The Posterior Cranial Vertical Line: A Novel Radiographic Marker for Classifying Global Sagittal Alignment
Article information
Abstract
Objective
To define a novel radiographic measurement, the posterior cranial vertical line (PCVL), in an asymptomatic adult population to better understand global sagittal alignment.
Methods
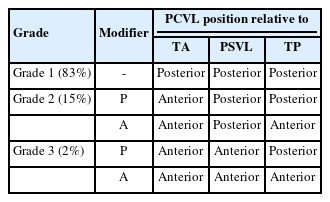
We performed a multicenter retrospective review of prospectively collected radiographic data on asymptomatic volunteers aged 20–79. The PCVL is a vertical plumb line drawn from the posterior-most aspect of the occiput. The horizontal distances of the PCVL to the thoracic apex (TA), posterior sagittal vertical line (PSVL, posterosuperior endplate of S1), femoral head center, and tibial plafond were measured. Classification was either grade 1 (PCVL posterior to TA and PSVL), grade 2 (PCVL anterior to TA and posterior to PSVL), or grade 3 (PCVL anterior to TA and PSVL).
Results
Three hundred thirty-four asymptomatic patients were evaluated with a mean age of 41 years. Eighty-three percent of subjects were PCVL grade 1, 15% were grade 2, and 3% were grade 3. Increasing PCVL grade was associated with increased age (p < 0.001), C7–S1 sagittal vertical axis (SVA) (p < 0.001), C2–7 SVA (p < 0.001). Additionally, it was associated with decreased SS (p = 0.045), increased PT (p < 0.001), and increased knee flexion (p < 0.001).
Conclusion
The PCVL is a radiographic marker of global sagittal alignment that is simple to implement and interpret. Increasing PCVL grade was significantly associated with expected changes and compensatory mechanisms in the aging population. Most importantly, it incorporates cervical alignment parameters such as C2–7 SVA. The PCVL defines global sagittal alignment in adult volunteers and naturally distributes into 3 grades, with only 3% being grade 3 where the PCVL lies anterior to the TA and PSVL.
INTRODUCTION
Achieving an upright posture and appropriate spinal balance requires a dynamic alignment between the head, spine, pelvis and lower extremities [1-5]. This is critical as malalignment in the sagittal plane has been correlated with poor functional status and patient outcomes [4,6-9]. However, achieving proper alignment of all these structures during spinal deformity surgery can be challenging for a multitude of reasons, including the lack of a global measure for spinal sagittal alignment.
When examining the spine, establishing a “normal” set of comprehensive spinal measurements has been elusive given the vast variation within asymptomatic individuals [2,10,11]. One fundamental aspect of an ergonomic posture that remains critical in all healthy individuals is the proper alignment of the spine with respect to the body’s center of mass [12-15]. The gravity line (GL) remains an important measure of global spinal alignment in theory. The GL is obtained using a force plate on which the bipedal subject is standing. Traditionally, the C7 plumb line (C7PL) has been used as a radiographic proxy for the GL and as a means of estimating sagittal alignment [16-19]. However, multiple studies have demonstrated there is discordance between these 2 measures, reducing the predictive value of the C7PL [20-22]. Given the shortcomings of the C7PL, and the inconvenience of establishing the true GL (i.e., via digital force plate), there exists a need for another measurement that can better approximate global sagittal alignment. By understanding the relative position of the head, spine, pelvis and lower extremities, surgeons will be better equipped to evaluate adult spinal deformity (ASD).
The purpose of this study is to define the posterior cranial vertical line (PCVL) as a potential marker for global spine alignment. The PCVL is a novel radiographic measurement which incorporates skull position as well as lower extremity position, which is frequently overlooked in other measurements. By comparison, the standard C7–S1 sagittal vertical axis (SVA) is a focal measurement of spinal balance from the C7 vertebral body down to the sacrum. Using the PCVL may provide a more complete picture of a patient’s global alignment and have important implications in preoperative planning and patient prognosis.
