Prevalence and Clinical Impact of Cervical Facet Joint Degeneration on Degenerative Cervical Myelopathy: A Novel Computed Tomography Classification Study
Article information
Abstract
Objective
To evaluate cervical facet joint degeneration using a newly developed classification, investigate its prevalence and relationship with cervical degenerative spondylolisthesis, and clarify its clinical significance in patients with degenerative cervical myelopathy (DCM).
Methods
This study included 145 consecutive patients with DCM who underwent surgical treatment. Clinical variables and radiological findings were analyzed. A new 6-grade computed tomography (CT) classification for cervical facet joint degeneration was adapted, and its prevalence was evaluated by categorizing the joints into those at responsible and those at nonresponsible spinal segmental levels. We evaluated the association between rapidly progressive myelopathy and the presence of significant facet joint degeneration or spondylolisthesis at the responsible segmental level.
Results
Finally, 140 patients with a mean age of 64.1 ± 12.8 years were analyzed. The prevalence of grade 1, 2, 3, 4, 5A, and 5B classification in all facet joints was 72.0%, 9.5%, 10.9%, 4.3%, 2.9%, and 0.4%, respectively. There was a statistically significant difference in the distribution of CT grades between the joints at the responsible and nonresponsible segmental levels (p < 0.001), with a high prevalence of grade 4 or 5B degeneration at the responsible segmental level, reflecting articular irregularity. There was also a statistically significant relationship between rapidly progressive myelopathy and grade 4 or 5B degeneration at the responsible segmental level (p < 0.001), but not between rapidly progressive myelopathy and spondylolisthesis (p = 0.255).
Conclusion
This novel CT classification for facet joints deserves additional evaluation in patients with DCM. Abnormal findings on the articular surfaces might be related to the progression of myelopathy.
INTRODUCTION
Degenerative cervical myelopathy (DCM), including cervical spondylotic myelopathy, is a common age-related spinal disorder. DCM is mostly asymptomatic, but sometimes it becomes a symptomatic background pathology and reduces quality of life due to impairment of motor function [1]. It comprises osteoarthritic changes to the spine, which include facet arthropathy, spondylosis, disc herniation, ligamentous hypertrophy, calcification, and ossification [2]. These degenerations do not occur in only one type, but often results from a combination of multiple degenerations, resulting in myelopathy. The degree of degeneration varies in each case, and many cases cannot be clearly subdivided in daily clinical practice.
The cervical facet joint is a synovial joint located in the posterolateral spine. Degenerative facet joint pathology is associated with cervical degenerative spondylolisthesis, which can induce myelopathy [3]. However, the evaluation of cervical facet joints has not received much attention in daily clinical practice, partly because it is difficult to evaluate them without computed tomography (CT) and partly because of the diagnostic superiority of magnetic resonance imaging in spinal and spinal cord diseases. For facet joint degeneration of the lumbar spine, several CT classifications have been reported for degenerative spondylolisthesis. CT evaluation of cervical facet joints is less debated and fewer relevant reports [4,5], so it is not clinically significant.
We recently reported a case of DCM with unilateral severe facet joint degeneration at the responsible spinal segmental level and rapid neurological deterioration without any trauma or cervical spondylolisthesis [6]. Because the relationship between facet joint degeneration and DCM remains unknown, we conducted a retrospective study to identify the prevalence of facet joint degeneration using a newly developed CT classification reflecting articular irregularities in patients with DCM and discuss its impact on the clinical setting.
MATERIALS AND METHODS
All experiments were conducted following the guidelines of the Declaration of Helsinki. All research protocols were approved by the Institutional Review Board of Nara Medical University (approval number: 2241). The need for informed consent was waived.
