1. Bennett J, M Das J, Emmady PD. Spinal cord injuries. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023.
2. Kang Y, Ding H, Zhou HX, et al. Epidemiology of worldwide spinal cord injury: a literature review. J Neurosurg 2018;6:1-9.


3. van Den Hauwe L, Sundgren PC, Flanders AE. Spinal trauma and spinal cord injury (SCI). In: Hodler J, Kubik-Huch RA, von Schulthess GK, editors. Diseases of the brain, head and neck, spine 2020–2023: diagnostic imaging [Internet]. Cham (CH): Springer; 2020. Chapter 19.
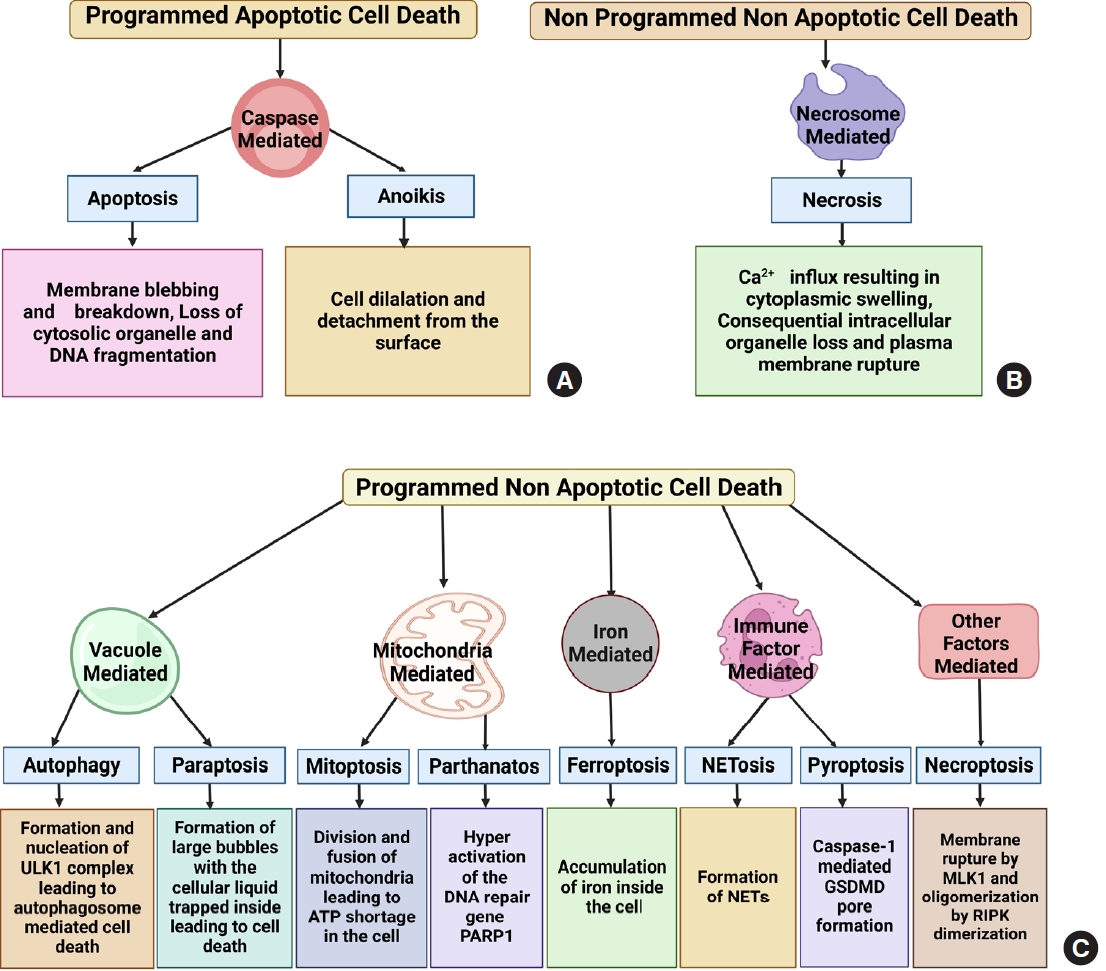
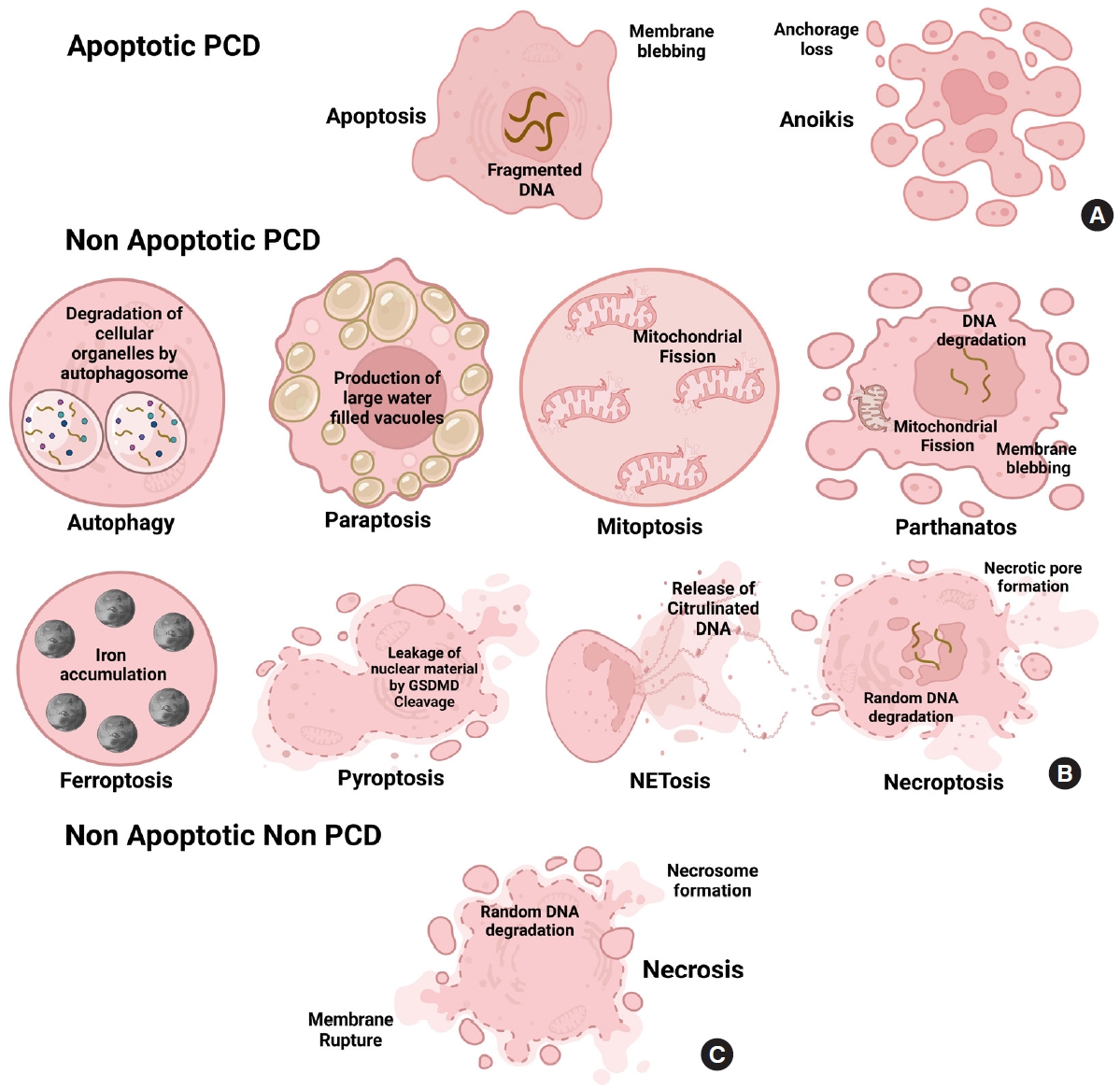
12. Galluzzi L, Vitale I, Aaronson SA, et al. Molecular mechanisms of cell death: recommendations of the Nomenclature Committee on Cell Death 2018. Cell Death Differ 2018;25:486-541.