MATERIALS AND METHODS
Prospectively collected standing, full-length bi-planar radiographs were retrospectively reviewed for 334 asymptomatic adult volunteers ages 20–79 years old. Radiographs were obtained using imaging with 3-dimensional capabilities (EOS Imaging, Paris, France) with the patient in a relaxed position, with fingers resting on the clavicles – no further instructions were given in order to preserve physiologic stance. Patients were excluded if they had any history of back or neck pain requiring time off from work/school or affecting daily activity; history of prior hip or knee arthroplasty, lower extremity realignment surgery or any spine surgery; coronal deformity (Cobb angle > 10°); any degenerative or pathologic spinal conditions (requiring intervention); pregnancy; nonambulatory patients; or patients with history or neuromuscular disorder, inflammatory arthritis, or congenital anomalies. Age, sex, body mass index (BMI), Oswestry Disability Index (ODI), and Neck Disability Index (NDI) were collected for each patient included. This study was approved by the Institutional Review Board of Washington University in St. Louis (201812144) and all volunteers provided informed consent.
Patients were excluded if full-standing radiographs did not clearly visualize the posterior-most aspect of the skull, thoracic apex (TA), or the tibial plafond (TP). Cervical measurements obtained included C2–7 lordosis (measured from inferior endplate of C2 to inferior endplate of C7) and C2–7 SVA (distance from C2 midbody plumbline to posterosuperior corner of C7). Thoracic measurements obtained included T1 slope (angle formed by superior endplate T1 and a horizontal reference line), T4–12 kyphosis (measured from superior endplate of T4 to inferior endplate of T12), and apex of thoracic kyphosis (TA). Spinopelvic measurements obtained included sacral slope, pelvic tilt, pelvic incidence (PI), L1–S1 lumbar lordosis (LL), PI–LL mismatch, and the C7–S1 SVA (distance from C7 midbody plumbline to posterosuperior corner of S1).
The PCVL was defined as a vertical plumb line from the posterior-most aspect of the occiput to the floor. The horizontal distances of the PCVL to the TA, posterior sagittal vertical line (PSVL; vertical line drawn superiorly from posterosuperior endplate of S1), the femoral head (FH) center, and center of the TP were measured. Each patient was then classified as either grade 1 (PCVL posterior to the TA and the PSVL), grade 2 (PCVL anterior to TA and posterior to the PSVL), or grade 3 (PCVL anterior to both the TA and the PSVL) (Fig. 1, Table 1). Grade 2 and 3 patients with a PCVL posterior to the center of the TP were given a “P” modifier; those with a PCVL anterior to the TP were given an “A” modifier (Table 1). All measurements were