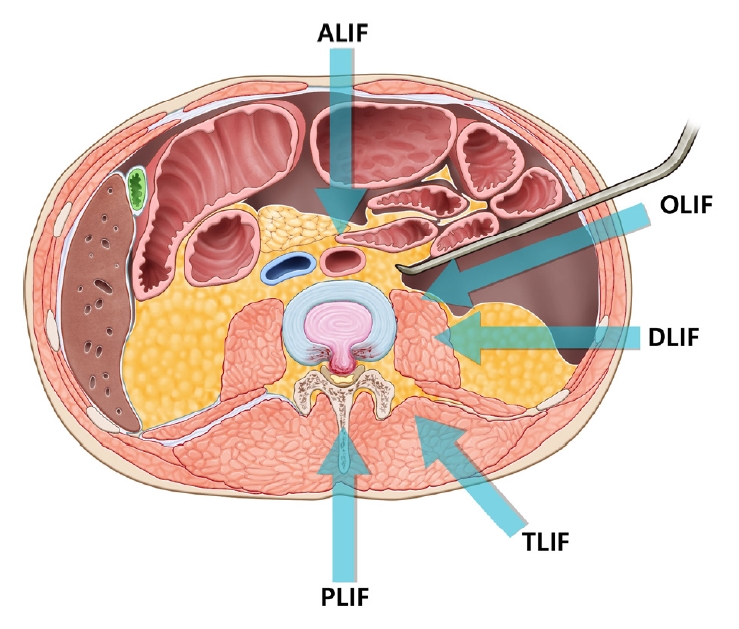
Lumbar interbody fusion techniques. ALIF, anterior interbody fusion; OLIF, oblique lateral interbody fusion; DLIF, direct lateral interbody fusion; TLIF, transforaminal lumbar interbody fusion; PLIF, posterior lumbar interbody fusion.
Gradual remodeling of the spinal canal following oblique lateral interbody fusion (OLIF). (A) Preoperatively, a T2-weighted axial magnetic resonance image (MRI) at L4–5 shows severe spinal stenosis. (B) At postoperative 1-week following OLIF, there is no significant change in the spinal canal area. (C) However, a postoperative 1-year MRI shows a significantly widened spinal canal due to the stabilization effect of OLIF.
The term OLIF was first used by Silvestre in 2012 following the description of a minimally invasive anterior retroperitoneal approach by Mayer in 1997 [9,10]. Because OLIF utilizes a retroperitoneal antepsoas approach involving a corridor between the psoas major muscle and great vessels, it has the theoretical advantages of lower rates of bowel injury than transperitoneal ALIF, as well as lower risk of lumbar plexus injury than transpsoas DLIF. Many authors have reported early favorable clinical outcomes with relatively few complications in their studies [11]. More recently, the use of OLIF in the treatment of lumbar degenerative disease has increased, and the indications for OLIF have expanded with recent advancements, such as stereotactic navigation and robotics.
This review will cover the evolution and application of OLIF in the treatment of lumbar degenerative disease, with a particular emphasis on the expansion of surgical indications and recent advancements in the OLIF procedure. We reviewed PubMed, Web of Science, and Embase databases for human clinical studies restricted to the English language from inception to November 2021. We used search terms including “OLIF,” “oblique lumbar interbody fusion,” and “ante-psoas.” An additional search was performed to identify studies on stereotactic navigation, robotics, and single-position surgery that covered OLIF. We also manually searched for additional relevant studies from the references of the key publications. We did not exclude studies with short follow-up periods or small sample sizes because the OLIF procedure is an ever-evolving surgical technique, and the objective of this review was to summarize the recent evidence available in the literature.
SURGICAL TECHNIQUES AND CONSIDERATIONS
1. Surgical Corridor and Patient Positioning
OLIF utilizes a retroperitoneal oblique corridor and a surgical window between the psoas major muscle and great vessels for L2–5 and between the bifurcated iliac vessels for L5–S1. Numerous anatomical and radiological studies have investigated the feasibility of this oblique corridor [12-14]. Molinares et al. [12] reviewed 133 magnetic resonance imaging (MRI) images and reported that a safe oblique corridor was identified in 90% of cases for L2–5 and 69% for L5–1. The oblique corridor of L4–5 requires additional consideration because it is often unavailable due to obstruction of vascular structures or a high riding psoas [15]. Although the operative corridor can be increased in the lateral decubitus position at the L4–5 level, surgeons should always consider these anatomical structures in preoperative planning and optimize the surgical incision to secure a safe oblique corridor.