1. Patient Selection
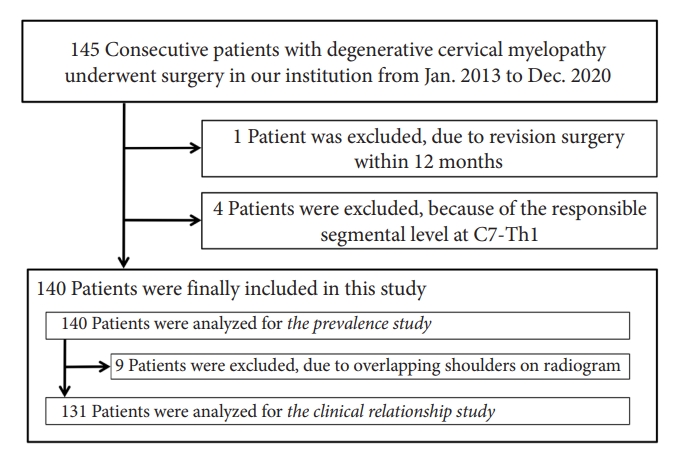
We retrospectively analyzed consecutive DCM patients who underwent surgical treatment at our institution between January 2013 and December 2020. Inclusion criteria included the responsible spinal segment being at the subaxial level between C2–3 and C6–7 and preoperative CT and radiography of the cervical spine. Patient who received revision surgery within 12 months was excluded. Clinical data, including responsible segmental level and radiological findings, were gathered retrospectively from medical records, preoperative neurologic examinations, and radiographic images. Regarding the clinical evaluation, the diagnosis of cervical myelopathy was made on the basis of symptoms first, but also on the magnetic resonance imaging (MRI) findings. The responsible segmental level was defined as the level of the lesion causing myelopathy and identified in each case based on the neurologic examinations first, and referring to the MRI findings if necessary. To study radiological classification as well as its clinical implications, the clinical course, especially concerning rapid progression of cervical myelopathy, was also investigated. Rapid progression of cervical myelopathy was defined in this study as in previous reports [7,8]. In brief, patients with rapid DCM progression had difficulty maintaining a standing posture or walking without support, which corresponded to Nurick grade 4 or 5, within 4 weeks of symptom onset due to rapidly progressive neurological deterioration. To assess the clinical impact of facet joint degeneration, the study population was divided into 2 cohorts: a rapid progression group and slow progression group, depending on whether or not they met the definition.
2. CT Assessment of Cervical Facet Joint Degeneration
Preoperative CT of the cervical spine was performed on admission in each patient. Results were retrospectively reviewed and assessed. We carefully evaluated all cervical facet joints from the C2–3 to C6–7 levels on the axial, sagittal, and coronal sections. In short, 10 facet joints for 5 intervertebral levels were evaluated separately for each case. We classified them into 6 grades according to the severity of the following degenerative findings: osteophyte formation, joint hypertrophy, joint space narrowing, cyst formation, articular irregularity, ankylosing changes, and facet joint opening with articular irregularity (Fig. 1). In this classification, the final stage of facet degeneration was defined as “grade 5.” There are 2 types of facet degeneration in the final stage: stabilization due to joint fusion and destabilization due to advanced joint destruction as in rheumatoid arthritis. Since there are incompatible and cannot be ordered, “grade 5” was subdivided into 2 categories, 5A and 5B. Assessments were conducted independently by 2 neurosurgeons; any differences in assessments were finalized through discussion. To evaluate the reproducibility of the CT classification, 2 different initial assessments by 2 independent neurosurgeons were examined for concordance.