performed by a team of fellows and residents. A standardized protocol was created and written visual instructions were provided to every contributor. Individual measurements were reviewed throughout the cohort to assess interrater relatability using Cronbach alpha values, which exceeded 0.8 for all measures. Chi-square tests and analysis of variance were performed for bivariate analyses using SAS Studio Versions 3.4 (SAS Institute Inc., Cary, NC, USA).
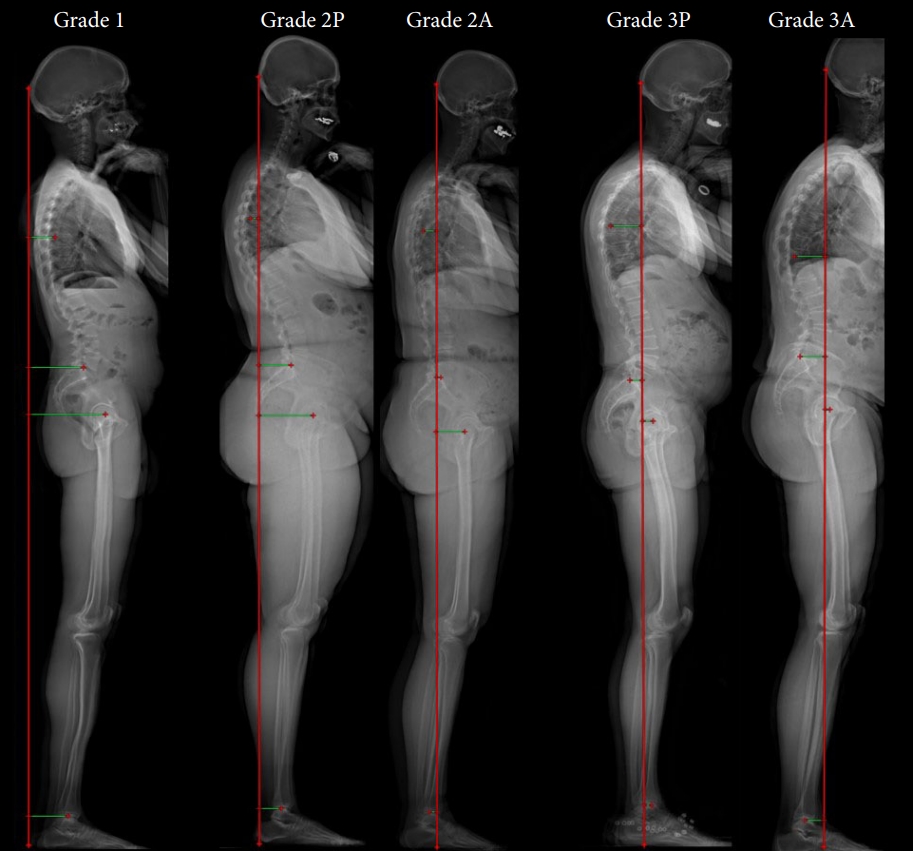
The posterior cranial vertical line (PCVL) grading system. Grade 1: The PCVL lies posterior to the thoracic apex (TA) and posterior sagittal vertical line (PSVL). Grade 2: The PCVL lies posterior anterior to the TA and posterior to the PSVL. Grade 3: The PCVL lies anterior to both the TA and PSVL. The “A” and “P” modifiers refer to the PCVL position relative to the center of the tibial plafond in grades 2 and 3.
RESULTS
Our study included a total of 334 asymptomatic volunteers, 64% of whom were female. Average age was 41±14 years and average BMI was 24.4 kg/m2. The average ODI score was 2.7±4.4 (Table 2). When measuring the relative position of the PCVL to various reference points, negative values were used to indicate a relatively posterior PCVL position, while a positive value indicated a relatively anterior PCVL position. Average PCVL–PSVL distance was -7.4 cm and average PCVL–TA distance was -2.1 cm. Average PCVL–FH distance was -10.8 cm and average PCVL–TP distance was -5.4 cm. Eighty-three percent of subjects were grade 1, 15% were grade 2, and 2% were grade 3. Overall, 98% of normal subjects were either grade 1 or grade 2.
Higher PCVL grade had a significant association with increasing age (p<0.001). The mean age in grade 1 patients was 39.6 years, grade 2 was 45.6 years, and grade 3 was 63 years. Fig. 2 illustrates the age distribution of the asymptomatic cohort demonstrating an increase in age throughout the PCVL grades. Higher PCVL grade was also significantly associated with increasing greater T1 slope (p < 0.001), greater T4–12 kyphosis (p<0.001), greater cervical lordosis (p=0.006), greater pelvic tilt (p<0.001), and increased knee flexion (p<0.001) (Table 2). Conversely, higher PCVL grade was associated with decreased sacral slope (p=0.045). Higher PCVL grade was associated with a larger C7–S1 SVA (p<0.001) and C2–7 SVA (p<0.001) (Table 2). Of note, PI remained similar between PCVL grades as expected. A strong positive correlation (coefficient ≥ 0.6) was seen with C2–7 SVA and greater T1 slope, while a moderate correlation (coefficient ≥ 0.4) was seen with C7–S1 SVA and T4–12 thoracic kyphosis. Similarly, a PCVL anterior to the TP was strongly correlated with greater C7–S1 SVA (p < 0.001), C2–7 SVA (p<0.001), T1 slope (p<0.001) (Table 2).