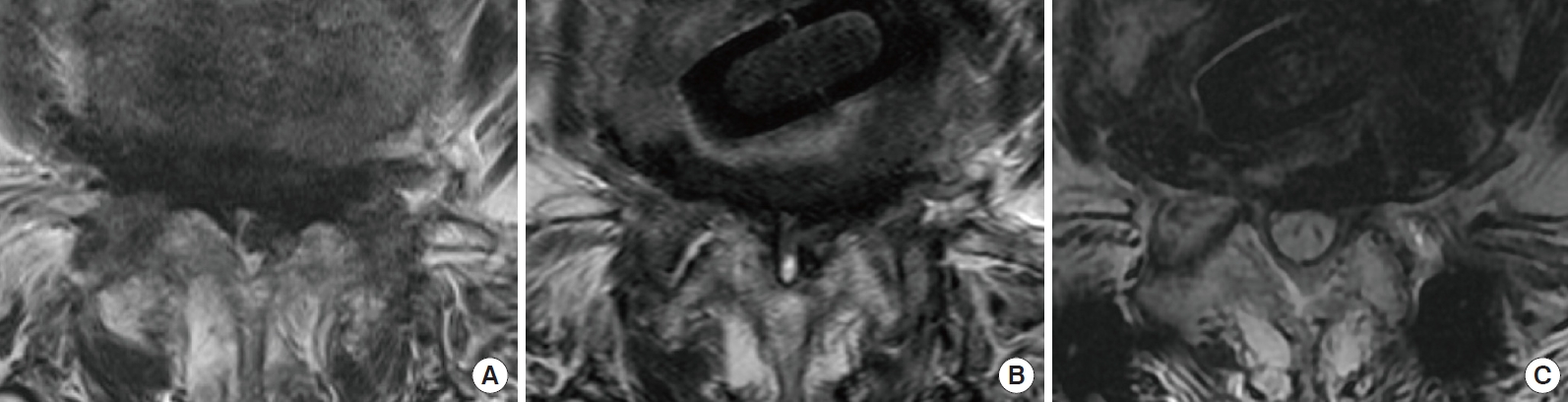
The surgical approach using an oblique corridor to the lumbosacral junction is less feasible than L2–5 due to the major abdominal vessels that overlie the L5–S1 IVD [16]. The right lateral decubitus position for OLIF at L5–S1 can further decrease the bare window for L5–S1 IVD access due to downward migration of the left common iliac vein (LCIV) [17]. Careful assessment of these vascular structures should be performed using preoperative axial and sagittal MRI images. Abdominal computed tomographic (CT) angiography or the novel MRI–CT fusion technique can also be utilized [14,16]. Three factors should be considered when determining the feasibility of L5–S1 anterior access: (1) the size of the vascular corridor, (2) the location of the LCIV, and (3) the presence of a fat plane between the LCIV and IVD [18,19]. In cases where the vascular corridor is narrow, with the LCIV crossing the midline, and no fat plane visible between the LCIV and IVD, one should consider a surgical approach other than OLIF due to the high risk of vascular injury (Fig. 3) [16,18]. Additionally, OLIF at the L5–S1 level is not possible in cases where the angle of the L5–S1 IVD in the sagittal plane goes under the symphysis pubis [16].

The types of vascular corridors oblique lateral interbody fusion (OLIF) at L5–S1. (A) A wide vascular corridor with no structures obstructing the L5–S1 intervertebral disc (IVD) access. (B) A difficult type of vascular corridor due to the left common iliac vein covering the left half of L5–S1 IVD with no fat plane between the vessel and IVD. (C) Another difficult type of vascular corridor with no accessible window for the whole length of L5–S1 IVD.
Early investigators introduced OLIF as a surgical procedure performed in the lateral decubitus position [9,10]. However, positioning patients in the true lateral decubitus position is becoming less crucial because of the development and application of stereotactic navigation systems in OLIF [20]. The evolution of OLIF due to recent technological advancements is further discussed in the later part of this review. Optimal hip positioning in the lateral decubitus position is an issue that has been investigated in previous studies [21,22]. Although controversy exists on whether the hip position is associated with widening of the surgical corridor, neutral hip positioning is generally recommended to reduce the psoas volume during OLIF [21,22].
2. Additional Fixation and Decompression
Although few studies advocate the stand-alone OLIF procedure as a safe and effective option for lumbar degenerative diseases [23,24], multiple biomechanical studies have shown that additional stabilization is beneficial for the stability of the OLIF construct [25,26]. In these studies, stand-alone OLIF without additional fixation could not provide sufficient stability to avoid cage subsidence. Among the various available fixation methods, bilateral pedicle screws and rod fixation provided the best biomechanical stability in previous finite element analysis studies [27,28]. With regard to fixation methods other than pedicle screws, lateral plate fixation showed no additional clinical benefit to stand-alone OLIF in preventing cage subsidence [29]. Anterolateral screws and rod fixation added to OLIF showed favorable early clinical outcomes, with a cage subsidence rate of 7.7% [30]. However, because these are retrospective studies with small sample sizes, we cannot currently make any recommendations on lateral plates or anterolateral screws based on their results.
Supplemental screw fixation can be performed to prevent anterior cage migration following OLIF at the L5–S1 level. Supplemental screw fixation at the anterior aspect of L5–S1 was initially introduced in stand-alone ALIF with favorable radiological outcomes [31,32]. Chung et al. [33] retrospectively reviewed 61 patients who underwent OLIF and pedicle screw fixation at the L5–S1 level and found that anterior cage migration was significantly reduced in cases where supplemental screw fixation was performed. However, in this case, the role of the supplemental screw was to prevent anterior cage migration rather than provide additional segmental stability and prevent cage subsidence. The cost-effectiveness of supplemental screw fixation in L5-S1 OLIF should also be verified in future studies.
