Comparison Between 3-Dimensional-Printed Titanium and Polyetheretherketone Cages: 1-Year Outcome After Minimally Invasive Transforaminal Interbody Fusion
Article information
Abstract
Objective
Three-dimensional (3D)-printed titanium implants have been developed recently, but the utility is not yet proven. The aim of this study was to compare 3D-printed titanium and polyetheretherketone (PEEK) implants after minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF).
Methods
Between October 2018 and September 2021, we retrospectively analyzed 83 patients who underwent single-level MIS-TLIF (3D-printed titanium, 40; PEEK, 43). Radiologic parameters were assessed with x-ray and computed tomography (CT) at postoperative 1 week, 6 months, and 1 year. Clinical status was evaluated using Oswestry Disability Index, visual analogue scale score, and Bridwell fusion grading was assessed on 6-month and 1-year postoperative CT.
Results
There were no differences between the 2 groups in demographics and clinical outcomes. At 1-year of follow-up, the reported 3D-printed titanium fusion grades were grade I: 77.5% (31 patients), grade II: 17.5% (7 patients), and grade III: 5% (2 patients). The PEEK fusion grades were grade I: 51.2% (22 patients), grade II: 41.9% (18 patients), and grade III: 7.0% (3 patients). For overall fusion rate (grade I + II), there was no difference between the 2 cages (95.0% vs. 93.0%, p=0.705), but grade I was reported at a higher incidence in 3D-printed titanium than PEEK (77.5% vs. 51.2%, p=0.013). There was no difference between cages based on subsidence and complications.
Conclusion
There were no significant differences in the overall fusion rate for MIS-TLIF surgery between 3D-printed titanium and PEEK, but the fusion grade was better in 3D-printed titanium than in PEEK. Long-term follow-up is required to verify the effectiveness.
INTRODUCTION
Due to the increase in life expectancy, lumbar spine degenerative disease is increasing in the elderly population [1]. Consequentially, there have been advances in surgical methods for lumbar degenerative disease, and interbody cages has been widely and frequently used for lumbar fusion surgery [2,3]. Minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) is a more recently developed technique that is widely performed in lumbar degenerative diseases and has a high fusion rate [4-7]. Many kinds of cages have been used for lumbar interbody fusion, and the 2 most popular cages are titanium and polyetheretherketone (PEEK). These interbody cages have been routinely used in fusion surgery and have been reported to have positive results [8-10]. However, there are some disadvantages to these traditional solid titanium and PEEK cages. Solid titanium cages have a good fusion rate, but subsidence is frequent due to the high elastic modulus, and there are disadvantages for radiolopaque [11,12]. The PEEK cage complements the titanium shortcomings because it has radiolucency, and elastic modulus is similar to human cortical bone [13]. However, the titanium cage promotes cell adhesion and is advantageous for bone fusion due to better osseous-integration and biocompatibility than the PEEK cage [14].
With developments in 3D-printing technology, many spine implants using 3D-printing technology have been released [15]. The 3D-printer could produce a tailored cage to each patient and a desired shape or a complex shape [16-18]. Therefore, recently produced 3D-printed titanium cages can be generated to reduce elastic modulus; they are produced with a rough surface and structure and an ideal porocity [14]. These structures have similar properties to cancellous tissue and facilitate osteoblast cell regrowth [19]. Therefore, we compared the fusion rate and quality of fusion for 3D-printed titanium and PEEK cages.
MATERIALS AND METHODS
1. Patient Population
Between October 2018 and September 2021, we retrospectively analyzed 83 patients who underwent single-level MISTLIF. The patients with follow-up more than 1-year were included in this study, and perioperative, clinical and radiologic date were collected. A total of 40 patients underwent MIS-TLIF with a 3D-printed titanium cage (PANTHER, Mantiz, Daegu, Korea), and 43 patients with a PEEK cage (CAPSTONE, Medtronic, Memphis, TN, USA). All patients had persistent low back pain and radiating pain in the lower extremities despite 3 months of conservative treatment. These patients had spinal stenosis (central or foraminal stenosis), recurrent herniated disc, spondylolisthesis, or instability. The patients were not diagnosed with osteoporosis and were not treated with antiosteoporosis agents. The Institutional Review Board of Gangnam Severance Hospital, Yonsei University College of Medicine approved this study (No. 2020-0971-001).
