Cervical Inclination Angle: Normative Values in an Adult Multiethnic Asymptomatic Population
Article information
Abstract
Objective
The role of the craniocervical complex in spinal sagittal alignment has rarely been analyzed but it may play a fundamental role in postoperative mechanical complications. The aim of the study is to analyze the normative value of the cervical inclination angle (CIA) in an adult asymptomatic multiethnic population.
Methods
Standing full-spine EOS of adult asymptomatic volunteers from 5 different countries were analyzed. The CIA was analyzed globally and then in each decade of life. Different ethnicities were compared. Comparisons between different groups was performed using a t-test and statistical significance was considered with a p-value < 0.05.
Results
EOS of 468 volunteers were analyzed. The global mean CIA was 80.2° with a maximum difference of 9° between T1 and T12 (p < 0.001). The CIA remains constant until 60 years old then decreases significantly passing from a mean value before 20 years old of 82.25° to 73.65° after 70 years old. A statistically significant difference was found between the Arabics and other ethnicities with the formers having an inferior CIA: this was related to a mean older age (p < 0.05) and higher body mass index (p < 0.05) in the Arabics.
Conclusion
The CIA remains constant until 60 years old and then reduces slightly but never under 70°. This angle is helpful to evaluate the lever arm at the upper instrumented vertebra after an adult spinal deformity surgery and could predict the occurrence of a proximal junctional kyphosis when its value is lower than normal. Further clinical studies must confirm this theory.
INTRODUCTION
With the improvements in health care and life expectancy we witness a raise in adult spinal deformity (ASD) incidence with a reported prevalence up to 68% in patients over 60 years [1-4].
When treating ASD, it is mandatory to respect the appropriate sagittal and coronal alignments to have good clinical outcomes and prevent mechanical complications [5-8]. The necessity to keep the head over the pelvis is a fundamental rule firstly supported by Dubousset [5,9]: this means that the cervical spine and the head must be included in the balance analysis.
The principal reported mechanical complication in ASD surgery is proximal junctional kyphosis (PJK) that can affect up to 60% of patients undergoing ASD correction with long or short instrumentations with a consequent high rate of reinterventions [4,10-12]. This complication was first defined by Glattes et al. [13] as a kyphotic angle greater than 10° between the upper instrumented vertebra (UIV) and 2 vertebrae above. Several risk factors have been advocated as responsible for the development of PJK and different attempts have been made to classify this complication to reduce its occurrence [4,10,11,14,15].
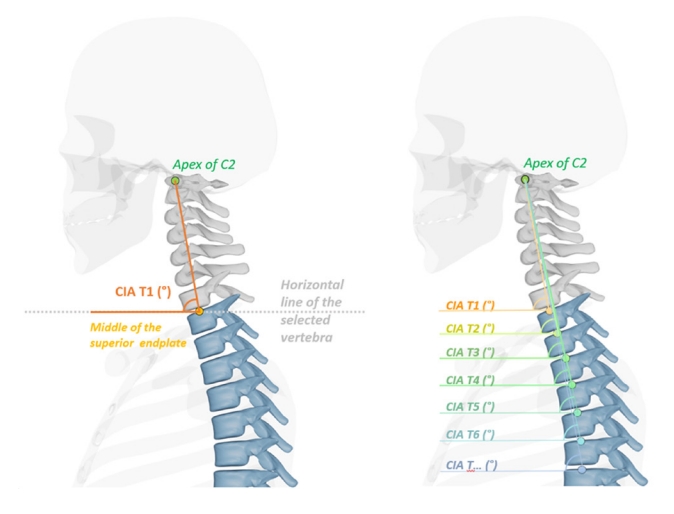
The role of the craniocervical complex (CCC) and the upper thoracic spine has rarely been analyzed and only recently Cerpa et al. [16] have proposed that the posterior skull plumbline anterior to the UIV on postoperative standing x-rays may be a risk factor for PJK. To analyze the role of the CCC on the global spinal alignment and on the risk of PJK, a new angle was proposed: the cervical inclination angle (CIA), defined as an angle between the center of the odontoid, the midpoint of each thoracic vertebra superior endplate and a horizontal line starting from the center of each thoracic vertebra endplate [17,18]. This angle was described to avoid the drawbacks of the C7 sagittal vertical axis which is measured in millimetres and has the inconvenient to be dependant of the length of the spine and the magnification calculation. With the CIA those 2 inconvenient are avoided.
