Perioperative Clinical Features and Long-term Prognosis After Oblique Lateral Interbody Fusion (OLIF), OLIF With Anterolateral Screw Fixation, or OLIF With Percutaneous Pedicle Fixation: A Comprehensive Treatment Strategy for Patients With Lumbar Degenerative Disease
Article information
Abstract
Objective
To compare the efficacy of oblique lateral interbody fusion (OLIF), OLIF combined with anterolateral screw fixation (OLIF-AF), and OLIF combined with percutaneous pedicle screw fixation (OLIF-PF) in the treatment of single-level or 2-level degenerative lumbar disease.
Methods
Between January 2017 and 2021, 71 patients were treated with OLIF and combined OLIF. The demographic data, clinical outcomes, radiographic outcomes, and complications were compared among the 3 groups.
Results
The operative time and intraoperative blood loss in the OLIF (p<0.05) and OLIF-AF (p<0.05) groups were lower than in the OLIF-PF group. Posterior disk height improvement in the OLIF-PF group was better than in the OLIF (p<0.05) and OLIF-AF (p<0.05) groups. In terms of foraminal height (FH), the OLIF-PF group was significantly better than the OLIF group (p<0.05), but there was no significant difference between the OLIF-PF and OLIF-AF groups (p>0.05) or between the OLIF and OLIF-AF groups (p>0.05). There were no significant differences in fusion rates, the incidence of complications, lumbar lordosis, anterior disc height, and cross-sectional area among the 3 groups (p>0.05). The OLIF-PF group had significantly lower rates of subsidence than the OLIF group (p<0.05).
Conclusion
OLIF remains a viable option with similar patient-reported outcomes and fusion rates compared with surgeries that include lateral and posterior internal fixation while greatly reducing the financial burden, intraoperative time, and intraoperative blood loss. OLIF has a higher subsidence rate than lateral and posterior internal fixation, but most subsidence is mild and has no adverse effect on clinical and radiographic outcomes.
INTRODUCTION
Lumbar fusion has been widely used in treating lumbar degenerative diseases. Oblique lateral interbody fusion (OLIF), an anterior, minimally invasive lumbar fusion, has received widespread attention in clinical practice [1-3].
He et al. [4] suggested that OLIF and OLIF with percutaneous pedicle screw fixation (OLIF-PF) have equivalent clinical and radiographic outcomes and similar complication rates. Guo et al. [5] reported that OLIF with anterolateral screw fixation (OLIF-AF) had the same Oswestry Disability Index (ODI) score, imaging findings, and complication rates as OLIF-PF in the treatment of single-segment lumbar degenerative disease.
Current literature [4-7], due to small sample sizes, heterogeneity of research objectives, short follow-up times, and low levels of evidence, is insufficient to determine whether OLIF or combined methods are superior. Thus, it is difficult for clinicians to choose the most appropriate method. In this study, which to our knowledge is the first to include OLIF, OLIF-AF, and OLIF-PF as comparison groups, we evaluate the clinical and radiographic outcomes of OLIF and OLIF-AF and OLIF-PF and analyze the differences among the 3 groups from multiple perspectives to provide recommendations on choosing the most appropriate approach in clinical practice.
MATERIALS AND METHODS
This study was reviewed and approved by the ethics committee of the Beijing Xuanwu Hospital (approval number: [2022]020) with waiver of informed consent from patients given that its retrospective nature. From January 2017 to January 2021, 71 patients were enrolled in this retrospective study, including 25 in the OLIF group, 19 in the OLIF-AF group, and 27 in the OLIF-PF group. Inclusion criteria were: (1) ≤ 2 surgical levels; (2) with the following one or more diseases: the degree I or II lumbar spondylolisthesis, lumbar degenerative disc herniation, lumbar spinal stenosis, and degenerative lumbar scoliosis. Exclusion criteria were: with complicated lumbar tumor, lumbar tuberculosis or other infectious diseases, and a history of previous lumbar surgery (Fig. 1).

Flow diagram of the study selection and follow-up process. OLIF, oblique lateral interbody fusion; OLIF-AF, OLIF combined with anterolateral screw fixation; OLIF-PF, OLIF combined with percutaneous pedicle screw fixation; CT, computed tomography; MRI, magnetic resonance imaging.