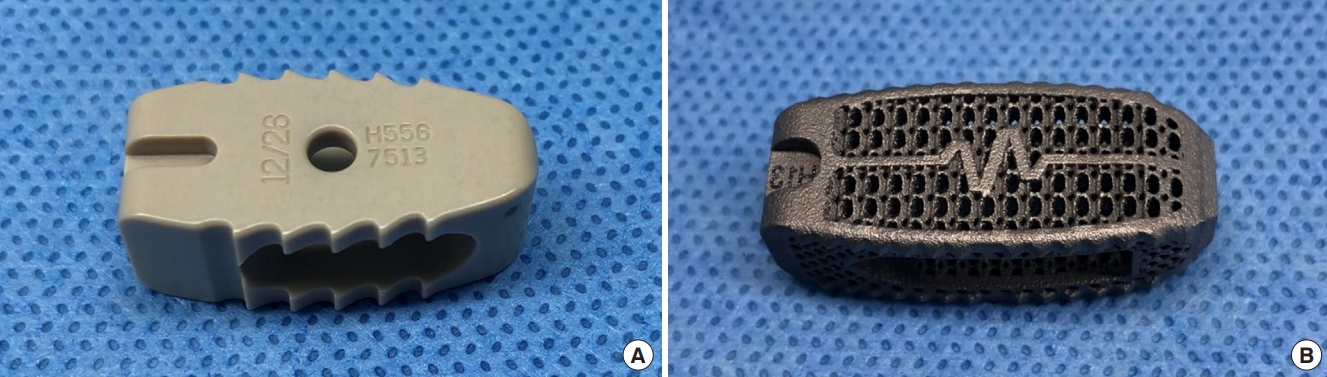
2. Preparation of 3D-Printed Titanium Cage
We used a 3D-printed titanium cage based on patient disc size (PANTHER, Mantiz, Daegu, Korea) (Fig. 1). This 3D model was produced using metal power bed fusion technology, which is also known as a Selective Laser Melting 3D printer (EP-M250, Shining 3D Tech., Hangzhou, China). This 3D-printed titanium cage has a mean pore size range of 630 μm to 730 μm and a mean porosity range of 70% to 80%. A straight bullet type was used for both the PEEK and the 3D-printed titanium cage. The height and length were measured and applied according to the patient's anatomical characteristics. This 3D-printed titanium cage was a standard-made, and height and length of the cage did not differ with PEEK cage.
3. Surgical Technique
The MIS-TLIF was performed as previously described [20], and the MIS-TLIF surgery was performed from the symptomatic side of the patient. The surgical level was confirmed under C-arm guidance. A 3-cm incision was applied at lateral pedicle line on disc space, and a working channel was created with a tubular retractor (METRx, Medtronic, Memphis, TN, USA). Total facetectomy, partial laminectomy, and ligamentum flavum removal were performed using a high-speed drill, osteotome, Kerrison punch, and pituitary rongeur. Contralateral side decompression was performed in all patients, and discectomy and preparation of disc space for fusion were conducted. Autologous local bone was inserted in the empty disc space. Both 3D-printed titanium and PEEK cage were filled with a mixture of demineralized bone matrix and small autologous local bone, and the fusion material in both cages were the same except for the cage. During this process, we placed the cage at as much of a transverse angle as possible (Fig. 2). Finally, the percutaneous pedicle screw was inserted into the appropriate position under fluoroscopic guidance. All pedicle screws were the same (ZENIUS, Medyssey, Jecheon, Korea). All procedures were performed by one neurosurgeon, who had sufficient MIS-TLIF experience (more than 1,000 cases).