Additional posterior direct decompression can be performed in conjunction with indirect decompression, particularly in cases with severe stenosis or a sequestered disc [34,35]. In a recent systemic review, Manzur et al. [36] compared clinical outcomes between isolated indirect decompression and combined indirect and direct decompression. In this study, the isolated indirect decompression group tended to have a more significant improvement in the Oswestry Disability Index (ODI; 21.3% vs. 17.1%, p=0.053). Other clinical outcomes, including overall complication and revision rates, showed no statistically significant differences between the 2 groups. However, the analysis failed to identify cases where additional posterior direct decompression was beneficial and warranted due to the limited quantity and quality of the included studies. Future studies comparing the 2 surgical methods (isolated indirect decompression versus combined indirect and direct decompression) should be conducted.
EXPANDING INDICATIONS FOR OLIF
1. Severe Spinal Stenosis
Degenerative disc disease, spinal stenosis, and spondylolisthesis (degenerative and spondylolytic) are common indications for OLIF, and previous studies have reported favorable outcomes following OLIF in these conditions [37,38]. However, there is skepticism among spine surgeons on whether severe lumbar spinal stenosis can be effectively treated by indirect decompression alone [39]. However, recent studies have reported favorable radiological and clinical outcomes following indirect compression even in severe spinal stenosis [40,41]. In a recent study by Shimizu et al. [42], the authors compared the radiographic and clinical outcomes between indirect (OLIF) and direct (TLIF, PLIF) decompression in patients with severe spinal stenosis (Schizas classification C or D). Although the 2 groups showed comparable 1-year clinical outcomes, the surgical (estimated blood loss and operative time) and radiographic outcomes (disc height restoration and fusion rate) were better in the OLIF group. These results may allow the expansion of indications for isolated indirect decompression, regardless of the degree of spinal stenosis. However, Shimizu et al. did not include patients with extraligamentous disc herniation, locked facets, or bony stenosis in the OLIF group. As many surgeons still regard these conditions as relative contraindications for indirect decompression, more studies are required to clarify the indications and contraindications for OLIF.
2. Lumbar Facet Cyst
Lumbar facet cyst (LFC), an indicator of segmental instability, is commonly found in degenerative spondylolisthesis [43]. Controversy exists regarding whether indirect decompression using OLIF can successfully treat LFC [44]. In a recent prospective study by Chang et al. [45], the authors observed that 75% of LFCs were reduced immediately following OLIF, while all LFCs were resolved in the postoperative 1-year MRI. In this study, patients with immediate reduction of LFC had more significant segmental instability in the preoperative dynamic x-ray than their counterparts. Based on these results, OLIF for LFC may produce more predictable outcomes in patients with segmental instability (Fig. 4).
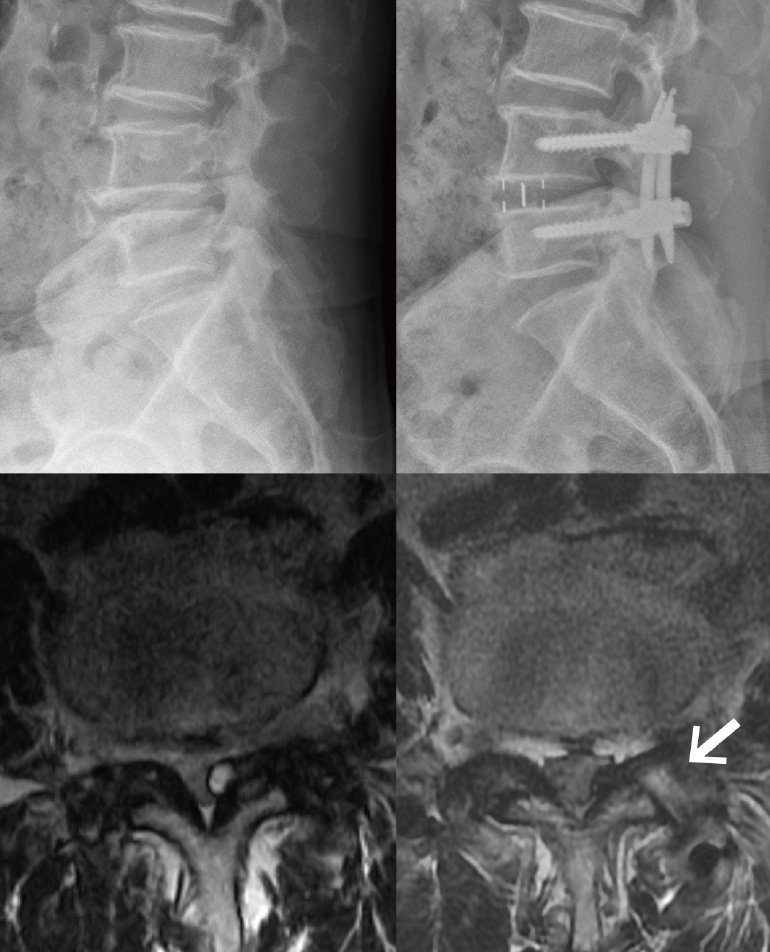
Oblique lateral interbody fusion (OLIF) for the treatment of lumbar facet cyst (LFC) associated with degenerative spondylolisthesis. An LFC arising from the left facet joint at L4–5 is causing subarticular stenosis preoperatively. Immediately following OLIF, the facet joint space has been widened (white arrow), and LFC is reduced.