1. Surgical Technique
The patient was positioned on their right side. Their arms were placed in a 90°/90° position, and their lower limbs were protected by padding and fastened with a band. C-arm fluoroscopy was used to locate the surgical segment. The localization line was marked on the body surface. We will describe the lumbar 4/5 segment operation as an example. After general anesthesia, the patient was placed in the right lateral decubitus position. The right lower limb was straightened, the left lower limb was flexed, the hips and knees were bent, and the psoas major muscles were relaxed. After fixation, the C-arm located and marked the lumbar 4/5 space. A longitudinal incision of approximately 5cm was made at the midpoint of the lumbar 4/5 gap. The subcutaneous skin tissue was cut, and the fascia of the external oblique muscle was cut. The deep internal oblique muscle and transverse abdominis muscle were bluntly separated along the direction of the muscle fiber. Outside the peritoneum, the abdominal organs were ventrally pulled and the psoas major muscles were dorsally pulled, exposing the vertebral body laterally.
C-arm fluoroscopy was used to locate the lumbar 4/5 space, cut the annulus fibrosus, remove the nucleus pulposus, release the intervertebral space, treat the endplate cartilage with reamer and various scrapers, and cut the contralateral annulus fibrosus. The test mold was placed and inserted diagonally into the intervertebral space gradually, vertically, and completely. After fluoroscopy, aspirated autologous bone marrow blood from the iliac crest was mixed with the allograft and bone morphogenetic proteins to pack in a cage of appropriate size for implantation into the intervertebral space. When fluoroscopy showed that the cage was centered, the intervertebral space was spread, the physiological lordosis was restored, and slippage was reduced. Intraoperatively, antibiotic saline was repeatedly rinsed, bipolar electrocoagulation was used to completely stop bleeding, and layer-by-layer sutures were completed. For patients who underwent anterolateral screw fixation, there was no need to change the position of the vertebrae. Using C-arm fluoroscopy, the screw was inserted along the surgical approach. Patients who underwent posterior percutaneous pedicle screw fixation were repositioned to the prone position, and the screws were implanted according to routine procedures, followed by C-arm fluoroscopy of the screw position.
2. Clinical Indicators
Relevant descriptive information such as age, body mass index, operative time, intraoperative blood loss, postoperative hospital stay, complications, and operative stage, was collected and analyzed. The visual analogue scale (VAS) and the ODI were used for preoperative, postoperative, and final follow-up. The final follow-up was at least 12 months after surgery. At this visit, computed tomography (CT) was used to assess pedicle screw position and fusion rate and to measure Hounsfield units. A combination of CT and magnetic resonance imaging (MRI) was used to assess the degree of decompression.
3. Imaging Parameter Measurement
All patients underwent lumbar x-ray, CT, and MRI at preoperative, postoperative, and final follow-up (Fig. 2). The sagittal angle of lumbar lordosis (LL) was measured by x-ray in the Picture Archiving Communication System (Fig. 3). Foraminal height (FH), cross-sectional area of the intervertebral foramina (CSAF), anterior disc height (ADH), and posterior disc height (PDH) were measured on the CT sagittal view (Fig. 4). The cross-sectional area (CSA) of the spinal canal was measured in the axial sections of T2-weighted imaging (Fig. 5). The degree of subsidence was graded using the grading system reported by Marchi et al. [8], where grades 0 and I were referred to as low-grade and grades II and III as the high-grade subsidence.