4. Clinical Assessment
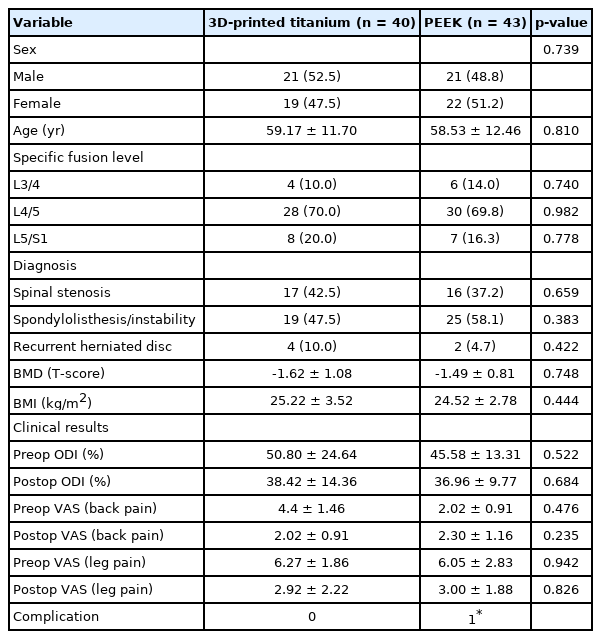
Collected patient information was demographics, medical comorbidities, surgical level, and surgical indications. Each patient was evaluated on an outpatient basis within 1 week and at about 1 year after surgery for Oswestry Disability Index (ODI), visual analogue scale (VAS) score, bone mineral density (BMD), and body mass index (BMI) (Table 1).
5. Radiologic Examination
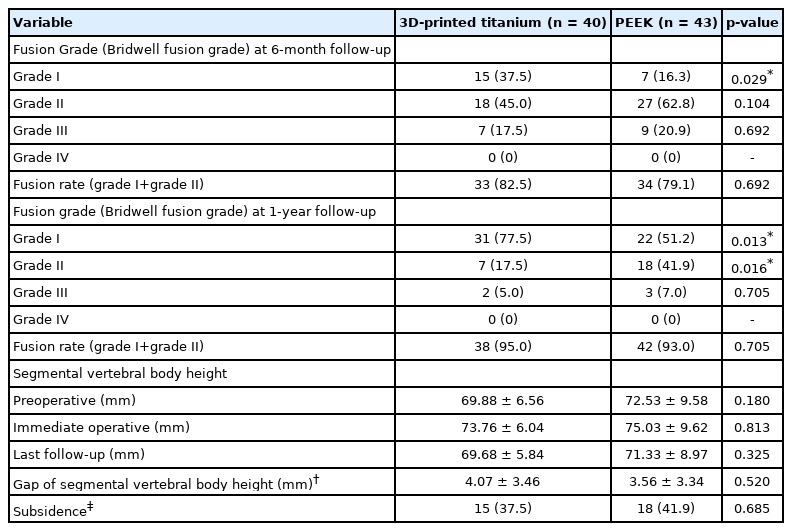
The x-ray and CT scans were performed at approximately 6 months and 1 year after surgery. Bone fusion was defined according to the Bridwell fusion grading system based on CT performed at 6 months and 1 year postoperative [21]. The Bridwell fusion grades were as follows: grade I, fused with trabecular bone formation; grade II, graft was intact but not completely remodeled, and there was no lucency in the upper and lower parts of the graft; grade III, graft was intact, but there was lucency above and below the graft; grade IV, fusion was absent with collapse or resorption of graft (Fig. 3). The calculated fusion rate was the sum of grades I and II.