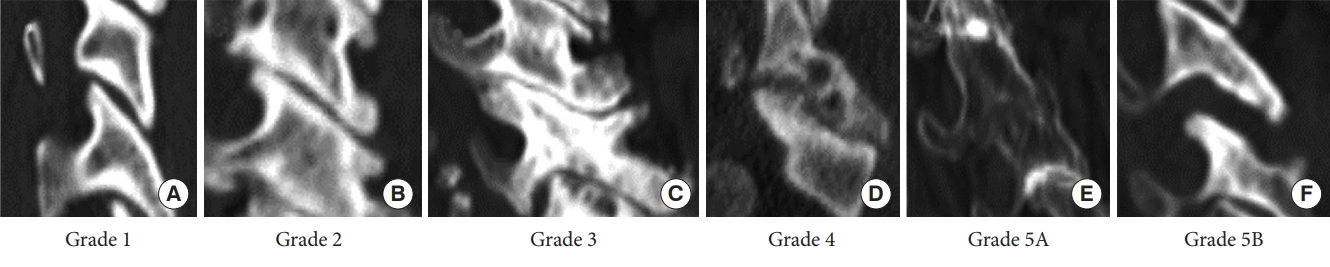
Newly developed computed tomography classification for cervical facet joint degeneration. (A) Grade 1, normal facet joint with no degenerative changes. (B) Grade 2, mild degenerative changes with only osteophyte formation. (C) Grade 3, degenerative changes with osteophyte formation including joint space narrowing, microcyst (< 2 mm), or joint hypertrophy. (D) Grade 4, severe degenerative changes, including moderate to large cysts (≥ 2 mm), and articular irregularity. (E) Grade 5A, ankylosing changes with bony fusion of the facet joint. (F) Grade 5B, facet opening with articular irregularity.
3. Radiographic Assessment of Cervical Spondylolisthesis
To evaluate cervical spondylolisthesis, all intervertebral spaces from C2–3 to C6–7 in each patient were examined using a preoperative lateral radiogram of the cervical spine in the neutral position. We measured anterior-posterior translation of the upper vertebral body relative to the lower vertebral body. In this study, we defined cervical spondylolisthesis as 2 mm or more in the forward or backward direction.
4. Clinical and Radiological Data Analysis
This clinical study consisted of the 3 evaluations. First, we investigated the prevalence of cervical facet joint degeneration in all patients with DCM using the classification mentioned above. The prevalence of each CT grade at all spinal intervertebral levels was investigated. In addition, we compared the distribution of CT grades by dividing the joints into those at responsible or nonresponsible segmental levels to assess the impact of the CT classification on clinical diagnostic aspects and identify which type of degeneration is clinically significant in DCM. Second, we assess the clinical relationship between cervical facet joint degeneration and spondylolisthesis in patients with DCM. The patients whose evaluation of the lower cervical vertebra was impossible due to overlapping shoulders were excluded, and the assessment of each intervertebral space from C2–3 to C6–7 in the remaining patients were collected and investigated. By dividing the joints and intervertebral levels into at responsible and nonresponsible segmental levels, the prevalence of clinically significant cervical facet degeneration, as evaluated during the first step, and spondylolisthesis were assessed and compared. We also investigated the relationship between the presence of significant cervical facet degeneration on either side of both facet joints and spondylolisthesis at responsible and nonresponsible segmental levels, respectively. Third, we assessed the clinical impact of these 2 variables at the responsible segmental level on rapidly progressive myelopathy in patients with DCM. The same patients as in the second assessment were also involved. After dividing the patients into 2 groups according to the presence or absence of rapidly progressive myelopathy, we evaluated the association between rapidly progressive myelopathy and the presence of significant cervical facet degeneration or spondylolisthesis at the responsible segmental level, separately.
5. Statistical Analysis
All statistical analyses were performed with IBM SPSS Statistics ver. 26.0 (IBM Co., Armonk, NY, USA). Radiological variables at each spinal levels were compared using the Pearson chi-square test, and relationships between the radiological variables were assessed using the McNemar test. The reproducibility of the CT classification was evaluated using Cohen kappa coefficient. Data are presented as means± standard deviation (SD). Statistical significance was defined as p <0.05.
RESULTS
1. Clinical Characteristics
Although 145 patients were enrolled, 140 patients were finally included in this study (Fig. 2). As a result, 700 intervertebral levels and 1,400 cervical facet joints were assessed. The characteristics of the study population are presented in Table 1. There were 93 men and 47 women aged 38–93 years (mean± SD, 64.1 ± 12.8 years). Most patients had cervical canal stenosis (60.0%), followed by ossification of posterior longitudinal ligament (22.1%) and cervical disc herniation (17.9%). The most common responsible segmental level was C5–6 (37.1%), followed by C4–5 (35.0%). C2–3 was the least common (2.1%).