14. Yan G, Elbadawi M, Efferth T. Multiple cell death modalities and their key features. World Acad Sci J 2020;2:39-48.
17. Vallès M, Mearin F. Pathophysiology of bowel dysfunction in patients with motor incomplete spinal cord injury: comparison with patients with motor complete spinal cord injury. Dis Colon Rectum 2009;52:1589-97.


23. Lu J, Ashwell KW, Waite P. Advances in secondary spinal cord injury: role of apoptosis. Spine (Phila Pa 1976) 2000;25:1859-66.

27. Matassov D, Kagan T, Leblanc J, et al. Measurement of apoptosis by DNA fragmentation. Methods Mol Biol 2004;282:1-17.


28. Zhang N, Yin Y, Xu SJ, et al. Inflammation & apoptosis in spinal cord injury. Indian J Med Res 2012;135:287-96.


29. Yong C, Arnold PM, Zoubine MN, et al. Apoptosis in cellular compartments of rat spinal cord after severe contusion injury. J Neurotrauma 1998;15:459-72.


30. Li GL, Brodin G, Farooque M, et al. Apoptosis and expression of Bcl-2 after compression trauma to rat spinal cord. J Neuropathol Exp Neurol 1996;55:280-9.


33. Emery E, Aldana P, Bunge MB, et al. Apoptosis after traumatic human spinal cord injury. J Neurosurg 1998;89:911-20.


36. Rowland JW, Hawryluk GW, Kwon B, et al. Current status of acute spinal cord injury pathophysiology and emerging therapies: promise on the horizon. Neurosurg Focus 2008;25:E2.

40. Wang Z, Zhou L, Zheng X, et al. Autophagy protects against PI3K/Akt/mTOR-mediated apoptosis of spinal cord neurons after mechanical injury. Neurosci Lett 2017;656:158-64.


42. Beattie MS. Inflammation and apoptosis: linked therapeutic targets in spinal cord injury. Trends Mol Med 2004;10:580-3.


45. Zhang HW, Ding JD, Zhang ZS, et al. Critical role of p38 in spinal cord injury by regulating inflammation and apoptosis in a rat model. Spine (Phila Pa 1976) 2020;45:E355-63.


46. Zhang T, Wang F, Li K, et al. Therapeutic effect of metformin on inflammation and apoptosis after spinal cord injury in rats through the Wnt/β-catenin signaling pathway. Neurosci Lett 2020;739:135440.


48. Abe Y, Yamamoto T, Sugiyama Y, et al. “Anoikis” of oligodendrocytes induced by Wallerian degeneration: ultrastructural observations. J Neurotrauma 2004;21:119-24.


50. Sater AP, Rael LT, Tanner AH, et al. Cell death after traumatic brain injury: detrimental role of anoikis in healing. Clin Chim Acta 2018;482:149-54.


53. Zurita M, Otero L, Aguayo C, et al. Cell therapy for spinal cord repair: optimization of biologic scaffolds for survival and neural differentiation of human bone marrow stromal cells. Cytotherapy 2010;12:522-37.


54. Domogatskaya A, Rodin S, Tryggvason K. Functional diversity of laminins. Annu Rev Cell Dev Biol 2012;28:523-53.


66. Kanno H, Ozawa H, Sekiguchi A, et al. Induction of autophagy and autophagic cell death in damaged neural tissue after acute spinal cord injury in mice. Spine (Phila Pa 1976) 2011;36:E1427-34.


70. Fontana F, Raimondi M, Marzagalli M, et al. The emerging role of paraptosis in tumor cell biology: Perspectives for cancer prevention and therapy with natural compounds. Biochim Biophys Acta Rev Cancer 2020;1873:188338.