Fusion assessed with the Bridwell grading system. The upper row is a 3-dimensional-printed titanium cage, and the lower row is a polyetheretherketone cage. (A) Grade I, (B) grade II, (C) grade III. Fusion was graded from I to IV: Fusion with remodeling and trabeculae (I); graft intact, not fully remodeled and incorporated, but no lucency (II); graft intact, potential lucency at the top and bottom of the graft (III); and fusion absent with collapse/resorption of graft (IV). According to the Bridwell grading system, solid fusion is defined as grade I and II based on radiologic outcomes. There was no grade IV in the study.
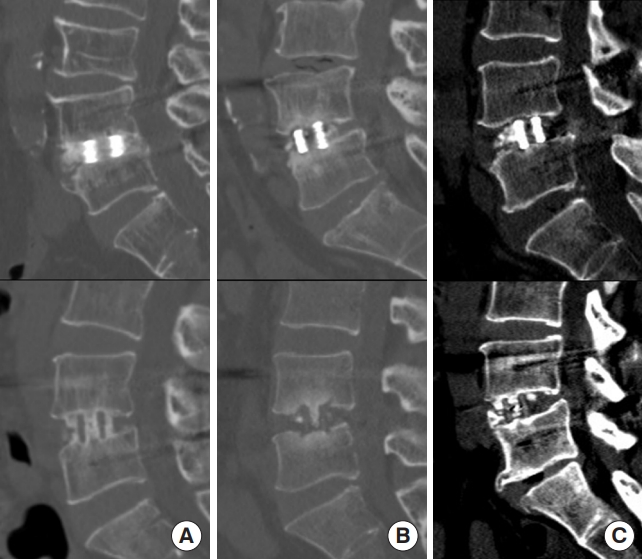
Measurement of subsidence is inconsistently defined in the literature because of use of relative and absolute measurements, and the most frequently used measurement method for defining subsidence was based on a threshold of 2 mm [22,23]. Therefore, we defined “subsidence” as segmental vertebral body height decrease by 2 mm or more at the last follow-up compared with 1 week after surgery. Segmental vertebral body height was measured from the midpoint of the cranial endplate of the upper vertebra to the caudal endplate of the lower vertebra (Fig. 4). The evaluation of the radiologic parameters was independently measured by 2 physicians not related to the surgery, and the average value was calculated.
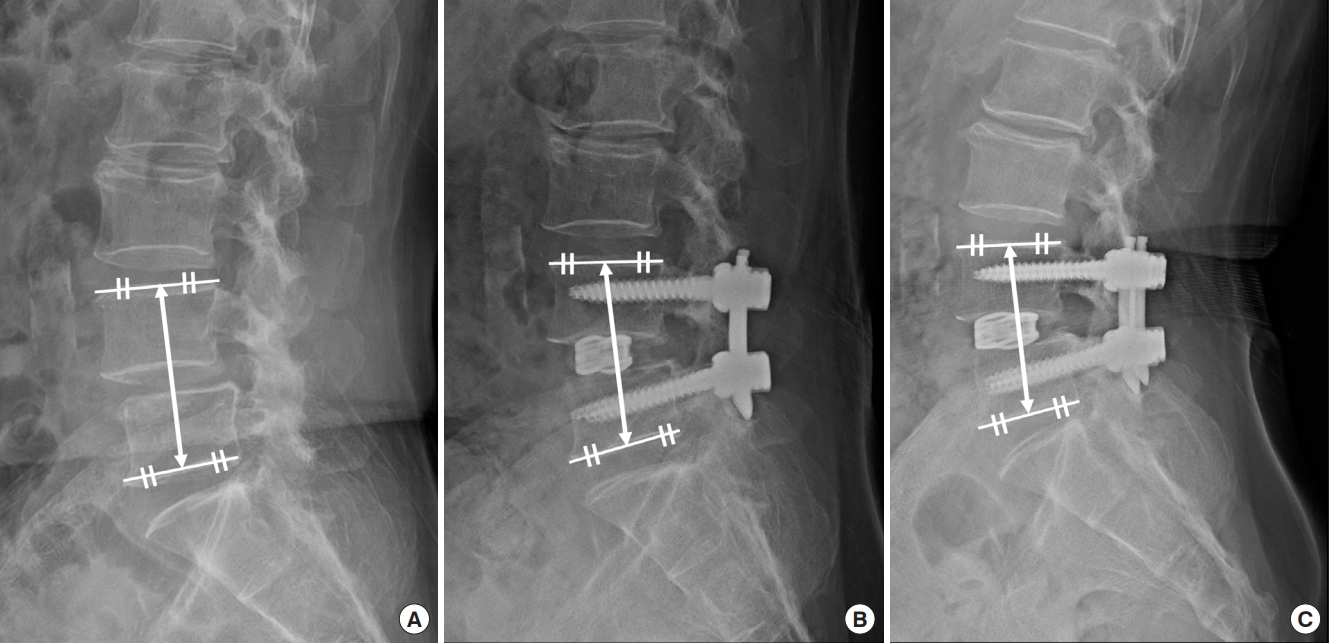
Segmental vertebral body height. The distance between the midpoint of the cranial vertebral upper endplate and the midpoint of the caudal vertebral lower endplate at the fusion level. Segmental vertebral height was measured at preoperative (A), 1-week postoperative (B), and 6-month postoperative x-ray (C). Subsidence was measured as segmental vertebral body height difference between immediate postoperative (A) (68.3 mm) and final follow-up x-ray (B) (62.6 mm).
6. Statistical Analysis