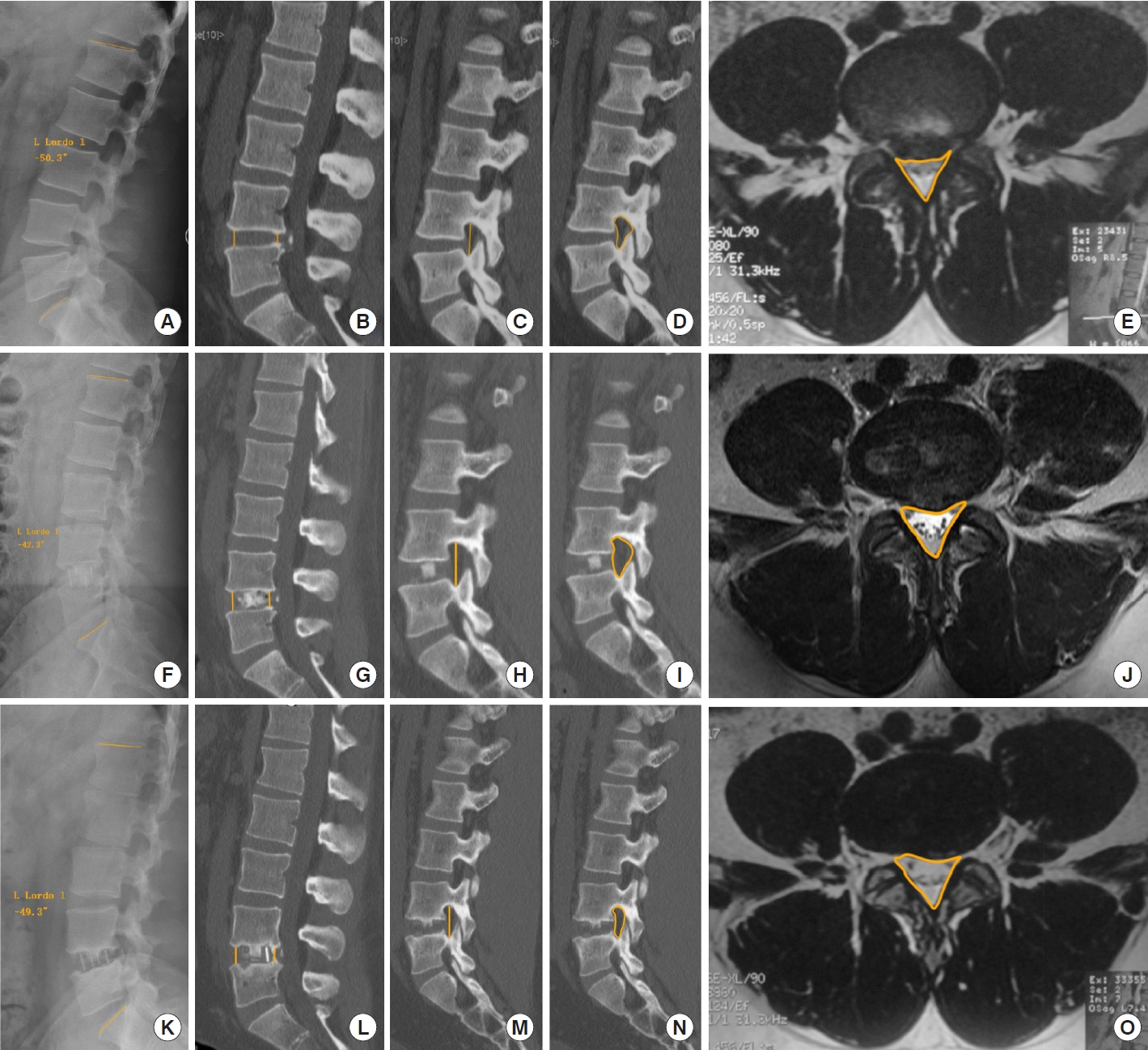
Radiographic evaluation. Measurement of cross-sectional area (CSA), anterior disk height (ADH), posterior disc height (PDH), foraminal height (FH), lumbar lordosis (LL), and the cross-sectional area of the intervertebral foramina (CSAF). Measurements of CSA, ADH, PDH, FH, and CSAF in the Picture Archiving Communication System (PACS) before the operation, at postoperative 1 day, and at last follow-up (A, F, and K). LL was measured in x-ray sagittal position, the head end measurement line was placed on the L1 superior end plate, the tail end measurement line was placed on the S1 superior end plate (B, G, and L). ADH and PDH were measured at the sagittal position in computed tomography (CT), the distance between the anterior/posterior edges of the upper vertebrae and the end plate of the lower vertebrae is called the anterior/posterior disk height (C, H, and M). FH was measured in the sagittal planes of the bilateral foramen in CT images. The length between the upper and lower edges is FH (D, I, and N). In the same plane of computed tomography CT, the foramen was outlined to read the CSAF (E, J, and O). CSA was measured in the axial sections of T2-weighted imaging. The central canal (including the thecal sac and epidural fat) was outlined in PACS to get the CSA.

The x-ray presentation in an operative patient. (A–C) The patient underwent OLIF. (D–F) The patient underwent OLIF-AF. (G–I) The patient underwent OLIF-PF. Three groups in x-ray before the operation, at postoperative 1 day, and at last follow-up.