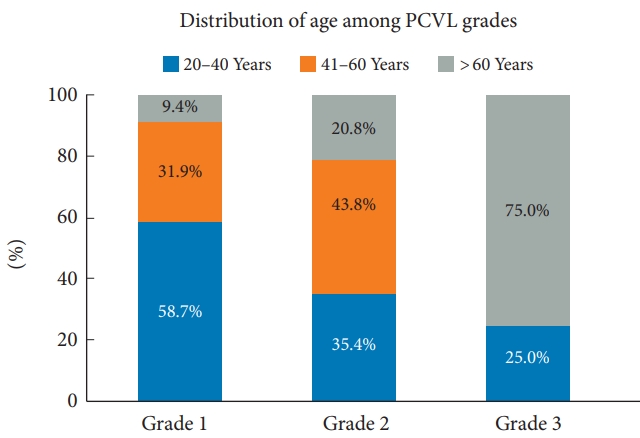
Distribution of age among the posterior cranial vertical line (PCVL) grades. Grade 1: The PCVL lies posterior to the thoracic apex (TA) and posterior sagittal vertical line (PSVL). Grade 2: The PCVL lies posterior anterior to the TA and posterior to the PSVL. Grade 3: The PCVL lies anterior to both the TA and PSVL.
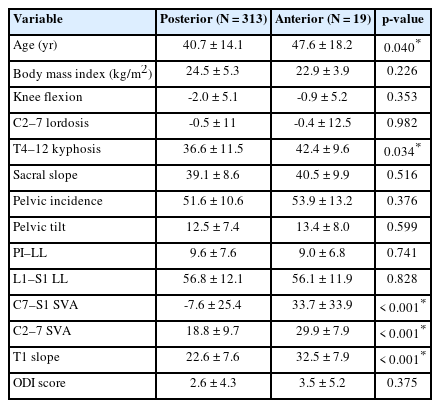
When the population was subdivided using the TP modifier (anterior vs. posterior position of the PCVL relative to TP), similar results were seen with the anterior modifier and increasing PCVL grade. An anterior modifier had significant association with age (p=0.04) as well as increased C7–S1 SVA, increased C2–7 SVA, as well as increased T1 slope (p<0.001) (Table 3).
DISCUSSION
Dubousset first described “the cone of economy” decades ago—the upright posture of the human body that minimizes energy expenditure [23]. As sagittal alignment increases, energy expenditure increases as well to remain upright and maintain horizontal gaze. Compensation through the lumbar spine and pelvis occurs through pelvic retroversion—as lumbar lordosis decreases, PT increases and SS decreases [24]. In addition, there is an active, dynamic component maintaining this optimal position termed the chain of balance [15]. This complex anatomic relationship between the spine and pelvis has been well described by Roussouly et al. [25,26] as well, and the importance of sagittal spinal alignment in patient-reported outcomes has been well established previously [4,6-9].
The current widely accepted radiographic measurement for sagittal alignment, the C7–S1 SVA, has been considered the strongest predictor of improved outcomes in patients with ASD [4,22,27]. Lafage et al. [28] showed an SVA > 50 mm or PT > 20° were associated with worse outcomes scores. In a normal population, Gelb et al. [17] found the mean SVA to be -3.2±3.2 cm. The C7–S1 SVA, however, fails to the position of the skull and alignment of the cervical spine, as well as compensation through the lower extremities.
Various studies have shown that age-related changes and increasing positive sagittal alignment leads to compensatory knee flexion and subsequent hip extension [29-32]. Age-related changes have also been described in the cervical spine showing increasing C2–7 lordosis in order to maintain horizontal gaze [33,34]. These changes were also shown in a prior publication performed on a subset of the healthy volunteer radiographs used in this study [35]. Given these other compensatory mechanisms, it is not surprising that the focal C7–S1 SVA measurement is discordant with the gold standard GL (obtained using a force plate) [20-22].
The goal of our study was to develop a simple, practical radiographic measurement that could take into consideration all aspects of global sagittal alignment. A prior study by Kim et al. [36] attempted to address this issue with the cranial SVA, requiring a measurement from the midpoint of the nasion-inion line, from the root of the nose to the external occipital protuberance. While this did address skull position, we hoped to improve on this concept with a simple, practical radiographic marker that was easier to measure and reproduce reliably, with an organic anatomic grading system in the asymptomatic population. The PCVL requires a single vertical line drawn from the posterior-most aspect of the occiput down to the floor. In our study, the vast majority of healthy volunteers examined (98%) had a PCVL posterior to the PSVL (grades 1 and 2), with 83% of patients having a PCVL posterior to both the PSVL and TA (grade 1).