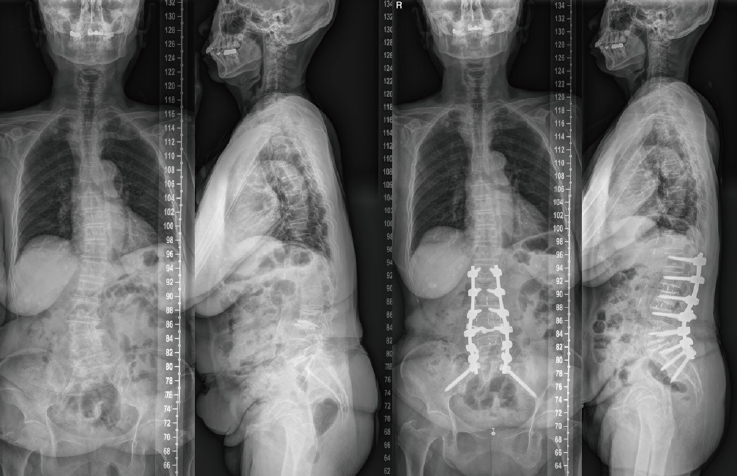
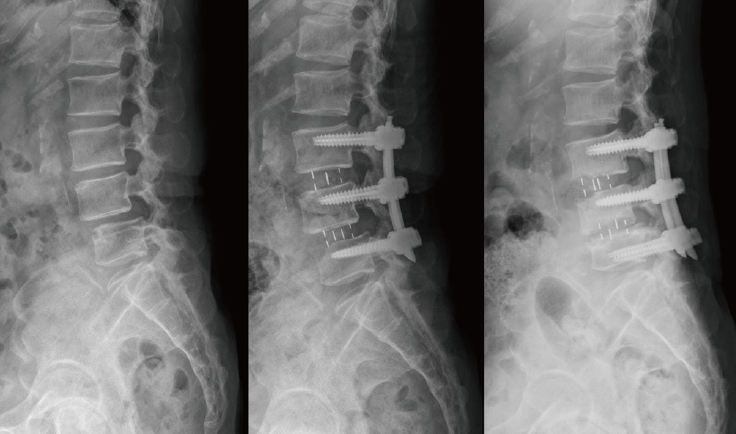
3. Adult Spinal Deformity
OLIF has gained popularity in the correction of adult spinal deformity (ASD) (Fig. 5) [46]. Numerous studies have identified OLIF as a safe and effective surgical option for treating ASD, with less intraoperative blood loss and lower complication rates than other techniques [47-49]. A recent meta-analysis showed that OLIF could successfully correct sagittal and coronal deformities with or without posterior column osteotomies (PCOs) [50]. Moreover, in severe sagittal malalignment, OLIF can be utilized in anterior column realignment (ACR) by adding circumferential annulotomy and anterior longitudinal ligament resection to conventional OLIF [51]. ACR can also be performed in conjunction with PCO depending on the severity of the deformity [52]. However, discussing the optimal indications for individual deformity correction techniques is beyond the scope of this review.
4. Infections
Several authors have reported clinical and radiological outcomes of lumbar interbody fusion using an antepsoas approach in pyogenic, fungal, and tuberculous infections of the lumbar spine [53,54]. The theoretical advantages of the antepsoas approach in the spinal infection treatment are as follows: (1) direct visualization and access to infectious tissue in the anterior column, allowing thorough debridement and stable anterior column reconstruction; (2) reduction of surgical morbidity when performed in a minimally invasive surgical (MIS) technique; and (3) avoidance of posterior spinal musculature violation during the posterior approach [55]. For these reasons, antepsoas lumbar interbody fusion combined with percutaneous pedicle screw fixation has shown superior clinical results, including infection control and complication rates, compared to other surgical techniques in previous studies [56].
However, surgeons should be more cautious when performing this technique for infections that occur at the L5–S1 level. The involvement of the L5–S1 level has been identified as an independent risk factor for unfavorable outcomes following surgical treatment for lumbar pyogenic spondylitis due to difficult surgical access to the lumbosacral junction [55]. Transperitoneal ALIF with dissection of the major vessels by a vascular surgeon may be preferred over minimally invasive antepsoas lumbar interbody fusion when vascular adhesion to the L5–S1 IVD is suspected on preoperative MRI.