Chi-square test, Student t-test, and Mann-Whitney U-test were used for statistical analysis using IBM SPSS Statistics ver. 25.0 (IBM Co., Armonk, NY, USA). Data are expressed as mean and standard deviation. A p-value lower than 0.05 was considered statistically significant.
RESULTS
We retrospectively analyzed the data of 83 patients who underwent single-level MIS-TLIF surgery for degenerative lumbar disease. Of the total 83 patients, 40 were in the 3D-printed titanium group and 43 were in the PEEK cage group. There were no statistically significant differences in sex and age between the 2 groups (Table 1). A fusion level of L4/5 was the most frequent site for specific surgery in both groups (70% vs. 69.8%) (Table 1). There was no statistically significant difference in BMD, BMI, and clinical results (ODI or VAS) (Table 1).
Successful fusion according to the Bridwell fusion grading system was observed in 33 patients (82.5%) in the 3D-printed titanium cage and 34 patients (79.1%) in the PEEK cage at 6-month follow-up and was observed 38 patients (95%) in the 3D-printed titanium and 42 patients (93%) in the PEEK cage at 1-year follow-up. This difference was not significant at 6 months and 1 year after surgery (82.5% vs. 79.1%, p=0.692, 95.0% vs. 93.0%, p=0.705, respectively). However, there was a difference in detailed fusion grade between the 2 cages. In the 3D-printed titanium cage, grade I was 37.5%, grade II was 45.0%, and grade III was 17.5% at 6-month follow-up. At 1-year follow-up of 3D-printed titanium cage, grade I was 77.5%, grade II was 17.5%, and grade III was 5%. Meanwhile, in the PEEK, grade I was 16.3%, grade II was 62.4%, grade III was 20.9% at 6-month follow-up. At 1-year follow-up of PEEK, grade I was 51.2%, grade II was 41.9%, grade III was 7%. There was no grade IV in either group (Table 2). Based on these results, only grade I was statistically significantly higher in 3D-printed titanium than PEEK cage at 6-month and 1-year follow-up. (37.5% vs. 16.3% at 6-months, p=0.029, 77.5% vs. 51.2% at 1-year, p=0.013) (Table 2).