2. Prevalence of Cervical Facet Joint Degeneration
The overall prevalence of cervical facet degeneration is shown in Fig. 3A. In the all facet joint survey, the prevalence of grade 1, grade 2, grade 3, grade 4, grade 5A, and grade 5B degeneration was 72.0%, 9.5%, 10.9%, 4.3%, 2.9%, and 0.4%, respectively. The Kappa coefficient was 0.822 for the first diagnosis by 2 independent neurosurgeons, which suggested almost complete agreement in the 6-grade CT classification. The grade concordance of a pair of facets at each intervertebral level was 488 out of 700 intervertebral levels (69.7%). Notably, after classifying degeneration by responsible versus nonresponsible segmental level, there was a statistically significant difference between the 2 distributions (p <0.001), with grade 4 and grade 5B degeneration being more prevalent at the responsible segmental level and grade 5A degeneration being more prevalent at nonresponsible levels (Fig. 3B). Grades 4 and 5B degeneration, which reflect articular irregularities considered destructive facet joint degeneration, were grouped in further analyses.

Prevalence of cervical facet joint degeneration by grade. (A) Prevalence of cervical facet joint degeneration. (B) Prevalence of cervical facet joint degeneration at responsible and nonresponsible segmental levels. There was a statistically significant difference between the 2 distributions (p < 0.001), with grade 4 or 5B degeneration being more prevalent at the responsible segmental level and grade 5A being more prevalent at nonresponsible levels. Grade 1, normal facet joint with no degenerative changes. Grade 2, mild degenerative changes with only osteophyte formation. Grade 3, degenerative changes with osteophyte formation including joint space narrowing, microcyst (< 2 mm), or joint hypertrophy. Grade 4, severe degenerative changes including moderate to large cysts (≥ 2 mm), and articular irregularity. Grade 5A, ankylosing changes with bony fusion of the facet joint. Grade 5B, facet opening with articular irregularity.
3. Relationship Between Cervical Facet Joint Degeneration and Spondylolisthesis
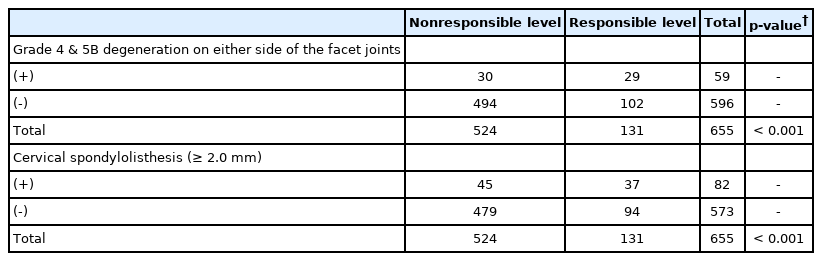
Evaluation of cervical spondylolisthesis was possible in 131 cases, because 9 patients were excluded for whom evaluation of the C6–7 vertebrae was impossible due to overlapping shoulders. Therefore, the following analysis was performed on 655 vertebrae. Spondylolisthesis of 2 mm or more was observed in 84 vertebrae (12.8%). Of the 131 patients with cervical myelopathy, 27 patients (20.6%) had rapid neurological deterioration before surgery. Therefore, 27 patients were classified into the rapid progression group and the remaining 104 patients into the slow progression group.
Grade 4 or 5B degeneration on either side of the cervical facet joints and spondylolisthesis were each observed with relatively high frequency at the responsible segmental level compared with nonresponsible levels. The prevalence of grade 4 or 5B degeneration in facet joints at the responsible level was 22.1% (29 out of 131 intervertebral levels), which was higher than 5.7% (30 out of 524 levels) at nonresponsible levels (p <0.001). The prevalence of cervical spondylolisthesis at the responsible level was 28.2% (37 out of 131 levels), which was also higher than 8.6% (45 out of 524 levels) at nonresponsible levels (p <0.001) (Fig. 4, Table 2).