5. Revisional Surgeries
OLIF is also useful in cases where a revision surgery is required. Revisions using indirect decompression can avoid burdensome adhesiolysis and prevent incidental durotomy and nerve root injury, which may occur during revisional direct decompression. Shimizu et al. [57] reported successful clinical and radiological outcomes following indirect decompression using OLIF in patients with spinal stenosis who had failed prior direct decompression. In addition, OLIF can be utilized as a salvage operation in patients with pseudarthrosis from previous lumbar fusion surgery. Masuda et al. [58] advocated salvage OLIF for treating pseudarthrosis following PLIF or TLIF because it allows extensive curettage of intervertebral scar tissue, rigid anterior support, and reduction of complications associated with the manipulation of posterior scar tissue.
CLINICAL AND RADIOLOGICAL OUTCOMES OF OLIF
Recent meta-analyses and multicenter studies have compared the operative results (e.g., operation time and estimated blood loss), clinical scores (pain and disability), radiological outcomes (disc height restoration, sagittal alignment, fusion rate), and complications between OLIF and other minimally invasive lumbar interbody fusion techniques.
1. OLIF Versus DLIF
The most significant advantage of OLIF over DLIF is relative preservation of the psoas major muscle and lower risk of lumbar plexus injury during an antepsoas approach. In a meta-analysis by Li et al. [59], the authors compared clinical and radiological outcomes between antepsoas OLIF and transpsoas DLIF for lumbar degenerative disease, based on the results from 56 studies. In their analysis, the improvement of visual analogue scale (VAS) and ODI scores was more significant in the OLIF group. The authors suspected that complications associated with psoas muscle injury in DLIF may have contributed to this difference. Other previous studies have also reported significantly higher rates of anterior thigh symptoms (pain, sensory deficit, and hip flexor weakness) in DLIF (30%–40%) than OLIF (1.3%–21.4%) [38,60-62]. However, these symptoms are generally transient and resolve at postoperative 3 to 6 months [63].
The estimated blood loss, operative time, and length of hospital stay did not differ significantly between the 2 groups in the meta-analysis by Li et al. [59]. However, another meta-analysis by Walker et al. [64] showed that the operation time was significantly shorter for the antepsoas approach than for the transpsoas approach (120.5 minutes vs. 203.6 minutes, p<0.001). A relatively higher number of surgical levels and use of intraoperative neuromonitoring in the transpsoas approach group included in this study may have contributed to the longer operation time. Although the 2 groups showed similar overall complication rates (26.7% for OLIF and 27.8% for DLIF), the types and incidences of the main complications differed significantly. As anticipated, anterior thigh symptoms (pain, numbness, transient, and permanent weakness) were more common in DLIF, while sympathetic plexus and vascular injuries were more frequent in OLIF [59,64].
Radiologically, the 2 groups showed similar disc height restoration in the meta-analysis by Li et al. [59]. As for the fusion rate, successful fusion was achieved in 96.9% of cases (278 of 287) for OLIF in 5 studies, while the fusion rate was 91.6% (535 of 584) for DLIF in 12 studies [59]. In addition, a meta-analysis by Souslian and Patel [65] reported that OLIF demonstrated a trend of higher fusion rates compared to other indirect decompressions. However, these studies could not provide an explanation for the clinical significance of a higher fusion rate for OLIF than for other lumbar interbody fusion techniques.
2. OLIF Versus TLIF
Multiple studies have compared OLIF (indirect decompression) to MIS-TLIF (direct decompression) in terms of clinical and radiological outcomes [66-70]. In a recent meta-analysis by Zhang et al. [68], the improvement in VAS score for radiating pain was more significant in the OLIF group, while the changes in VAS score for back pain and the ODI scores were equivalent. Koike et al. [66] retrospectively reviewed 86 patients who underwent OLIF or MIS-TLIF with cortical bone trajectory screw fixation in both groups. The authors found that the improvement in the psychological domain in the Japanese Orthopedic Association Back Pain Evaluation Questionnaire (JOABPEQ) was more significant in patients who underwent OLIF. However, Takaoka et al. [67] reported that there were no significant differences in clinical scores, including VAS and JOABPEQ scores, between the 2 surgical methods in their retrospective multicenter study.
In the meta-analysis by Zhang et al. [68], OLIF showed a shorter duration of surgery and less intraoperative blood loss than MIS-TLIF, even with supplementary posterior fixations. In the same study, pooled analyses identified no significant differences in the overall complication rate and complication types [68]. Other comparative studies also reported similar complication rates between the surgical methods [66,67,69].
Radiologically, in multiple studies, OLIF has shown a clear advantage over MIS-TLIF in disc height restoration, especially in the anterior portion of IVD [66-68]. Segmental lordosis creation was also superior in OLIF than in MIS-TLIF [68], particularly at the L5–S1 level [69]. This result is expected because the only mechanism for creating segmental lordosis in MIS-TLIF is compression of the posterior spinal column. However, a pooled analysis found no significant difference in total lumbar lordosis restoration between the 2 procedures [68]. This insignificance may have resulted from the fact that most studies investigated single-level surgeries.