Among patients who underwent surgery at L4/5, there were 28 patients in the 3D-printed titanium and 30 patients in the PEEK cage. The fusion rate was not significant at 6 month and 1 year after surgery (82.1% vs. 76.7%, p=0.462, 96.4% vs. 96.7%, p=0.737, respectively). In L4/5, there was also a difference in detailed fusion grade between the 2 cages. In the 3D-printed titanium cage, grade I was 35.7%, grade II was 46.4%, and grade III was 17.9% at 6-month follow-up. In addition, at 1-year follow-up of 3D-printed titanium cage, grade I was 78.6%, grade II was 17.9%, and grade III was 3.6%. Meanwhile, in the PEEK, grade I was 13.3%, grade II was 63.3%, grade III was 23.3%. In addition, at 1-year follow-up of PEEK, grade I was 53.3%, grade II was 43.3%, grade III was 3.3% (Table 3).
No significant differences were found between groups in segmental vertebral body height at preoperative, immediate postoperative, and final follow-up. In addition, subsidence occurred in 15 patients (37.5%) in the 3D-printed titanium cage and 18 patients (41.9%) in the PEEK cage. There was no difference between the 2 cages in incidence rate of subsidence (37.5% vs. 41.9%, p=0.685) or difference in segmental vertebral body height (segmental vertebral body height difference between immediate postoperative and final follow-up x-ray) (4.07 mm vs. 3.56 mm, p=0.520) (Table 2). In addition, when the patients who underwent surgery at L4/5 level were selected, There was no difference between the 2 cages in incidence rate of subsidence (35.7% vs. 43.3%, p=0.373) or difference in segmental vertebral body height (segmental vertebral body height difference between immediate postoperative and final follow-up x-ray) (4.38 mm vs. 3.11 mm, p=0.224) (Table 3).
DISCUSSION
Previous studies have shown that MIS-TLIF was effective surgical treatment in degenerative lumbar spine disease, and the aim of TLIF is to stabilize the unstable movement of the spine by fusion. PEEK has been associated with weaker imaging disturbance in CT and x-ray, because of radiolucency. In addition, PEEK has been reported less mechanical complications, because of lower elastic modulus [13]. Despite these advantages, due to the inherent characteristics of PEEK, integration of osteoblast is low [24]. Olivares-Navarrete et al. [25] reported that fibrous tissues grow around PEEK implants because osteoblastic differentiation of progenitor cells decreases and inflammatory reactions increase due to apoptosis and necrosis. In addition, McGilvray et al. [19] found through histopathology that PEEK implants had poorly vascularized fibrous connective tissue and increased inflammatory response, consisting of lymphocytes and macrophages, in an in vivo ovine lumbar fusion model.
In comparison, titanium is advantageous for bone remodeling and inducing bony fusion due to good biocompatibility and induced osseous-integration of titanium, resulting in a high fusion rate [26,27]. Olivares-Navarrete et al. [28] reported that titanium has osteogenic conditions including bone morphogenetic proteins (BMPs) BMP2, BMP4, and BMP7 compared to PEEK; as a result, osteoblast maturation is increased. In addition, several studies have suggested that the difference in osteogenic environment is due to structural difference between the surfaces of PEEK and titanium cages [29,30]. The fusion rate showed varying results depending on method and follow-up period. In the follow-up period of 1 year, the fusion rate of the solid traditional titanium cage ranged from 53% to 96%, while that of the PEEK cage ranged from 32% to 74.5% [8-10,26,27]. At a 6-month follow-up, the fusion rate of the titanium cage in posterior lumbar interbody fusion was 91.4% [31], and that of the PEEK cage was 86.7% [32]. However, previous comparison between titanium and PEEK cages has been performed with a solid titanium cage instead of a 3D-printed titanium cage. The 3D-printed titanium cage has a finer structure than solid titanium cage, which can increase the porosity and decrease the elastic modulus. Titanium has been used for a long time as a major material for fracture and fusion surgery due to its high biocompatibility with bone. Solid titanium cage has also been used for interbody fusion for a long time, but due to its high elastic modulus and subsidence rate, it has been replaced by PEEK cage. The 3D-printed titanium cage was developed to overcome the elastic modulus problem of solid titanium and maintain the advantage of biocompatibility [14-17,19].