71. Wang Y, Wen X, Zhang N, et al. Small-molecule compounds target paraptosis to improve cancer therapy. Biomed Pharmacother 2019;118:109203.


72. Xue J, Li R, Zhao X, et al. Morusin induces paraptosis-like cell death through mitochondrial calcium overload and dysfunction in epithelial ovarian cancer. Chem Biol Interact 2018;283:59-74.


74. Wang WB, Feng LX, Yue QX, et al. Paraptosis accompanied by autophagy and apoptosis was induced by celastrol, a natural compound with influence on proteasome, ER stress and Hsp90. J Cell Physiol 2012;227:2196-206.


76. Pehar M, O’Riordan KJ, Burns-Cusato M, et al. Altered longevity-assurance activity of p53:p44 in the mouse causes memory loss, neurodegeneration and premature death. Aging Cell 2010;9:174-90.


77. Tanabe K, Nakanishi H, Maeda H, et al. A predominant apoptotic death pathway of neuronal PC12 cells induced by activated microglia is displaced by a non-apoptotic death pathway following blockage of caspase-3-dependent cascade. J Biol Chem 1999;274:15725-31.


81. Nara A, Aki T, Funakoshi T, et al. Methamphetamine induces macropinocytosis in differentiated SH-SY5Y human neuroblastoma cells. Brain Res 2010;1352:1-10.


82. Lyamzaev KG, Nepryakhina OK, Saprunova VB, et al. Novel mechanism of elimination of malfunctioning mitochondria (mitoptosis): formation of mitoptotic bodies and extrusion of mitochondrial material from the cell. Biochim Biophys Acta 2008;1777:817-25.


85. Arnoult D, Rismanchi N, Grodet A, et al. Bax/Bak-dependent release of DDP/TIMM8a promotes Drp1-mediated mitochondrial fission and mitoptosis during programmed cell death. Curr Biol 2005;15:2112-8.


87. Wingrave JM, Schaecher KE, Sribnick EA, et al. Early induction of secondary injury factors causing activation of calpain and mitochondria-mediated neuronal apoptosis following spinal cord injury in rats. J Neurosci Res 2003;73:95-104.


91. Yu SW, Wang H, Poitras MF, et al. Mediation of poly(ADPribose) polymerase-1-dependent cell death by apoptosisinducing factor. Science 2002;297:259-63.


94. Yang D, Shu T, Zhao H, et al. Knockdown of macrophage migration inhibitory factor (MIF), a novel target to protect neurons from parthanatos induced by simulated post-spinal cord injury oxidative stress. Biochem Biophys Res Commun 2020;523:719-25.


96. Wang X, Ge P. Parthanatos in the pathogenesis of nervous system diseases. Neuroscience 2020;449:241-50.


100. Nasrabady SE, Kuzhandaivel A, Nistri A. Studies of locomotor network neuroprotection by the selective poly(ADPribose) polymerase-1 inhibitor PJ-34 against excitotoxic injury to the rat spinal cord in vitro. Eur J Neurosci 2011;33:2216-27.


102. Muthaiah VPK, Michael FM, Palaniappan T, et al. JNK1 and JNK3 play a significant role in both neuronal apoptosis and necrosis. Evaluation based on in vitro approach using tert-butylhydroperoxide induced oxidative stress in neuro-2A cells and perturbation through 3-aminobenzamide. Toxicol In Vitro 2017;41:168-78.


108. Zhou H, Yin C, Zhang Z, et al. Proanthocyanidin promotes functional recovery of spinal cord injury via inhibiting ferroptosis. J Chem Neuroanat 2020;107:101807.


111. Enge TG, Ecroyd H, Jolley DF, et al. Longitudinal assessment of metal concentrations and copper isotope ratios in the G93A SOD1 mouse model of amyotrophic lateral sclerosis. Metallomics 2017;9:161-74.