The computed tomography (CT) presentation in an operative patient. (A–C) The patient underwent OLIF. (D–F) The patient underwent OLIF-AF. (G–I) The patient underwent OLIF-PF. Three groups in CT before the operation, at postoperative 1 day, and at last follow-up. OLIF, oblique lateral interbody fusion; OLIF-AF, OLIF combined with anterolateral screw fixation; OLIF-PF, OLIF combined with percutaneous pedicle screw fixation.

The magnetic resonance imaging (MRI) presentation in an operative patient. (A–C) The patient underwent OLIF. (D–F) The patient underwent OLIF-AF. (G–I) The patient underwent OLIF-PF. Three groups in MRI before the operation, at postoperative 1 day, and at last follow-up. The yellow arrow points to the sagittal segment corresponding to the axial MRI image.OLIF, oblique lateral interbody fusion; OLIF-AF, OLIF combined with anterolateral screw fixation; OLIF-PF, OLIF combined with percutaneous pedicle screw fixation.
4. Statistical Analysis
The normal distribution of parameters was compared between the 2 groups using a t-test and expressed as mean± standard deviation, while 1-way analysis of variance was employed for comparing the data among multiple groups. If there was a statistically significant difference between the groups, a post hoc comparison was performed using Bonferroni correction. Parametrics with nonnormal distribution were statistically described by the median. The Mann-Whitney U-test was used for assessing data between the 2 groups, and for multiple groups, the Kruskal-Wallis H-test was used. If the difference between the groups was statistically significant, a post hoc comparison was performed using Bonferroni correction. Categorical data were represented by frequency. The chi-square test or Fisher exact test was used to compare data between the 2 or more groups. If the differences between the groups were statistically significant, the chi-square test or Fisher exact test was further used for multiple comparisons, and the corresponding p-value was corrected using Bonferroni correction. Multivariate analysis was performed using linear regression for linear variables and logistic analysis for categorical variables. Baseline variables that were considered clinically relevant or that showed a univariate relationship with outcome were included in multivariate analysis [9]. Statistical analysis was performed using IBM SPSS Statistics ver. 24.0 (IBM Co., Armonk, NY, USA).
RESULTS
1. Demographic Data
The demographics data of the patients was shown in Table 1. A total of 71 patients (48 women and 23 men) were enrolled in the study, and the mean patient age was 64.8± 10.6 years (range, 34–88 years). 51 cases had at least 12 months of follow-up, 12 cases had at least 24 months of follow-up, and 8 cases had at least 36 months of follow-up.
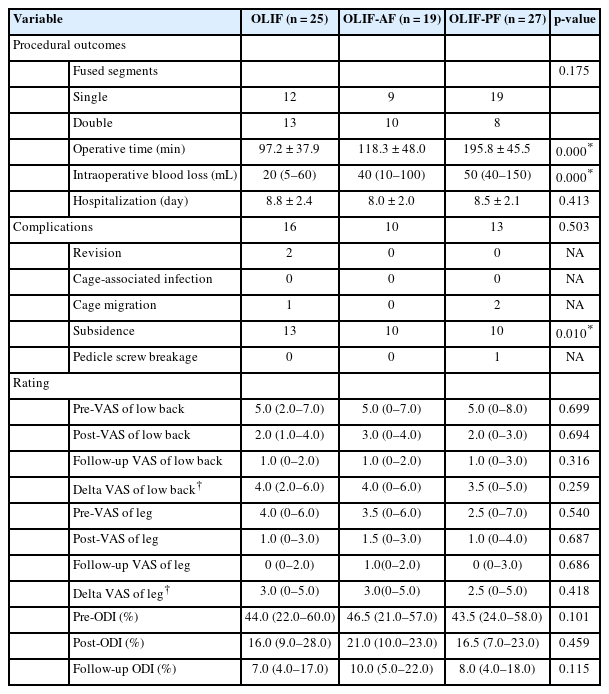
2. Clinical Outcomes
Forty patients underwent single-level surgery, and 31 patients underwent double-level surgery; the operation time of the OLIF group (p< 0.05) and OLIF-AF group (p< 0.05) was shorter than that of the OLIF-PF group. The intraoperative blood loss in the OLIF group (p< 0.05) and OLIF-AF group (p< 0.05) was also less than that in the OLIF-PF group. The OLIF, OLIF-AF, and OLIF-PF groups showed no significant difference in VAS and ODI scores (p> 0.05), recorded preoperatively, 1 week postoperatively, and final follow-up, respectively (Table 2).