In our study, there was no difference in early-stage fusion rate between 3D-printed titanium and PEEK cages (82.5% vs. 79.1% at 6 months, 95.0% vs. 93.0% at 1 year). However, when comparing patients of fusion grade I, the quality was better in the 3D-printed titanium than in PEEK cage (37.5% vs. 16.3% at 6 months, 77.5% vs. 51.2% at 1 year) (Table 2). In order to exclude biomechanical effects according to each fusion level, there was no difference from the previous results when the fusion grade was measured for patients who had undergone at L4/5 (35.7% vs. 13.3% at 6 months, 78.6% vs. 53.3% at 1 year) (Table 3). This is the first study to evaluate early-stage fusion rate and to compare 3D-printed titanium and PEEK cages. We hypothesize that there will be no difference in fusion rate between 3D-printed titanium and PEEK cages in long-term follow-up, though 3D-printed titanium may be more advantageous in the early stage. This difference could be attributable to the more porous structure in the titanium cage due to application of 3D-printing technology and to the structural similarity to physiological cancellous bone [33]. These structures showed good biocompatibility and induced osseous-integration [14,34,35].
Previous studies have indicated that solid titanium has a high elastic modulus, so subsidence incidence is high [11,12,36]. Several studies have shown differences in subsidence between solid titanium and PEEK cages, with subsidence ratio ranging from 16% to 35% in solid titanium and from 0% to 28% in PEEK cages [11,12,26,37-39]. Our study is the first comparative study to evaluate the subsidence between 3D-printed titanium and PEEK cages, and the results indicate no significant difference between the 2 cages in incidence of subsidence. Differences could be attributable to the unique porous 3D-printed titanium cage structure, and the elastic modulus could be adjusted by changing the size of the porosity. Therefore, it was possible to maintain an elastic modulus similar to the physiological level, resulting in no difference in fusion rate or incidence of subsidence with PEEK cage [14,34,35]. In this study, subsidence was relatively high (3D-printed titanium, 37.5%; PEEK, 41.9%), but there were no significant differences in preoperative segmental vertebral body height or final follow-up metrics (3D-printed titanium, 69.88 to 69.68 mm; PEEK, 72.53 to 71.33 mm). This indicates that clinically meaningful subsidence was not high (Table 2).
This study had several limitations. First, it was difficult to determine final fusion because the 3D-printed titanium cage is relatively new, and the long-term fusion rate cannot be measured. Second, due to the radiologic interference of titanium, it may be difficult to distinguish fusion grade. Third, since the occurrence of subsidence was based only on radiographic and morphologic results, it is difficult to determine whether clinical subsidence occurred. This limitation seemed to have occurred due to the short follow-up period, therefore, all cases in this study will be followed for more than 2 years to report the final results. Despite the limitations described, this study is the first to clinically compare the fusion rates of 3D-printed titanium and PEEK cage. In addition, we observed that the 3D-printed titanium showed better fusion quality than PEEK cage in early preliminary outcomes after MIS-TLIF, which is likely because of the difference in porous structure and biocompatibility of 3D-printed titanium. With development of recent 3D-printing technology, it is possible to overcome the limitations of PEEK and solid titanium implants, and we are confident that 3D-printed titanium cage will be used increasingly for spine fusion.
CONCLUSION
The overall fusion rate of MIS-TLIF surgery showed no significant difference between 3D-printed titanium and PEEK cages. In addition, there was no difference between the 2 groups in incidence of subsidence. However, fusion grade was better in the 3D-printed titanium than PEEK cage. With development of recent 3D-printing technology, it is possible to overcome the limitations of previous spine implants, and we are confident that 3D-printed titanium technology will contribute to improvements in spine fusion surgery.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: JP; Data curation: DK, OK; Formal analysis: DK, OK; Funding acquisition: DK; Methodology: DK, OK; Project administration: JP; Writing - original draft: DK; Writing - review & editing: JP.