The fusion rate at the last follow-up tended to be higher in OLIF, albeit without statistical significance [65,68]. In addition, Lin et al. [70] reported an earlier fusion time for OLIF than MIS-TLIF in their retrospective comparative study. However, unlike TLIF, no local autologous bone graft is available in the standard OLIF procedure. Therefore, utilizing bone graft substitutes, such as demineralized bone matrix and bone morphogenetic protein, is essential in OLIF. Cage subsidence measured by the loss of disc height was also significantly less in OLIF in a pooled analysis of 3 studies [68]. The following factors may have contributed to these favorable outcomes in OLIF: (1) a wider window for discectomy and endplate preparation, (2) a significantly larger contact surface between the interbody cage and endplates, and (3) a longer interbody cage, which can touch both sides of the apophyseal ring [71,72].
3. OLIF Versus ALIF
OLIF at L5–S1 using a retroperitoneal approach in the lateral decubitus position can be compared to transperitoneal ALIF performed in the supine position. OLIF is a safe and effective option for L5–S1 access and fusion, with comparable outcomes and complications to ALIF [73,74]. However, there are discrepancies regarding which procedure is more beneficial in restoring disc height and segmental lordosis. Chung et al. [74] reported more significant disc height and segmental lordosis restoration in OLIF, whereas Xi et al. [73] found that ALIF provided a greater disc height increase but similar postoperative segmental lordosis. We cannot derive any definite conclusion at this time from these retrospective studies with small sample sizes.
COMPLICATIONS REQUIRING SPECIAL CONSIDERATIONS
Various intraoperative and postoperative complications can occur following OLIF. Although OLIF using the antepsoas approach is presented as a relatively safe procedure in these studies, several complications require special considerations and will be discussed here.
1. Vascular Injury
Among many studies that have reported complications of OLIF, the retrospective cohort study by Tannoury et al. [62] is the largest, including 940 patients and 2,429 fusion levels. Interestingly, the overall surgical complication rate in this study was 8.2%, with no cases of major vascular injury. A similar study by Mehren et al. [11], which reviewed 812 patients during a 12-year period, reported only 3 cases (0.37%) of major vascular complications (2 common iliac vein injuries and 1 aortic injury). In our clinical experience of 752 OLIF cases during a 10-year span, major vascular injuries occurred in only 3 cases (0.39%). All cases were LCIV injuries, 1 at L4–5 and 2 at L5–1, which were surgically repaired successfully by a vascular surgeon. Although major vascular injuries are rare during OLIF, careful preoperative planning by considering the vascular anatomy in the surgical corridor as previously described is crucial to avoid this catastrophic event.
Segmental arteries (SAs) can also be injured and cause profuse bleeding during OLIF, especially when inserting pins for retractor fixation. SA injury occurred at a rate of 0.3% to 2.6% in previous studies [61,62]. Several authors have used imaging studies to evaluate the regional anatomy of the SAs and stratify the risk of SA injury. After reviewing 272 lumbar MRIs, Orita et al. [75] found that L5 SA was close to or overlying the L4–5 IVD in 4.1% of cases, increasing the risk of injury during OLIF. Wu et al. [76] reviewed the CT angiography images of 50 patients and found that the risk of SA injury was high when the interbody cage was placed in the posterior one-fourth of the IVD at L3–5. They also suggested that the retractor pins should be placed on the upper edge of L2 and L3 in L1–2 and L2–3 OLIF, respectively. For L3–4 and L4–5 OLIF, the pins were fixed at the lower edge of L3 and L4 to prevent SA injury. These observations are helpful for surgeons to avoid SA injuries during OLIF procedures.
2. Ureter Injury
Ureteral injury is a rare complication following OLIF, only described in several case reports [77,78]. Most surgeons have reported no case of ureteral injury in their large case series [38,62,79]. The ureter, attached to the posterior wall of the peritoneum, is commonly encountered during a retroperitoneal antepsoas approach. However, it can be easily mobilized and swept anteriorly with the peritoneum, especially when the peritoneum is directly visualized for mobilization. Because several authors have reported ureteral injuries when placing the retractors or lateral plates blindly, surgeons should avoid conducting these procedures through retroperitoneal fat in a blind fashion [61,80]. Ureteral injuries can be clinically suspected in cases of unexplained abdominal pain or distention following OLIF. Delayed contrast CT or retrograde urography can be utilized for diagnosis, and ureteroureterostomy and ureteral stenting can be performed as a treatment [81].
3. Postoperative Ileus
Postoperative ileus (POI) is a relatively common complication that can adversely affect clinical outcomes following lumbar fusion surgery, with a rate of 0.6% to 22.0% [82]. The POI rate from previous studies on OLIF ranged from 0.9% to 3.9% [11,62,79,83]. A recent study by Park et al. [83] analyzed 460 patients who underwent OLIF and percutaneous pedicle screw instrumentation and identified inadvertent endplate fracture as an independent risk factor for POI following OLIF. Suggested explanations for the association between POI and endplate fracture are as follows: (1) endplate fracture inducing the release of inflammatory mediators, leading to abnormal intestinal motility; and (2) nociceptive stimulus caused by endplate fracture stimulating inhibitory neural reflexes, leading to postoperative hypomotility [83]. Avoiding endplate violation during OLIF is also important in preventing POI.