3. Radiographic Outcomes
There was no significant difference in preoperative and postoperative ADH, PDH, FH, the CSAF, and CSA, LL among the OLIF, OLIF-AF, and OLIF-PF groups (p> 0.05). During followup, the improvement of PDH in the OLIF-PF group was superior to that in the OLIF (p< 0.05) and OLIF-AF groups (p< 0.05) (Table 3). In terms of FH, the OLIF-PF group was significantly better than the OLIF group (p< 0.05), but there was no statistical difference between the OLIF-PF group and the OLIF-AF group (p> 0.05) or between the OLIF group and the OLIF-AF group (p > 0.05). In the improvement of CSAF, the OLIF-PF group (p< 0.05) and OLIF-AF group (p< 0.05) were better than the OLIF group. There were 38 surgical segments in the OLIF group and 32 achieved bony fusion, with a fusion rate of 84.2% (32 of 38); 29 surgical segments in the OLIF-AF group involving 25 cases of bony fusion at a fusion rate of 86.2% (25 of 29), and a total of 35 segments were operated in the OLIF-PF group, of which 33 achieved bony fusion, with a fusion rate of 94.3% (33 of 35). There were no significant differences in fusion rates among the OLIF, OLIF-AF, and OLIF-PF groups (p> 0.05).
4. Complications
There were no vascular, ureteral, lumbar plexus, sympathetic nerve, abdominal organ injuries, or other serious complications in the 3 groups. There were 38 surgical segments in the OLIF group including 25 segments showing subsidence. Of which, 68% (17 of 25) patients had grades 0–I and 32% (8 of 25) cases exhibited grades II–III subsidence. There were 29 surgical segments in the OLIF-AF group, and a total of 13 segments showed subsidence. Of which, 70% (9 of 13) cases reported grades 0–I, and 30% (4 of 13) presented grade II. A total of 35 segments were operated in the OLIF-PF group, and a total of 11 segments showed subsidence with grades 0–I. In the subsidence rates, OLIF-PF was superior to the OLIF group (p< 0.05), and there was no significant difference between the OLIF and OLIF-AF groups (p > 0.05), or the OLIF-AF and OLIF-PF groups (p > 0.05). One patient who underwent OLIF was found to have cage displacement 2 weeks postoperatively without symptoms and was treated with posterior percutaneous pedicle screw fixation. Two patients who underwent OLIF-PF had cage displacement, but they were asymptomatic and did not receive treatment. One patient with OLIF-PF was found to have screw fractures at their final follow-up visit, but they were asymptomatic and required no treatment.
5. Subgroup Analysis
We conducted subgroup analysis based on numbers of fused surgical segments (single vs. double) (Supplementary Table 1), gender (male vs. female) (Supplementary Table 2), and age (≤ 65 years old vs. > 65 years old) (Supplementary Table 3). However, there was no significant prognostic difference in these subgroups, which indicating the operation of OLIF, OLIF-AF, and OLIF-PF may have similar prognostic outcomes, regardless of numbers of fused surgical segments, gender, and age.
6. Multivariate Regression Analysis
Univariate analysis was explored to evaluate improvement of clinical outcomes (Supplementary Table 4) and radiographic outcomes (Table 4). We found that age, gender, numbers of fused surgical segments, and bone mineral density did not show statistically significant differences in clinical outcomes and radiological outcomes, and the choice of internal fixation did not show statistically significant differences in the improvement of clinical outcomes, but the choice of posterior internal fixation was significantly better than OLIF in terms of avoiding subsidence in the radiological outcomes (p< 0.05). Using multivariate analysis, compared with the OLIF group, the risk of subsidence in the OLIF-PF group was lower (odds ratio, 0.272; 95% confidence interval, 0.082–0.904; p< 0.05). In the other words, the choice of posterior internal fixation was an independent protective factor in terms of avoiding subsidence (Table 5), while there were no factors independently associated with clinical outcomes (Supplementary Table 5).
DISCUSSION
With the development of the OLIF technique, OLIF and OLIF combined with internal fixation have been widely used and have achieved satisfactory results (Table 6) [4,6,7,10-18]. Nevertheless, research comparing the advantages of OLIF and OLIF combined with different internal fixations is urgently needed. To our knowledge, this is the first retrospective study to date which evaluate outcomes in the OLIF, OLIF-AF, and OLIF-PF. In our study, we used a multivariate analysis to investigate the effects of age, gender, and single or double surgical level on clinical and radiological outcomes. In addition, the follow-up time in this study is longer than that reported in similar literature.