It is known that to maintain an ergonomic sagittal alignment, with less paravertebral muscular effort, the thoracic and cervical spine should be aligned and have small anterior lever arms: each centimetre of anterior displacement of the gravity line results in +3.5 Nm bending moment that raises the risk of vertebral fracture and discal damage [17,18].
The aim of this paper is to confirm the reproducibility of the CIA in an adult asymptomatic population and then to analyze its correlation with the other main sagittal parameters.
MATERIALS AND METHODS
1. Study Population
Asymptomatic adult volunteers between the ages of 18–80 years were enrolled prospectively across 5 different countries/centers (France, Japan, Singapore, Tunisia, and United States) forming the MEANS cohort. The study was approved by all local Institutional Ethics Review Boards for each respective center. Volunteers included in the study reported no significant neck or back pain (visual analogue scale ≤ 2), nor any known spinal disorder(s), and had no history of prior surgical or nonsurgical treatment for a spine related disorder. All volunteers underwent a standing full body or full-spine low-dose stereoradiograph (EOS Imaging, part of ATEC Spine, Inc, Carlsbad, CA, USA) for enrolment in the study. Those with an abnormal vertebral count or transitional anatomy were excluded from the analysis. Following exclusion, a total of 468 patients were included in MEANS. Basic demographic data included age, sex, body mass index (BMI), and ethnicity. Oswestry Disability Index (ODI) scores were also obtained.
2. Radiographic Measurements
All radiographic measurements were performed using a 2D/3D sterEOS modelling software (EOS Imaging). The following sagittal parameters were analyzed for the study: pelvic incidence (PI), pelvic tilt (PT), L1S1 lumbar lordosis (LL), thoracic kyphosis (TK), C7 slope, odontoid-hip axis angle (OD-HA), CIA, and odontoid-thoracic distance (Th-OD) (defined as the distance from the odontoid plumbline and the center of each thoracic vertebra superior endplate). This distance represents the lever arm applied on each vertebral plateau (Fig. 1).
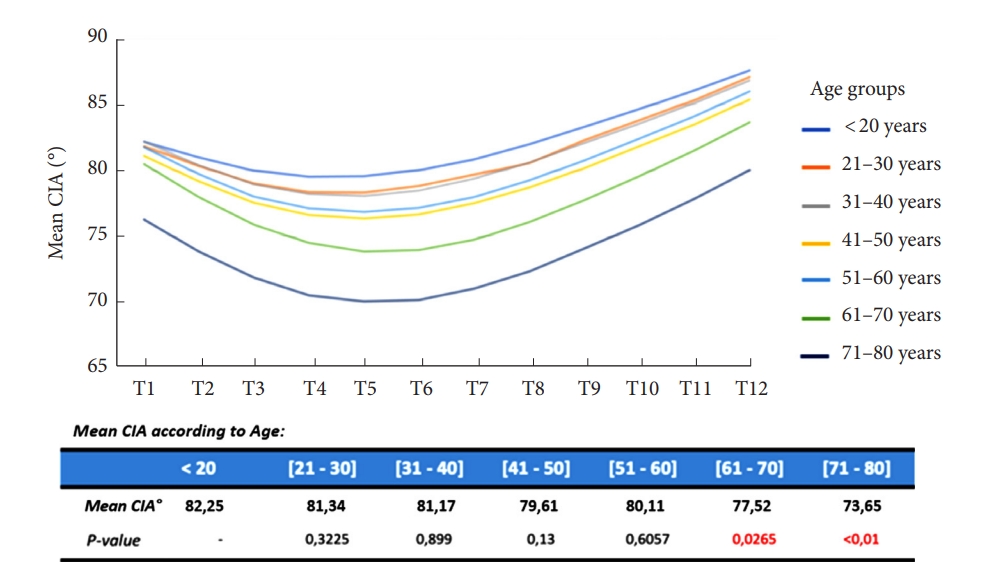
The CIA was first analyzed globally and then in each decade of life (< 20 years [n=12], 21–30 years [n=143], 31–40 years [n=108], 41–50 years [n=94], 51–60 years [n=58], 61–70 years [n=40], 71–80 years [n=19]).
