Saving Stabilizing Structure Treatment With Bilateral-Contralateral Decompression for Spinal Stenosis in Degenerative Spondylolisthesis Using Unilateral Biportal Endoscopy
Article information
Abstract
Objective
This study aimed to evaluate the treatment of spinal stenosis with spondylolisthesis using bilateral-contralateral unilateral biportal endoscopic (UBE) decompression to minimize facet joint damage.
Methods
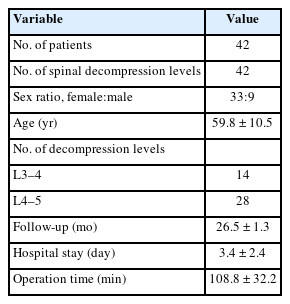
We retrospectively evaluated 42 patients with grade 1 spondylolisthesis who underwent bilateral-contralateral UBE decompression between July 2018 and September 2019. To identify segmental instability, static and dynamic images from preoperative and postoperative procedures and final follow-up radiographs were reviewed. Lateral radiograph slippage ratio, sagittal motion, and facet joint preservation were evaluated. Clinical assessments were conducted using the visual analogue scale (VAS), Oswestry Disability Index (ODI), and modified MacNab criteria.
Results
The average final follow-up period was 26.5 ± 1.3 months. The average preoperative slip percentage was 15.70% ± 5.25%, which worsened to 18.80% ± 5.41% at the final follow-up (p < 0.005). The facet joint preservation rate was 95.6% ± 4.1% on the contralateral side. Improvements in the VAS scores (leg pain: from 7.9 ± 2.2 to 3.1 ± 0.7; p < 0.005; back pain: from 7.2 ± 3.0 to 2.8 ± 1.0; p < 0.005) were observed at the final follow-up. The mean preoperative ODI was 26.19 ± 3.42, which improved to 9.6 ± 1.0 (p < 0.005). Thirteen patients exhibited delayed focal segmental instability following decompression. Despite the absence of symptoms or improvement with conservative treatment in the majority of patients with delayed instability, two patients required fusion surgery to address the instability. Additionally, 2 patients developed facet synovial cysts, while 2 experienced spinous process fractures.
Conclusion
Bilateral decompression with a contralateral UBE approach could be an effective and alternative treatment method to reduce instability in spinal stenosis with grade 1 spondylolisthesis.
INTRODUCTION
Patients with degenerative spondylolisthesis, a condition that greatly influences older people and most commonly affects the lower lumbar spine [1], generally have symptoms of back and/or lower extremity pain and neurological deficits. Although conservative treatments, such as anti-inflammatory drug use and physical therapy, can help alleviate the pain caused by degenerative spondylolisthesis, back and/or leg pain persists in many patients and may require surgical treatment to ameliorate it, stabilize the spine, and improve body function. Spinal fusion remains the gold standard for the surgical care of degenerative spondylolisthesis, particularly in the presence of spinal instability.
Dynamic radiographic research has proven that most patients with degenerative spondylolisthesis do not have spinal instability, and that their symptoms are primarily due to spinal nerve root compression or stimulation of inflamed nerve root. Open spinal decompression, with or without fusion, is generally performed in these patients. In particular, surgical processes involving fusion are traumatic, require general anesthesia, have a long recovery period, and are frequently associated with a high incidence complications and elevated costs [2].
Minimally invasive surgical methods, such as unilateral biportal endoscopic (UBE) decompression that targets the paingenerating area, have recently been revised with the goal of reducing fusion, resulting in improved clinical outcomes and increased patient satisfaction [3-7]. Nevertheless, despite the continuous development of surgical processes using spinal endoscopic and related equipment, issues such as iatrogenic instability caused by facet joint involvement remain [8].
In the ipsilateral approach, the medial facet joint is unavoidably exposed at the surgical site. The facet joint is less involved on the contralateral side than on the ipsilateral side when unilateral laminotomy bilateral lumbar decompression is performed [9,10]. In particular, invasion of the facet structure is minimized during contralateral decompression when using endoscopic decompression (Fig. 1A, B) [11,12]. However, there have been no reports on bilateral-contralateral decompression in patients with spinal stenosis in degenerative spondylolisthesis who require minimal facet joint damage. In such cases, the operator approaches the left side to decompress the right side and vice versa. Thus, we performed bilateral-contralateral decompressions on both sides to minimize damage to the facet joint for the treatment of spinal stenosis with spondylolisthesis via UBE (Fig. 1C).