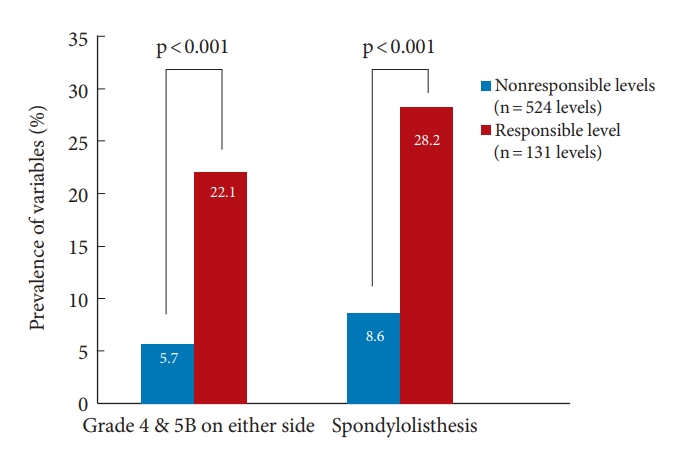
Prevalence of significant cervical facet degeneration and spondylolisthesis. The prevalence of grade 4 or 5B degeneration on either side of the facet joints at the responsible segmental level was 22.1%, which was higher than 5.7% at nonresponsible levels (p < 0.001). The prevalence of cervical spondylolisthesis at the responsible segmental level was 28.2%, higher than 8.6% at nonresponsible levels (p < 0.001). Grade 4, severe degenerative changes including moderate to large cysts (≥ 2 mm), and articular irregularity. Grade 5B, facet opening with articular irregularity.
Cervical facet degeneration with articular irregularity and spondylolisthesis at each of the spinal levels
Although there were similar trends for cervical facet joint degeneration and spondylolisthesis, there was no association between these 2 variables. There were no statistically significant differences between the presence of grade 4 or 5B degeneration on either side of both facet joints and the presence of spondylolisthesis at nonresponsible segmental levels (p = 0.142) (Table 3) or at the responsible level (p = 0.322) (Table 4).
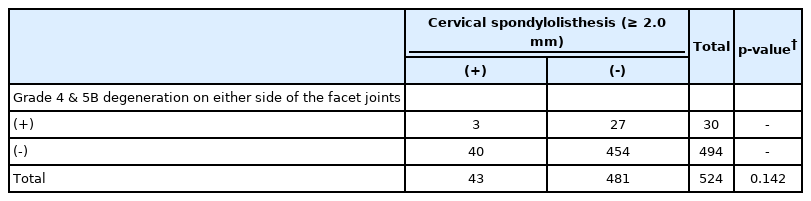
Relationship between cervical facet degenerations with articular irregularity and spondylolisthesis at the nonresponsible segmental level
4. Clinical Impact of Facet Joint Degeneration and Cervical Spondylolisthesis
In the investigation of the clinical impact of facet joint degeneration and cervical spondylolisthesis in patients with DCM, the prevalence of grade 4 or 5B degeneration on either side of the facet joint at the responsible segmental level was higher in the rapid progression group compared to the slow progression group (p <0.001). On the other hand, the prevalence of cervical spondylolisthesis at the responsible segmental level was higher in both the rapid and slow progression group, resulting in no statistical difference between the rapid and slow progression groups (Fig. 5) (p = 0.255).