4. Cage Subsidence
Delayed subsidence of the interbody cage is a common complication following OLIF [38,81]. The incidence of cage subsidence has been reported to be up to 18.7% when combined with intraoperative endplate violations [61]. However, rates may significantly vary among studies depending on the definition of cage subsidence and measurement methods. During OLIF, cage subsidence must be minimized because it has been associated with poor radiological and clinical outcomes (Fig. 6). Cage subsidence can lead to insufficient indirection decompression (reduction of the disc and foraminal height) and loss of segmental lordosis radiologically, and recurrence of radiculopathy clinically [6]. However, some previous studies have reported no significant difference in leg pain VAS between patients with or without cage subsidence following indirect decompressions (both OLIF and DLIF) [84-86]. In addition, there are conflicting results on whether cage subsidence increases the risk of pseudarthrosis and revision surgery [87-89]. Therefore, more future studies are required to verify the clinical significance of cage subsidence following indirect decompression.
A case of delayed cage subsidence following oblique lateral interbody fusion (OLIF). (A) A 68-year-old female with chronic kidney disease on hemodialysis underwent OLIF at L3-4-5. (B) There were no endplate violations in the immediate postoperative radiograph. (C) Six months postoperatively, significant subsidence of interbody cages occurred.
Preoperative imaging studies can help surgeons to stratify the risk of endplate violation and cage subsidence in OLIF procedures. The Hounsfield unit can be measured in preoperative CT images to evaluate the strength of the endplates. In a previous study, a low Hounsfield unit at the ipsilateral epiphyseal ring was identified as an independent risk factor for endplate violation and cage subsidence following OLIF [90]. Endplate morphology was also associated with cage subsidence; flat endplates are relatively resistant to cage subsidence, while concave endplates are prone to cage subsidence [84].
Aggressive shaving of endplates and overdistraction by using too large or tall interbody cages are associated with the above complications. Therefore, careful distraction of the disc space using serial implant trials and avoiding excessive endplate preparation is crucial for preventing endplate violation and cage subsidence during OLIF [61]. It is also preferrable to perform additional stabilization, including pedicle screw instrumentation, because stand-alone OLIF cannot provide sufficient stability to avoid cage subsidence in biomechanical studies [25,26].
5. Adjacent Segment Degeneration and Disease
Radiological adjacent segment degeneration (ASDeg) and symptomatic adjacent segment disease (ASDis) are common long-term adverse events following lumbar fusion surgeries [91]. Indirect decompression has the potential to reduce ASDeg and ASDis because it has advantages over direct decompression in the preservation of posterior spinal elements and restoration of sagittal alignment. A recent meta-analysis compared indirect and direct decompression and reported that patients who underwent indirect decompression had 0.34-fold lower odds of developing ASDeg and 0.40-fold lower odds of reoperation due to ASDeg than those who underwent direct decompression [92]. The pooled mean differences for the segmental and total lumbar lordosis angles were more significant in indirect decompression in this meta-analysis. However, the authors mentioned that the quantity and quality of the included studies were limited. Therefore, the long-term effect of indirect decompression on ASDeg and ASDis should be determined in future studies.
RECENT ADVANCEMENTS
The use of intraoperative stereotactic navigation systems and robotic assistance in OLIF has increased recently [20], as has the evidence on these technical advancements, which can improve surgical accuracy and patient outcomes. Xi et al. [93] published the results of 214 navigated OLIF cases and reported a cage placement accuracy rate of 94.86%. Only one patient underwent a revisional operation due to cage misplacement, and there was no vascular injury in their series. Navigation assistance in OLIF is considered a safe and effective alternative to fluoroscopy, which can improve surgical accuracy and reduce radiation exposure to surgeons and surgical staff [94].
Navigated OLIF can be performed in a single lateral decubitus position without changing to the prone position for posterior instrumentation. From a technical standpoint, the navigation system does not require the true lateral position of the patient, and the side tilting of the table can be adjusted for each surgical step (Fig. 7). In addition, OLIF and posterior instrumentation can be performed simultaneously by dual attending surgeons. The results of single-position surgery in the literature are promising because it has a significantly shorter operation time and less blood loss than dual-position surgery (lateral decubitus, then prone) [95]. The accuracy of pedicle screws, segmental lordosis restoration, and clinical outcomes were also comparable to other surgical methods, such as dual-position lateral interbody fusion surgery or PLIF [95,96].