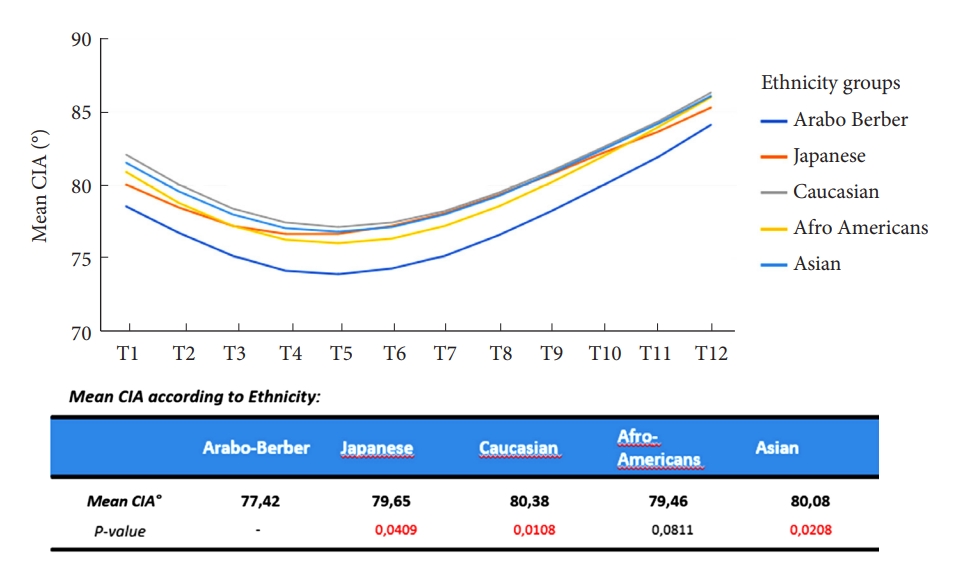
The global population was then divided into 5 different major ethnicities (Caucasian, Japanese, Afro-Americans, Arab-Berber, Asians) and an analysis was performed to identify if the CIA remained constant and reproducible.
The CIA was then analyzed in relation to the BMI and, finally, based on volunteers Roussouly type dividing the population in 3 groups according to the PI value (PI< 45°=Roussouly 1 and 2; PI 45°–60°=Roussouly 3; PI> 60°=Roussouly 4) [19].
3. Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). Categorical variables were expressed as number of cases and percentage. Continuous variables were reported as mean±standard deviation; means were compared with the Student t-test. Two-sided p-values and/or 95% confidence interval (CI) were reported, and significance was accepted at p < 0.05.
Comparisons between different age groups and ethnicities was performed using a t-test and statistical significance was considered with a p < 0.05. Correlations between CIA and BMI, and between CIA and Roussouly type, were performed with a Mann-Whitney test and significance was assessed for a p < 0.05.
Finally, correlations between the CIA and the other major sagittal parameters were assessed with a Pearson correlation coefficient (R: -1 to +1; where -1 identifies a negative correlation while +1 a positive correlation) and significance was assessed for p < 0.05.
RESULTS
Four hundred sixty-eighty adult asymptomatic volunteers were included in the analysis (176 Caucasians, 119 Japanese, 12 Afro-Americans, 80 Arab-Berber, 81 Asians). The mean age was 40,4±14,8 years (95% CI, 39.1–41.7) and the mean BMI was 24.5±5.3 kg/m² (95% CI, 24.0–25.1). The male to female ratio was 184:284. The mean visual analogue score was 0.3±0.5 (95% CI, 0.2–0.3) and the ODI score was 2.2%±4.1% (95% CI, 1.9–2.6).
The global CIA mean value was 80.12°±2.8° (95% CI, 78.28–81.96) with a maximal difference of 9° between all thoracic vertebrae (min T5= 77.05° to max T12= 86.05°, p < 0.001) (Fig. 2).

Graphic of the cervical inclination angle (CIA) value according to the thoracic vertebra. SD, standard deviation.
Of the included volunteers 12 had ≤ 20 years, 142 had 21 to ≤ 30 years, 107 had 31 to ≤ 40 years, 93 had 41 to ≤ 50 years, 57 had 51 to ≤ 60 years, 39 had 61 to ≤ 70 years, and 18 were older than 70 years old. When analyzing the CIA by different decades of life, we observed a significant decrease of the angle after 60 years old: the CIA remains constant until 60 years old (p > 0.05) and then decreases at all thoracic levels passing from 82.25° to 73.65° of mean value (p < 0.05) (Fig. 3).