115. Masuda S, Nakazawa D, Shida H, et al. NETosis markers: quest for specific, objective, and quantitative markers. Clin Chim Acta 2016;459:89-93.


116. Vande Walle L, Lamkanfi M. Pyroptosis. Curr Biol 2016;26:R568-72.


119. Li R, Zhang LM, Sun WB. Erythropoietin rescues primary rat cortical neurons from pyroptosis and apoptosis via Erk1/2-Nrf2/Bach1 signal pathway. Brain Res Bull 2017;130:236-44.

126. Sollberger G, Choidas A, Burn GL, et al. Gasdermin D plays a vital role in the generation of neutrophil extracellular traps. Sci Immunol 2018;3:eaar6689.


131. Yap YW, Whiteman M, Cheung NS. Chlorinative stress: an under appreciated mediator of neurodegeneration? Cell Signal 2007;19:219-28.


132. Kubota K, Saiwai H, Kumamaru H, et al. Myeloperoxidase exacerbates secondary injury by generating highly reactive oxygen species and mediating neutrophil recruitment in experimental spinal cord injury. Spine (Phila Pa 1976) 2012;37:1363-9.


136. Sun L, Wang H, Wang Z, et al. Mixed lineage kinase domain-like protein mediates necrosis signaling downstream of RIP3 kinase. Cell 2012;148:213-27.


139. Andera L. Signaling activated by the death receptors of the TNFR family. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2009;153:173-80.


141. Wang Y, Wang H, Tao Y, et al. Necroptosis inhibitor necrostatin-1 promotes cell protection and physiological function in traumatic spinal cord injury. Neuroscience 2014;266:91-101.


142. Fan H, Tang HB, Kang J, et al. Involvement of endoplasmic reticulum stress in the necroptosis of microglia/macrophages after spinal cord injury. Neuroscience 2015;311:362-73.


147. Wang Z, Jiang H, Chen S, et al. The mitochondrial phosphatase PGAM5 functions at the convergence point of multiple necrotic death pathways. Cell 2012;148:228-43.


149. Sims NR, Muyderman H. Mitochondria, oxidative metabolism and cell death in stroke. Biochim Biophys Acta 2010;1802:80-91.


154. Jalalvand E, Robertson B, Tostivint H, et al. The spinal cord has an intrinsic system for the control of pH. Curr Biol 2016;26:1346-51.


155. Zhu S, Liu J, Kang R, et al. Targeting NF-κB-dependent alkaliptosis for the treatment of venetoclax-resistant acute myeloid leukemia cells. Biochem Biophys Res Commun 2021;562:55-61.


156. Jamison JM, Gilloteaux J, Taper HS, et al. Autoschizis: a novel cell death. Biochem Pharmacol 2002;63:1773-83.


158. Weerasinghe P, Buja LM. Oncosis: an important non-apoptotic mode of cell death. Exp Mol Pathol 2012;93:302-8.


161. Syntichaki P, Tavernarakis N. Death by necrosis. Uncontrollable catastrophe, or is there order behind the chaos? EMBO Rep 2002;3:604-9.


162. Martin LJ. Neuronal cell death in nervous system development, disease, and injury (Review). Int J Mol Med 2001;7:455-78.


163. Beattie MS, Hermann GE, Rogers RC, et al. Cell death in models of spinal cord injury. Prog Brain Res 2002;137:37-47.

166. Chen KB, Uchida K, Nakajima H, et al. Tumor necrosis factor-α antagonist reduces apoptosis of neurons and oligodendroglia in rat spinal cord injury. Spine (Phila Pa 1976) 2011;36:1350-8.


167. Martin LJ, Al-Abdulla NA, Brambrink AM, et al. Neurodegeneration in excitotoxicity, global cerebral ischemia, and target deprivation: a perspective on the contributions of apoptosis and necrosis. Brain Res Bull 1998;46:281-309.


168. Tator CH. Update on the pathophysiology and pathology of acute spinal cord injury. Brain Pathol 1995;5:407-13.