Differences in facet invasion (blue circle) between the ipsilateral (A) and contralateral approaches (B). Opposite decompression on both sides were performed using a bilateralcontralateral approach for spondylolisthesis with spinal stenosis via unilateral biportal endoscopic (C).
A key consideration is that the safety and effectiveness of this method in the treatment of patients with degenerative spondylolisthesis has not been completely established. This retrospective study aimed to describe in detail how this approach can be applied safely and effectively to treat patients with grade 1 degenerative spondylolisthesis, summarize our experiences, identify technical obstacles, and present the surgical outcomes of spondylolisthesis treatment.
MATERIALS AND METHODS
1. Patient Selection
This retrospective study included 42 consecutive patients who were treated using bilateral-contralateral UBE techniques between July 2018 and September 2019. All patients were diagnosed with grade 1 lumbar spondylolisthesis according to the Meyerding classification system [13], and had lumbar stenosis and neurogenic claudication with or without lumbar radiculopathy [14]. Diagnosis was made using standard lumbar anteroposterior and lateral radiographs (degree of spondylolisthesis of ≥ 3 mm).
Symptoms such as lasting radicular leg pain, neurological deficits, or neurogenic intermittent claudication refractory-to-preservation treatment for ≥ 6 months caused by moderate-to-severe spinal canal stenosis with lateral recess stenosis were considered indications for surgery. Based on the magnetic resonance imaging (MRI) grading system for lumbar foraminal stenosis [15], patients with grade 3 severe foraminal stenosis and complete loss of fat and/or neuromuscular morphological changes were excluded. Patients with pre-existing degenerative scoliosis with a Cobb angle of > 20°, degenerative spondylolisthesis greater than or equal to grade 2 in the Meyerding classification system, segmental instability (i.e., translation of angular movement of > 4 mm or 10° between flexion and extension on upright lateral radiographs), a history of prior lumbar spine surgery, or < 20 or > 80 years of age were excluded from the study. During the same period, fusion was performed on 26 patients with spondylolisthesis who required surgery that did not correspond to the bilateral-contralateral UBE decompression indication. Three neurosurgeons centrally examined each patient’s radiographic and MRI findings to confirm degenerative lumbar canal stenosis with spondylolisthesis without disc herniation.
All the included patients underwent bilateral-contralateral UBE decompression. A facet-sparing procedure was performed in all cases. Data access and use were approved by the Institutional Review Board (IRB No. 2022-W04) of the Leon Wiltse Memorial Hospital, Suwon. Preapproval was not necessary for the use of the data in this study as it included anonymous secondary data published for research purposes.
2. Surgical Technique
After placing the patients under general anesthesia, they were positioned with their abdomen free on the radiolucent Relton-Hall framework. The skin and surgical field were arranged using the standard method. Bilateral-contralateral UBE decompression was performed with ongoing general saline irrigation, a waterproof final layer of draping, and a smooth drainage system for saline outflow.