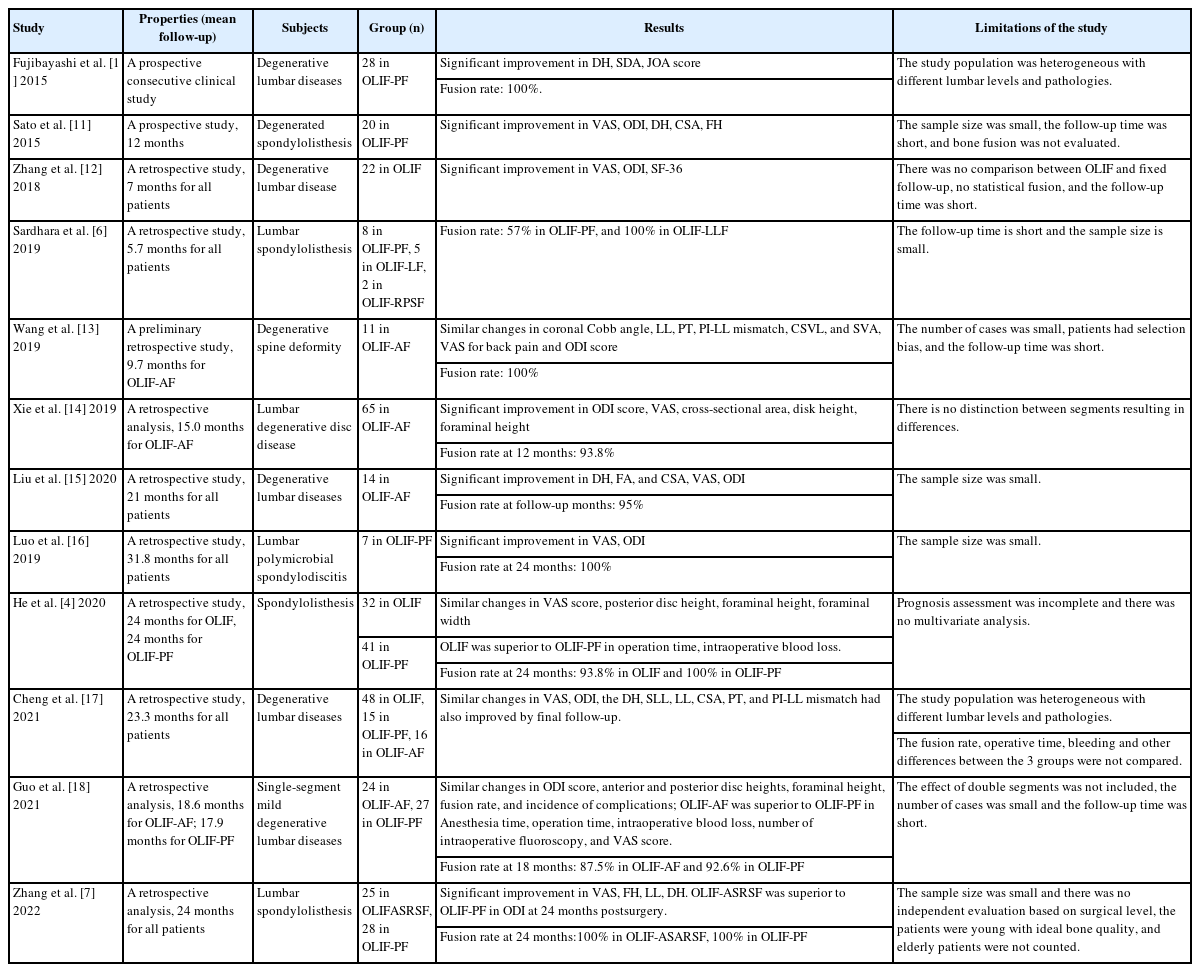
Literatures review of the clinical and radiologic outcomes of OLIF compared other lumbar interbody fusion
Our study found that the OLIF group and OLIF-AF group outperformed the OLIF-PF group in terms of shorter operation duration and less intraoperative blood loss. Similar findings have been reported in the previous studies [5,19]. Because patients in the OLIF-PF group must be adjusted from the lateral position to the prone position, the surgical procedure is longer. Without the need for a change in position or an extra incision, the OLIF-AF group's total operation time and blood loss were reduced. Because of enhanced recovery after surgery, there was no significant difference in the length of hospital stays across the 3 groups.