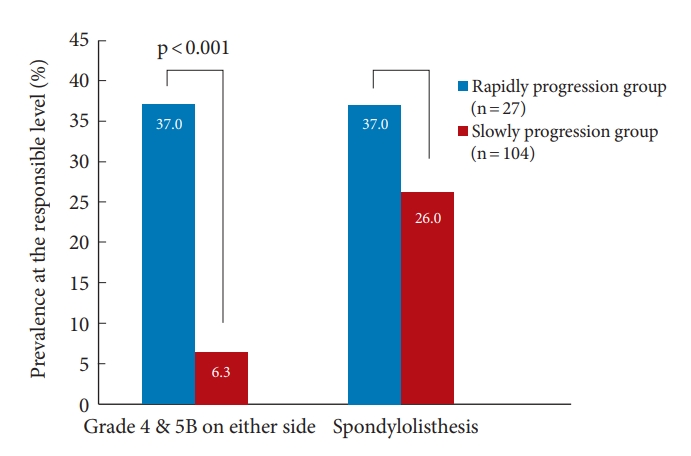
Impact of cervical facet degeneration and spondylolisthesis on preoperative rapidly progressive myelopathy. The prevalence of grade 4 or 5B degeneration on either side of the facet joints at the responsible segmental level was significantly higher in the rapid progression group than in the slow progression group (p < 0.001). On the other hand, there were no statistically significant differences in the prevalence of cervical spondylolisthesis at the responsible level between the 2 groups (p = 0.195). Grade 4, severe degenerative changes including moderate to large cysts (≥ 2 mm), and articular irregularity. Grade 5B, facet opening with articular irregularity.
DISCUSSION
The present study investigated clinical significance of facet joint degeneration in patients with DCM, by comparing the joints at responsible versus nonresponsible segmental levels. This is the first detailed comparative study of the association between facet joint degeneration and spondylolisthesis in DCM. The newly developed CT classification reflecting articular irregularity had few intraexaminer differences, and facet joint degeneration with articular irregularity and spondylolisthesis were more prevalent at the responsible segmental level. Moreover, this study showed that facet joint degeneration with articular irregularity at the responsible segmental level is significantly associated with rapid progression of myelopathy than slow progression of myelopathy. Although both articular irregularity and spondylolisthesis were significantly more prevalent at the responsible than the nonresponsible segmental levels, no such trend was observed in spondylolisthesis. We were able to clarify the clinical significance of facet joint degeneration; the impact of articular irregularity at a responsible segmental level was particularly significant in the rapid progression of DCM.
1. Evaluation of Cervical Facet Joint Degeneration
Age-related degeneration of the spine causes decreased mobility, stabilization, and bony fusion. In contrast, it can also cause increased local mobility and pathological conditions with intervertebral instability. Because the facet joints, a component of the cervical spine, play a role in static and gliding cervical motion and facilitate cervical spine mobility [9], they are also highly susceptible to degenerative changes [10]. With increasing age, the facet joints have thinner articular cartilage and more lax capsular ligaments; there is also bone erosion [11]. Capsular ligament stiffness affects segmental mobility and spatial positioning of the vertebra. The sagittal angle of the facet joint influences the distribution of disc pressure. These effects may result in a vicious cycle of cervical spine degeneration and instability [12]. In addition, the cumulative effect of micro-injury can initiate or accelerate cervical degeneration. Significant Modic changes are a predisposing factor for facet degeneration [13].
Facet joint degeneration of the spine also occurs not only with osteoarthritic bony changes but also with articular surface degeneration [11]. CT is more reliable than radiography or MRI in detecting facet arthrosis [14,15]. Therefore, we subdivided facet joint degeneration into 6 grades by including articular surface changes and intervertebral space opening in a new approach. Moreover, because cervical spondylosis is associated with a high incidence of asymptomatic lesions [1], we included assessment of responsible versus nonresponsible segmental level in this study. We found for the first time that articular irregularity of the facet joints is involved in the development of myelopathy, which might indicate that motion stress concentration is occurring locally.