Considering the ethnicities, a difference was observed between the Arab-Berbers and the other populations. The Arab-Berber had a statistically lower CIA mean value at each thoracic level (p < 0.05) (Fig. 4). It should be highlighted that the Arab-Berber population had an older age (45.48±14.77 years vs. 39.35±14.58 years, p < 0.05) and a higher BMI (27.13±5.23 kg/m² vs. 23.86±5.15 kg/m², p < 0.001) compared to the other populations.
When analyzing CIA in relation to BMI, no statistically significant correlation was observed between these 2 parameters (p = 0.100). Furthermore, Roussouly type (group 1 = PI < 45°, Roussouly 1 and 2; group 2 = PI 45°–60°, Roussouly 3; group 3= PI> 60°, Roussouly 4) did not have an influence on CIA values (group 1 vs. group 2, p = 0.748; group 1 vs. group 3, p = 0.446; group 2 vs. group 3, p = 0.578).
The CIA demonstrated good negative correlations with the Th-OD distance (p < 0.001), the OD-HA angle (p < 0.001), the C7 slope (p < 0.001), the TK (p < 0.001) whereas no or little correlations were observed with the LL, lower LL (L4S1), and the PT (p > 0.05) (Table 1).
DISCUSSION
The goal of an ASD corrective surgery should be a satisfying global sagittal balance so that the patient may have a horizontal gaze and an upright position with the head over the hips [5].
Despite all the efforts made to avoid postoperative mechanical complications, the rate of PJK’s is still very high [4]. Several factors have been advocated as responsible for this event but rarely the effect of an excessive lever arm on the UIV has been discussed [10,11,14]. To analyze this lever arm, the CIA has been proposed with a mean reported value of 77,7° [17].
Here we confirm the reproducibility of this angle with a reported mean value of 80.12°±2.8° and we were able to confirm that the CIA remains constant through different ages, despite BMI and Roussouly type, until 60 years old. When planning an ASD correction, the surgeon should keep this angle in mind and try to restore the sagittal alignment avoiding an excessive lever force on the UIV (CIA≈80°).
The value of the CIA is confirmed by its correlation to other important sagittal parameters. Here we have observed a strong negative correlation with the C7 slope, TK, OD-HA, and ThOD: this means that the increasing value of these parameters correspond to a reduction in the CIA. It is well known that with aging the TK raises due to disc degeneration, vertebral body wedging and reduce paravertebral muscle strength [17]. The increase in TK corresponds to a major C7 slope and to a forward displacement of the trunk with a consequent higher OD-HA angle and higher Th-OD distance [20]. The anterior shift of the trunk raises the bending moment and consequently the risk of a vertebral fracture or PJK [17]. In this scenario an excessive reduction of the CIA at the UIV corresponds to an increased risk of mechanical complications.
We have observed a lower normative value of this angle in the Arabo-Berber population, but as reported previously, this might be influenced by the mean older age in this population. The role of the aging process on the CIA has been demonstrated in this study. Concerning the BMI, it is uncertain if this could directly influence the value of the CIA, especially because we did not find significant correlations between higher body weight and CIA, but high BMI has already been reported as a minor risk factor for PJK [4,21,22].
We are aware that this study has some limitations as it is a descriptive analysis of an adult asymptomatic population and the role of the CIA in prevention of PJK should be confirmed with further clinical investigations. Nevertheless, we have demonstrated the reproducibility of this angle despite age, ethnicities or Roussouly type and its implications in the analysis of the global sagittal balance when planning an ASD correction surgery.
CONCLUSION
The CIA remains constant through ages until 60 years old and then reduces slightly but never under 70°. This angle might be a helpful tool to evaluate the lever arm at UIV on the thoracic spine after an ASD surgery and could predict the occurrence of a PJK when its value is lower than normal. Our experience support this feeling but further clinical studies must confirm this theory.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: JCLH; Data curation: ZMS, EQ, MC, MPK, HWDH, HKW, HR, LGL, SB; Formal analysis: ZMS, EQ, MC, MPK, SB; Methodology: SB; Project administration: JCLH, ZMS, MPK, KH, HWDH, HKW, HR, LGL, SB; Visualization: JCLH, KH, LGL, SB; Writing - original draft: EQ; Writing - review & editing: JCLH.
Acknowledgements
The authors would like to thank Dr. Beatrice Dozin for her assistance in data analysis.