In our study, low-grade subsidence was observed in all 3 groups but high-grade subsidence was only observed in the OLIF group. By implanting an interbody fusion device, OLIF can restore the height of the intervertebral space, achieve indirect decompression, and alleviate neurological symptoms [20]. Subsidence, on the other hand, may impede the effects of indirect decompression by restoring disc height and result in discomfort, nonfusion, and other negative effects. In OLIF, the problem of the loss of interbody height brought on by fusion subsidence cannot be avoided [21,22]. Subsidence has been demonstrated to be a significant predictor of revision after OLIF [23]. Pitzen et al. [24] show that the use of posterior fixation can boost axial compressive strength, which lowers the likelihood of subsidence. According to Ge et al. [19], additional lateral plate fixation is ineffective at preventing subsidence. In this study, we found that posterior internal fixation is superior to lateral fixation in avoiding subsidence, and lateral fixation outperforms OLIF alone, which is consistent with the findings of Guo et al. [5] and He et al. [4].
We found that the fusion rate of OLIF-PF was better than that of OLIF-AF and OLIF, but not significantly so. This indicates that OLIF-PF may be superior at fostering fusion and maintaining intervertebral stability. We suggest that posterior percutaneous pedicle screw internal fixation can effectively maintain the stability of the 3 columns, restrict flexion and extension of the operative segment, distribute the stress of the fusion device, and establish a stable external environment for bone graft fusion [23]. The lateral screw also promotes fusion and lowers the likelihood of subsidence because it can greatly lessen the stress on the fusion device, even if it is not as effective as the posterior bilateral pedicle screw [18].
In the present study, we found improvements in VAS and ODI after surgery and at follow-up in all 3 groups, while there were no statistically significant differences in ODI and VAS scores between groups. We hypothesize that the recurrence of symptoms after OLIF is due to excessive loss of reconstructed intervertebral height caused by subsidence. Intervertebral fusion may prevent the occurrence of these symptoms. Recent studies have also shown that fusion is associated with better clinical outcomes [25,26]. In all 3 groups, the fusion rate rose as time passed after surgery, which led to an improvement in symptoms.
Although OLIF has the advantage of indirect decompression fusion and causes little damage to the posterior anatomical structure of the lumbar spine, the risk of injury to abdominal organs, great vessels, psoas major muscle, and lumbar plexus nerve from this approach cannot be ignored [10,27,28]. However, in our cohort, there were no serious complications, and there was no statistically significant difference in the probability of complications among the 3 groups.
This study has a few limitations. Firstly, our sample size is small, which may affect the statistical analysis. Second, some patients who met the inclusion criteria were lost to follow-up. Third, this is a retrospective study with no long-term follow-up results, so we hope to conduct a large, prospective randomized control trial with long-term follow-up to conduct a more comprehensive evaluation. Finally, we currently consider OLIF for patients without osteoporosis, without isthmic lysis, spondylolisthesis ≤ Meyerding grade I and fusion segment ≤ 2. Otherwise, we prefer to use supplement fixation. In our experienced, sometimes we need to choose posterior fixation instead of anterior construct due to limited space/bleeding during the approach. However, since this study was retrospective, not all patients followed this selection criterion for the choice of internal fixation.
CONCLUSION
For 2 or fewer surgical levels, we believe that OLIF remains a viable option. This technique has similar patient-reported outcomes and fusion rates as compared with the addition of lateral and posterior instrumentation, while it also substantially reduces the patient's financial burden, intraoperative time, and intraoperative blood loss. The subsidence rate of OLIF is higher than that of lateral and posterior internal fixation, but most of the subsidence is mild and has no adverse effects on clinical and radiographic outcomes. The long-term effects still need to be evaluated via long-term follow-up in a large number of cases.
SUPPLEMENTARY MATERIALS
Supplementary Tables 1-5 can be found via https://doi.org/10.14245/ns.2244954.477.
Subgroup analysis of prognosis in patients with single/double fused segment
Subgroup analysis of prognosis in male and female patients
Subgroup analysis of prognosis in elderly patients
Univariate analysis of clinical outcomes
Multivariate linear regression analysis of clinical outcomes
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: ZL; Data curation: XZ; Formal analysis: YW, WZ, KW; Methodology: HW; Project administration: HW, SL; Writing - original draft: XZ; Writing - review & editing: KW.