Aside from linear measurements such as the C7–S1 SVA, angular measurements have also been proposed to characterize global sagittal alignment. The cervicothoracic pelvic angle (CTPA), introduced by Protopsaltis et al. [37] in 2017, is defined as the angle formed between a line from C2 midvertebral body to the FH center and a line from T1 midvertebral body to the FH center. The CTPA has been shown to be associated with the development of proximal junctional kyphosis (PJK) postoperatively [37]. This is similar to the previously described T1PA, which is defined as the angle formed between a line from the T1 midvertebral body and the FH center to a line from the midpoint of the S1 superior endplate to the FH center [38]. T1PA has been shown to correlate with health-related quality of life for ASD patients [38].
In our study, we found that the PCVL grade does strongly correlate with the current gold standard C7–S1 SVA. In addition, we found that greater PCVL grade was significantly associated with expected compensatory changes over time such as increasing PI–LL, decreasing SS, increasing PT, increasing T1 slope. Regarding the skull and lower extremity position, the higher PCVL grade was significantly associated with expected compensatory increasing C2–7 lordosis, greater C2–7 SVA, as well as with increased knee flexion. In fact, C2–7 SVA and T1 slope both had a strong correlation (coefficient ≥ 0.6) with increasing PCVL grade. Based on our results, we hypothesize that the PCVL grade is an accurate reflection of global positive sagittal alignment, and as seen with prior sagittal measures that a higher PCVL grade may be associated with higher risk of PJK following a fusion procedure. The next step in this study would be to measure the PCVL in ASD patients preoperatively and postoperatively while tracking patient-reported outcome measures as well as radiographic evidence of PJK postoperatively.
When interpreting the results of this study, it is important to consider its limitations. First, the generalizability of the asymptomatic volunteers used in this study and whether they represent a true normal distribution of humanity upon which to base a new classification system may be brought into question. However, this cohort of asymptomatic volunteers is one of the largest collection of volunteers with full-standing radiographs across a wide variety of ages and ethnic backgrounds which we believe is a powerful tool in understanding a normative population. Secondly, the use of the PCVL requires radiographs to be obtained via imaging with 3-dimensional capabilities (EOS Imaging) which may not be available to every institution. Nonetheless, we believe that full-standing radiographs will be the new gold standard moving forward. Thus, this measure is crucial to further characterizing sagittal alignment with additional information provided by both the position of the skull as well as the lower extremities. Thirdly, the conducted study focuses on establishing a classification to patients with no spinal pathologies which may question if the proposed measurements correlate with the disease process. It is important to note that the purpose of this study is to establish a baseline distribution in the asymptomatic population in order to first characterize the measurement. Thus, the aforementioned relationship will be assessed in a subsequent study on its application in the ASD population.
CONCLUSION
We present the PCVL as a novel singular sagittal alignment marker that may play a helpful role in understanding global sagittal alignment. The PCVL is easy to implement and allows for immediate visualization of skull position relative to the thoracic spine, sacrum, as well as the TPs that is simple to interpret. Our population showed that a majority of asymptomatic volunteers were grade 1 (83%), while 17% of patients were grade 2 or 3 with a PCVL anterior to the TA. We propose here a simple grading system that may have the potential to aid in preoperative planning to correct sagittal malalignment, as well as assess patients postoperatively over time.
Notes
Conflict of Interest
EOS imaging supported the multicentric collaborative group by providing the 3D parameters for the MEANS cohort and a web-based solution for image review. Authors, or their institutions did not receive any funding from EOS imaging relative to this work.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: PJP, ZMS, MPK, SB, KH, HKW, HWDH, HR, JCLH, LGL; Formal Analysis: PJP, FMH, MC; Investigation: LGL; Methodology: PJP, XEF, FMH, CM, NJL; Project Administration: FMH; Writing – Original Draft: PJP, XEF, FMH, CM, NJL, MC; Writing – Review & Editing: PJP, FMH, ZMS, MPK, SB, KH, HKW, HWDH, HR, JCLH, LGL.