These preservation techniques were necessary to protect patients from hypothermia caused by immersion in the cold saline solution. The fluoroscope was arranged parallel to the disc space to obtain accurate anteroposterior images. The spinal levels of interest were indicated on the skin using a biplanar fluoroscope. Four small incisions penetrating the deep fascia were required for bilateral-contralateral UBE decompression. Two skin incisions are generally made along the medial pedicle line, separated by 2–3 cm, using the left approach (Figs. 2, 3A). Serial dilators (≤ 10 mm) are used to divide the paraspinal muscles, enlarge the instrument portal, and gently remove the soft tissues from the interlaminar space. A narrow gap was created by the inflow of normal saline. The overall surgical process was conducted in a precise and expanded surgical field using meticulous hemostasis (Fig. 4). By modifying the inflow of hydrostatic pressure and managing the outflow, hemostatic disruptions such as bleeding from small epidural veins and oozing from bones could be observed. A radiofrequency wand was used for proper cauterization of bleeding from soft tissues and larger epidural veins (ArthroCare, Austin, TX, USA). Bone wax was also used to prevent severe bleeding. Decompression from the spinolaminar junction was performed using an electric highspeed diamond bur, 3 or 4 mm in diameter (Primado 2; NSK, Fukushima, Japan). The decompression steps were as follows (Fig. 4):
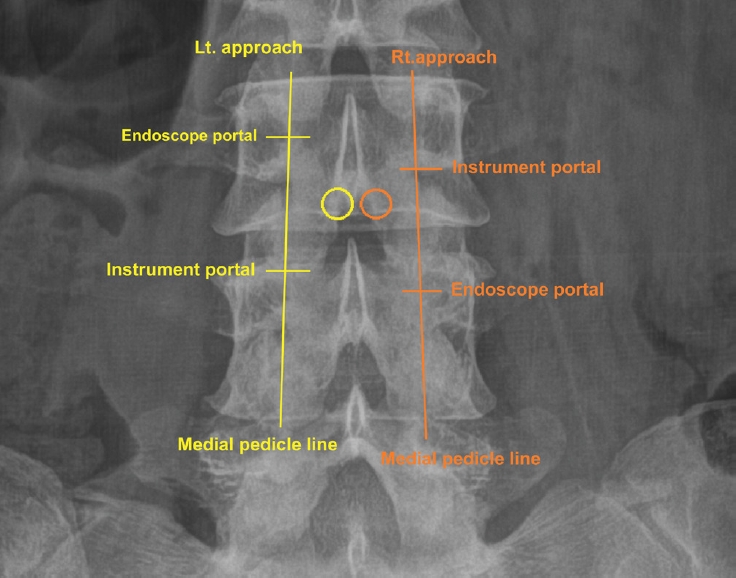
The circle indicates the initial targeting area: the spinolaminar junction. Skin incisions are made along the medial pedicle line, separated by 2–3 cm. Lt., left; Rt., right.

(A) Decompressing the right side by approaching through the left side. (B) Decompressing the left side by approaching through the right. Dual monitors allow the operator to go to the contralateral side and immediately start decompression.

Unilateral biportal endoscopic decompression is performed with left-side access using a 0° arthroscope. (A) The spinolaminar junction is the starting point for decompression. (B) The origin of the ligamentum flavum is detached (*), and the base of the spinous process is removed using a high-speed diamond bur. (C) Decompression of the contralateral lateral recess (right decompression via left-side approach). (D) Decompression of the contralateral lateral recess (left decompression via right-side approach). Lt, left; Rt, right.
(1) The ipsilateral lamina was drilled, starting cranially at its lower edge; the origin of the ligamentum flavum and underlying epidural fat became visible, as shown in Fig. 4A.
(2) The underside of the contralateral lamina was drilled to approach the lateral recess. The ligamentum flavum was preserved to protect the underlying neural tissues. Hypertrophic and deformed facets of joints are usually observed during severe stenosis. More bone was removed from the base of the spinous process to widen the laminotomy window and provide easier access to the contralateral lateral recess (Fig. 4B).
(3) Extract the contralateral half of the ligamentum flavum and decompress the lower side of the contralateral facet joint to release the contralateral traversing nerve root (Fig. 4C).
(4) To facilitate reentry from the right side, move the UBE tower to the opposite side. The surgeon should also position themselves on the right side of the patient and perform contralateral left decompression using the right approach. By utilizing dual monitors (Fig. 3B), the surgeon can switch to the other side without relocating the instruments and begin the contralateral approach, thereby reducing time. It is advisable to approach the right side approximately 5 mm lower than the conventional approach to prevent excessive laminectomy of the lamina caused by the right hand getting caught on the lamina (Fig. 2).
(5) The Freer Elevator (Endovision, Seoul, Korea) can be used to locate the pre-existing left laminectomy site and access the epidural area. Perform laminectomy only on the portion trapped in the right lamina and conduct contralateral decompression using the same method as before (Fig. 4D).
(6) Supplementary Fig. 1 shows pre- and postoperative image.
