Freehand Juxtapedicular Screws Placed in the Apical Concavity of Adult Idiopathic Scoliosis Patients: Technique, Computed Tomography Confirmation, and Radiographic Results
Article information
Abstract
Objective
The purpose of this study is to highlight our technique for freehand placement of juxtapedicular screws along with intraoperative computed tomography (CT) and radiographic results.
Methods
Consecutive patients with adult idiopathic scoliosis undergoing primary surgery by the senior author were identified. All type D (absent/slit like channel) pedicles were identified on preoperative CT. Three-dimensional visualization software was used to measure screw angulation and purchase. Radiographs were measured by a fellowship trained spine surgeon. The freehand technique was used to place all screws in a juxtapedicular fashion without any fluoroscopic, radiographic, navigational or robotic assistance.
Results
Seventy-three juxtapedicular screws were analyzed. The most common level was T7 (9 screws) on the left and T5 (12 screws) on the right. The average medial angulation was 20.7° (range, 7.1°–36.3°), lateral vertebral body purchase was 13.4 mm (range, 0–28.9 mm), and medial vertebral body purchase was 21.1 mm (range, 8.9–31.8 mm). More than half (53.4%) of the screws had bicortical purchase. Two screws were lateral on CT scan, defined by the screw axis lateral to the lateral vertebral body cortex. No screws were medial. There was a difference in medial angulation between screws with (n = 58) and without (n = 15) lateral body purchase (22.0±4.9 vs. 15.5±4.5, p < 0.001). Three of 73 screws were repositioned after intraoperative CT. There were no neurovascular complications. The mean coronal cobb corrections for main thoracic and lumbar curves were 83.0% and 80.5%, respectively, at an average of 17.5 months postoperative.
Conclusion
Freehand juxtapedicular screw placement is a safe technique for type D pedicles in adult idiopathic scoliosis patients.
INTRODUCTION
Pedicle screw instrumentation of the thoracolumbar spine is a critical component of modern spinal surgery and facilitates powerful correction of spinal deformities. Freehand placement of thoracolumbar pedicle screws has been shown to be a safe and reproducible technique [1-3]. The purchase for transpedicular screws relies on the screw traversing the cancellous channel of the pedicle [4].
Juxtapedicular, or extrapedicular, screw placement is a previously described method for screw fixation in the case of small or absent pedicles [5,6]. Watanabe et al. [4] identified 4 pedicle types in scoliosis patients based upon the size of the cancellous channel. Type A pedicles have a “large cancellous channel,” type B a “small cancellous channel,” type C a “cortical channel” that a pedicle probe can be inserted with a mallet, and type D is a “slit/absent channel,” that warrants a juxtapedicular screw position. The technique for freehand juxtapedicular screw placement has been inconsistently described. In addition, several publications recommend a starting point at the tip of the transverse process [6,7]. Due to this lateral starting point, the resulting screw would require an offset connector to be in-line with the rest of the transpedicular screws. Moreover, the dorsal position of the tip of the transverse process increases the distance to vertebral body making freehand instrumentation more challenging [8]. The purpose of this study is to highlight the freehand technique for juxtapedicular screw placement along with intraoperative CT and radiographic results in a retrospective series of adult idiopathic scoliosis patients.
MATERIALS AND METHODS
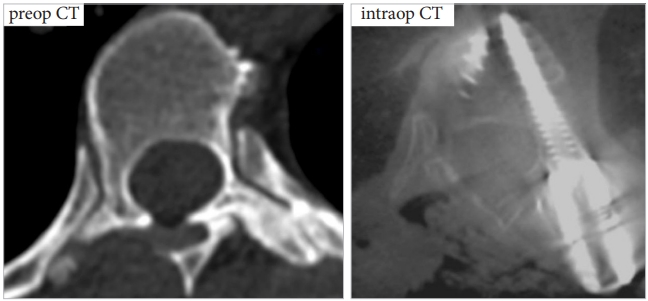
Consecutive patients (n = 25) with adult idiopathic scoliosis undergoing primary surgery by the senior author were identified. All type D pedicles with absent channels were identified on preoperative CT. Operative notes and instrumentation logs were reviewed to identify screw sizes. Intraoperative CT scan images obtained after screw placement were analyzed with 3-dimensional visualization software was used to measure screw angulation and purchase (Figs. 1, 2). Postoperative radiographs were used to analyze curve correction.