2. Prevalence of Facet Joint Degeneration
There have been several attempts to classify cervical facet joint degeneration and determine its prevalence [4,14]. The prevalence of facet joint degeneration varied widely in previous reports. Park et al. [14] evaluated the facet joints of patients who underwent CT for cervical spine-related symptoms such as neck pain, pain radiating to the arm, or difficulty walking. They found that 8.63% of all the facet joints had some kind of degeneration, including 0.5% of degeneration with bony fusion. Kim et al. [4] investigated the facet joints in patients with non-spinal pathology. They found that 33% had facet joints with degenerative changes. Although it is difficult to discuss prevalence consistently because these studies had patients with different backgrounds and used their own CT classifications, they indicate a certain amount of asymptomatic facet degeneration. In the present study, some kind of degeneration occurred in 27.9% of the facet joints at nonresponsible segmental levels that were considered clinically silent. Because of the large number of these asymptomatic lesions, it is difficult to associate facet joint degeneration alone with the pathogenesis of DCM.
There has been a report on the prevalence of cervical facet joint degeneration based on a 4-grade CT classification of facet joint degeneration in the cervical spine: grade I, normal; grade II, degenerative changes including joint space narrowing, cyst formation, and small osteophytes without joint hypertrophy; grade III, joint hypertrophy; grade IV, bony fusion of the joint [14]. Although this study was innovative in that it focused on the facet joints, it was difficult to evaluate the clinical significance of facet joint degeneration because facet joint degeneration was classified into only 2 categories, except for the evaluation of “normal” and “bony fusion.” It was also difficult to detect the various changes related to facet degeneration based on only the 2 categories. In contrast, we classified joints into 6 grades in the present study. With our new classification, we found that 28.0% of facet joints had some type of degeneration, 2.9% had bony fusion (grade 5A), and 4.7% had articular irregularity (grade 4 or 5B). The presence of articular irregularity was more prevalent at the responsible segmental level than at nonresponsible levels, and the presence of bony fusion was conversely more prevalent at nonresponsible levels. In particular, the inclusion of articular irregularity in the classification provided a more detailed and clinically realistic assessment of facet joint degeneration.
We also investigated differences among evaluators, since subdivision of CT grades may cause differences in classification. In this newly proposed CT classification, the investigation of intraexaminer differences showed almost perfect agreement, despite a significant difference in the number of years of clinical experience between examiners. Therefore, this classification is a useful tool in daily clinical practice for evaluating the degree of facet joint degeneration in a comprehensive and effective manner.
3. Relationship Between Degeneration of Facet Joints and Degeneration of Other Structures
Previous studies evaluated the relationship between degeneration of facet joints and degeneration of other structures in the cervical spine. One study focused on degeneration of the vertebral disc, which is not associated with facet joint degeneration. Lee et al. [16] showed that facet joint degeneration depends on uncoveretebral joint degeneration and Modic change on MRI, but not disc or endplate degeneration, spinal stenosis, or ossification of the posterior longitudinal ligament. Moreover, there were no significant differences in disc height, segmental angle (SA), or SA range of motion based on the presence or absence of facet joint degeneration. Thus, advanced disc degeneration does not necessarily mean advanced facet joint degeneration. These results also suggest the need for the assessment of facet joint degeneration independent of the assessment of cervical disc degeneration.
On the other hand, cervical spondylolisthesis can be caused by severe facet degeneration [16]. Progressive loss of cartilage and articular remodeling as part of osteoarthritis can cause subluxation of the facet joint [11]. Therefore, facet joint degeneration can make a vertebral segment unstable and result in degenerative spondylolisthesis [2,17,18], resulting in symptomatic DCM. Therefore, these 2 factors, facet joint degeneration and spondylolisthesis, seem to be interrelated and can together lead to the onset of DCM. However, we reported a case of rapidly progressive DCM induced by severe unilateral facet joint degeneration without any trauma or cervical spondylolisthesis [6]. This case showed that the 2 factors are not necessarily interrelated concerning the onset of DCM, as indicated in the current study. The prevalence of grade 4 or 5B degeneration, suggesting destructive changes in the facet joint, was significantly higher at the responsible level than at nonresponsible levels. There was also no relationship between the presence of grade 5 or 5B facet degeneration and spondylolisthesis at either the responsible level or nonresponsible levels. These results suggest that articular irregularity, a form of facet joint degeneration, and the occurrence of cervical spondylolisthesis are not related to the onset of DCM, but that they may be independent factors in the development of myelopathy.