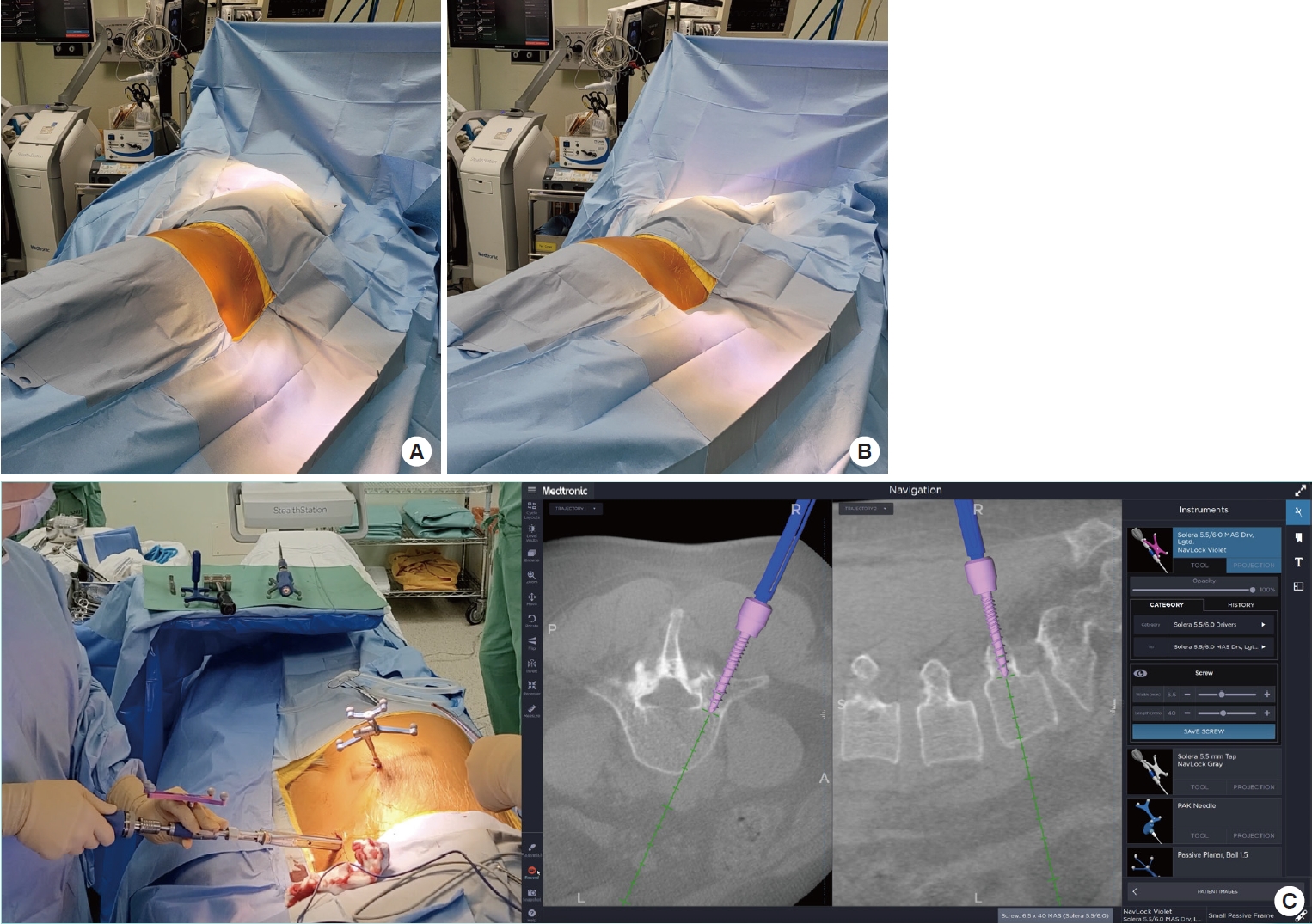
Patient positioning in single position navigated oblique lateral interbody fusion (OLIF). (A) For the anterior surgery, the patient is positioned close to lateral decubitus. (B) The patient can be tilted forward to a semiprone position for posterior surgery to allow more space for posterior instrumentation, especially for the downside screws. (C) In this position, downside screws can be inserted without difficulty.
Navigated OLIF can also be performed with robotic assistance for posterior pedicle screw instrumentation [97]. More recently, the application of robotic and navigation-assisted OLIF in a single position has been expanded to the lumbosacral junction: OLIF at L5–S1 and posterior sacropelvic fixation [98,99]. Because this is a still-evolving technique, future studies investigating the long-term outcomes and cost-effectiveness of these technical advancements should follow.
CONCLUSIONS
OLIF is a safe and effective surgical option for treating various lumbar degenerative diseases, with comparable radiological and clinical outcomes to other minimally invasive lumbar fusion techniques. The indications for OLIF are expanding with the application of recent technical advancements, including stereotactic navigation systems and robotics. Although serious complications are rare, careful preoperative planning is required to reduce complications and improve surgical outcomes. Future studies should investigate the long-term outcomes of OLIF.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: HK, BC, SYC; Formal analysis: BC, SYC; Methodology: HK, BC, SYC; Project administration: BC; Visualization: SYC; Writing - original draft: HK, BC, SYC; Writing - review & editing: HK, BC, SYC.