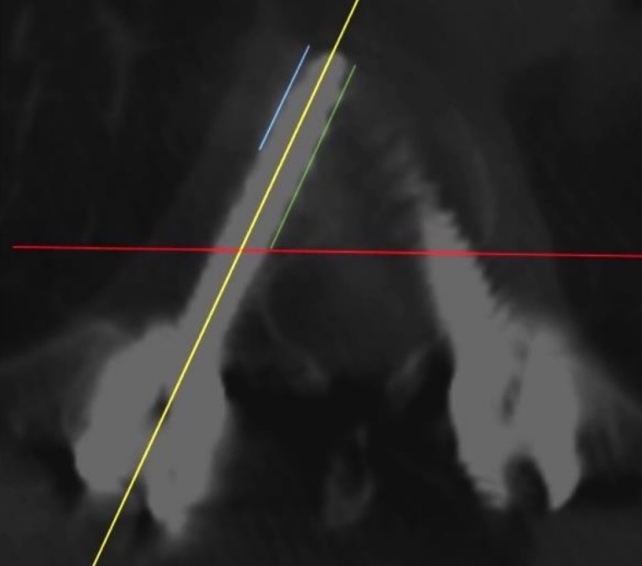
Visualization software for pedicle instrumentation determination. Red line, dorsal limit of vertebral body; yellow line, screw axis; green line, medial vertebral body purchase; blue line, lateral vertebral body purchase.
1. Surgical Technique
Our technique is similar to the previously published freehand placement of juxtapedicular pedicle screws (Fig. 3):

Step-by-step illustration of the juxtapedicular screw placement technique. (A) Creation of pilot hole with matchstick burr, using traditional anatomical landmarks. (B) Insertion of slightly curved gearshift down the lateral pedicle with the curved tip directed medially. (C) Following palpation of competent lateral vertebral body wall and screw length measurement using a flexible ball tip probe, placement of K-wire into pathway. (D) Undertap by 1mm with an open cannulated tap to visualize that the K-wire is not advancing. (E) Screw placement.
(1) Meticulous exposure of the dorsal bony surface
(2) Creation of ventral starting point creation by removing the dorsal transverse process bone to the depth of the superior articulating facet [8]
(3) Starting point on the transverse process is in-line with the lateral edge of the superior articular facet in the thoracic spine and 1 mm lateral to the ascending pars in the lumbar spine
(4) Create pilot hole into juxtapedicular space using a matchstick burr
(5) Glide down lateral pedicle using a 1mm “baby” slightly curved gearshift with the curved tip directed medially to depth of 15 mm in the thoracic spine and 20 mm in the lumbar spine
(6) Enter lateral vertebral body at the pedicle-body junction
(7) Palpation of competent lateral vertebral body wall and screw length measurement using a flexible ball tip probe
(8) Place K-wire into pathway and undertap by 1mm with an open cannulated tap to visualize that the K-wire is not advancing
(9) Re-palpation of the bony tract ventrally in the vertebral body
(10) Screw placement
RESULTS
1. Instrumentation Characteristics
A total of 73 juxtapedicular screws were analyzed with intraoperative computed tomography (CT). The most common level for juxtapedicular screw placement was T7 (9 screws) on the left and T5 (12 screws) on the right, with 8 screws placed in the upper lumbar region (Table 1, Fig. 4). Screw widths had the following distribution: 15.1% of screws were 5.5 mm, 68.5% were 6.0 mm, 15.1% were 6.5 mm, and 1.4% were 7.0 mm. The average screw length was 35 mm (range, 30–45 mm) (Table 2).

Distribution of juxtapedicular screw placement by instrumented level. Yellow areas signify the most common levels in the patient cohort.
2. Screw Placement
The average medial angulation of screw placement was 20.7° (range, 7.1°–36.3°), lateral vertebral body purchase was 13.4 mm (range, 0–28.9 mm), and medial vertebral body purchase was 21.1 mm (range, 8.9–31.8). More than half (53.4%) of the screws had bicortical purchase, without significant anterior breach (< 3 mm). Two screws had a lateral breach on CT scan, defined by the screw axis lateral to the lateral vertebral body cortex. No screws were medially breached. There was a difference in medial angulation between screws with (n = 58) and without (n = 15) lateral body purchase (22.0±4.9 vs. 15.5±4.5, p < 0.001). Thoracic (n = 65) and lumbar (n = 8) screws showed significant differences in screw length (37.5±3.2 mm vs. 44.4±1.8 mm, p < 0.001) and vertebral body purchase (16.4±15 mm vs. 23.8±20.0 mm, p = 0.0007), but no difference in screw angulation (20.7°±5.6° vs. 20.4°±3.9°, p = 0.871).
3. Surgical Outcomes
Three of seventy-three screws were repositioned after intraoperative CT. There were no neurovascular complications. The mean coronal cobb corrections for main thoracic and lumbar curves were 83.0% and 80.5%, respectively, at an average follow-up of 17.5 months postoperative. A representative case is shown in Fig. 5.