4. Clinical Impact of Facet Joint Degeneration
The clinical impact of cervical facet joint degeneration on myelopathy has not been well debated, but there are few relevant studies. Even in these studies, the clinical impact has not been sufficiently examined because the studies included evaluation of images from a wide range of patients, such as patients without symptoms or neck pain only [4,14], categorized patients into only 2 groups (presence or absence of facet joint abnormalities) [19], evaluated only facet joint tropism [20], focused on evaluating the reproducibility of the scoring system for facet degeneration [21], or included evaluations of other characteristics such as intervertebral height loss, anterior osteophytes, and endplate sclerosis [5]. Therefore, it would be very meaningful to develop a clinically relevant and appropriate method to evaluate facet joint degeneration. The current study investigated the clinical implications of a novel classification system.
DCM occurs due to the interrelated involvement of many factors [2,3,22,23]. As cervical facet joint degeneration progresses, spondylolisthesis will occur, but if there is already spinal canal stenosis related to factors such as osteophytes, disc protrusion, or ligamentous hypertrophy, cervical myelopathy might occur before spondylolisthesis. In the present study, the prevalence of grade 4 or 5B degeneration at the responsible segmental level was significantly higher in the rapid progression group than in the slow progression group, but the prevalence of cervical spondylolisthesis was not similar. This fact may inform us about the nature of the pathology. The cervical spine contains multiple joints and is highly susceptible to movement, but cervical degeneration does not occur uniformly. As a result of stress distribution, there may be a concentration of motion stress in one area, as in the case of adjacent segmental disease after fusion surgery. The articular irregularity indicates that excessive strain has been placed on the articular surfaces. Therefore, it is speculated that articular irregularity at the responsible segmental level may be a change that could reveal motion stress concentration. It is also speculated that if spinal cord compression is present in the background, this motion stress concentration may cause the rapid progression of cervical myelopathy. Further research is warranted in this respect.
5. Limitations
This study has several limitations. First, it used a retrospective design with a small number of patients. Second, it is uncertain whether the responsible segmental level was correctly identified in all patients. Third, the evaluation of cervical spondylolisthesis was not sufficient because there is no consensus on the definition of dynamic instability, which was not assessed in this study. Considering cervical spondylolisthesis, this study compared it only with articular irregularity of facet joints. It is speculated that patients who present with cervical spondylolisthesis at the responsible segmental level often have a low grade of facet degeneration. In addition, the spondylolisthesis in this study includes both forward and backward spondylolisthesis. Further studies are required on this point. Fourth, there is a pair of facet joints at each intervertebral height, and they do not always have the same degree of degeneration. If the contralateral facet joint was classified differently, it could have reduced the proportion of joints with grade 4 or 5B degeneration despite the presence of articular irregularity, which can underestimate the impact of facet joint degeneration with articular irregularity. Therefore, the clinical effect of grade 4 or 5B degeneration might be more significant. Despite these limitations, this study demonstrated the importance and clinical usefulness of evaluating cervical facet joint degeneration in patients with DCM.
CONCLUSION
This study was the first to focus on the potential importance of facet joint degenerative pathology and demonstrate the usefulness and reliability of a newly created CT classification of cervical facet joint degeneration in patients with DCM. The novel CT classification had few intraexaminer differences and deserves additional evaluation, suggesting that abnormal findings on articular surfaces might be related to the progression of myelopathy.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: YT; Data curation: YT; Formal analysis: YT; Methodology: YT; Project administration: HN; Visualization: AO, YT; Writing - original draft: AO; Writing - review & editing: YT, SY, FN, IN, YP.