Representative case: a 59-year-old female with adult idiopathic scoliosis presenting with imbalance, back and leg pain. Preoperative films show structural (major) curves in the main thoracic and thoracolumbar/lumbar regions (Lenke type 6/S/Sag Malaign), with Type D pedicles on the right L2 and left T5. The patient underwent a T2 to sacrum correction, with a unilateral L2 pedicle subtraction osteotomy and transforaminal lumbar interbodies were placed from L3 to the sacrum. Greater than 80% correction of both curves was achieved.
DISCUSSION
In scoliosis and spinal deformity surgery, pedicle screw fixation is a hallmark of achieving segmental stabilization. Transpedicular instrumentation achieves fixation in all 3 columns, allowing for rigid fixation and improved deformity correction [9-11]. In adult idiopathic scoliosis (AdIS), differences in pedicle morphology on the convex versus concave sides of a spinal deformity have been well documented with narrower pedicle widths on the side of the concavity, creating additional challenges for transpedicular instrumentation [12-16]. Juxtapedicular, or extrapedicular, screw placement is a previously described method for screw fixation in the case of small or absent pedicles [5-7]. The purpose of this manuscript to is describe our technique and radiographic results for freehand juxtapedicular screw placement in AdIS patients.
In this study, we found that 70 of 73 (95.8%) of screws were placed successfully using our freehand technique with confirmation on intraoperative CT scan after screw placement. There were no neurovascular complications, as has been shown in previous similar studies [2,9]. The most common screw diameter was 6.0 mm and the most commonly instrumented levels were at T4, T5, and T7.
Freehand pedicle screw placement without the guidance of intraoperative fluoroscopic, radiographic navigation or robotics, has been shown to be safe and reproducible. In a retrospective study of 3,204 freehand thoracic pedicle screws, Kim et al. [1] found that out of 577 screws randomly assigned for CT analysis, only 10 (1.7%) violated the medial wall, and no screws had caused neurovascular compromise with up to 10-year follow-up [4]. In a retrospective series of 115 consecutive patients receiving 1,035 thoracic pedicle screws for scoliosis correction, Di Silvestre et al. [16] found a screws misplacement rate of 1.7%, with no occurrence of neurovascular complication. The use of intraoperative navigation and robotic assistance has been gaining popularity and has demonstrated high levels of accuracy as well [17,18]. However, we believe it remains critical for spine deformity surgeons to understand the technique for freehand juxtapedicular screw placement.
Juxtapedicular screw placement has been previously described in several papers but with a very dorsal and lateral starting point over the tip of the transverse process. In a cadaveric study of extrapedicular screw placement at T3–10 levels, Husted et al. [6] determined that extrapedicular screws can be safely and effectively placed throughout the thoracic spine using the transverse process starting point. In a comparative study between transpedicular and extrapedicular instrumentation, White et al. [5] demonstrated in a cadaver model that while transpedicular screws were stronger in both axial and sagittal loading methods, the difference was small, suggesting that juxtapedicular placement provides an acceptable alternative method for instrumentation.
In this study, juxapedicular screws were frequency placed at T3–5 on the right and T6–9 on the left, corresponding to the concavity of the proximal and main thoracic curves in idiopathic scoliosis. These findings are in agreement with previous studies which show type C and D pedicles are most often found in the concavity of scoliotic curves [4]. Our technique differs from previous descriptions in that that starting point is more ventral and medial. We have previously shown that a more ventral starting point generates a 51% increase in maximal insertional arc, allowing for safer freehand pedicle screw placement [8]. This shortens the distance from the starting point to the target vertebral body in juxtapedicular screw placement, thereby minimizing the margin for error. In addition, by starting only 1mm more lateral than a transpedicular screw, the screw heads can be well-aligned with the rest of the construct.
The current study has several limitations. Longitudinal patient data to assess outcomes and fusion rates were not available due to the short length of follow-up. However, the main purpose of this study was to assess the technical considerations and accuracy for instrumentation of small apical concave type D pedicles. There was no biomechanical testing as part of this study, and therefore the strength and pullout assessment of juxtapedicular screws (versus conventional pedicle screws) cannot be determined. However, the excellent overall coronal cobb correction rates speak to adequate vertebral purchase to allow for this amount of correction. Future studies are necessary to analyze long term patient outcomes, fusion rates, and biomechanical properties of juxtapedicular screws in the AdIS population.
CONCLUSION
The freehand technique for juxtapedicular screw placement of type D pedicles in AdIS is a safe and effective technique. Careful preoperative analysis, intraoperative technical execution with CT scan verification and appropriate instrumentation techniques can provide adequate deformity correction in these adult patients.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: JDL, RAL, LGL; Data curation: JDL, JAO, NJL, JML; Formal analysis: AJS, NJL; Methodology: AJS, JDL, RAL, LGL; Project administration: JDL, NJL, JMS, LGL; Writing - original draft: AJS, JDL; Writing - review & editing: AJS, JDL, JAO, JMS, RAL, LGL.