3. Radiographic Measurements
To identify segmental instability, static and dynamic images from the preoperative and postoperative procedures and final follow-up radiographs were reviewed. The Taillard method [16] was used to measure the slippage ratio of lateral radiographs, and the sagittal motion in spondylolisthesis was estimated based on the difference in the slippage of the flexion-extension points. Preoperative computed tomography (CT) images were used to measure disc height, facet angle, and Pathria grading scales, as previously demonstrated [17]. Supplementary Fig. 2 shows how the measurements were performed. MRI studies of the lumbar spine were conducted over 2 days during the preoperative and postoperative periods. The method described by Dohzono et al. [18] was used to evaluate facet joint preservation; however, MRI was performed instead of CT (Supplementary Fig. 3). For the mean value, each measurement was repeated 3 times by the 3 spine surgeon investigators (DHL, DGL, and JWJ).
4. Clinical Outcomes
Clinical results were assessed based on the visual analogue scale (VAS) for back pain and lower leg symptoms, while the Oswestry Disability Index (ODI) and MacNab criteria were used to evaluate the degree of disability and medical care results, respectively. Assessments were conducted during the preoperative, postoperative, and final follow-up periods. In the case of complications, medical charts were carefully examined. Operation time and length of hospital stay were also included.
5. Statistical Analyses
IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA) was used for all statistical analyses. Medical outcomes and radiological changes after surgery were assessed using Wilcoxon signed-rank tests. The Mann-Whitney U-test was used to compare changes in the slippage ratio at the final follow-up between patients with and without spinal instability. Statistical significance was set at p< 0.05. Intraclass correlation coefficient analysis was used to assess the interobserver reliability to validate the assessed data.
RESULTS
A total of 42 patients (9 men and 33 women) were included in the study. All patients underwent single-level decompression with grade 1 spondylolisthesis, with L4–5 affected in 28 patients and L3–4 in 14 patients. The patients’ average age was 60 years (range, 48–76 years), and the clinical and radiological final follow-up period was 26.5 ± 1.3 months (range, 24–29 months). The average slip percentage before surgery was 15.70%± 5.25%, which worsened and increased to 18.80%± 5.41% at the final follow-up (p< 0.005; Supplementary Fig. 4). Thirteen patients showed delayed instability and increased slip percentage from 12.75%± 2.34% to 18.98%± 2.77% (p< 0.005). Slip percentage increased from 17.09% ± 5.78% to 18.83 ± 6.44% in the stable group of 29 patients (p< 0.005). There was a statistically significant increase in slipping in the delayed instability group (p < 0.005). The percentage of facet joint preservation was 95.6%± 4.1% on the contralateral approach. There was no statistically significant difference in the facet Pathria grade.
The operation time was 108.8± 32.2 minutes (range, 92–150 minutes). The average volume of blood loss during surgery and on postoperative day 1 was 60.1± 20.2 mL. The average duration of hospital stay was 3.4±2.4 days (range, 3–6 days). On postoperative day 1, most patients were able to ambulate. The demographic data are presented in Table 1. Multivariate forward selection stepwise logistic regression analysis of the factors that could cause instability after decompression in spondylolisthesis (disc height, facet angle, and spondylolisthesis movement) revealed p= 0.312, p= 0.932, and p= 0.137, respectively (Table 2). After surgery, the patients showed a significant improvement in their symptoms. The VAS scores for leg and back pain decreased from 7.9±2.2 to 3.1±0.7 (p<0.005) and from 7.2±3.0 to 2.8±1.0 (p< 0.005), respectively, at the final follow-up. The mean preoperative ODI was 26.19 ± 3.42, which improved to 9.6 ± 1.0 (p< 0.005) at the final follow-up.

Multivariate analysis using forward selection stepwise logistic regression in patients with lumbar spondylolisthesis
According to the modified MacNab criteria, the final results were excellent in 26 patients (61.9%), good in 12 (28.6%), fair in 2 (4.8%), and poor in 2 (4.8%). Overall, 90.0% of patients had good or excellent outcomes. A few surgical complications were identified, including delayed focal segmental instability after decompression in 13 patients. Although no symptoms or relief with conservative treatment was noted, 2 patients underwent fusion surgery due to instability. A facet synovial cyst developed in 2 patients, although it was asymptomatic and disappeared within the follow-up period. Two patients had a spinous process fracture. No complications associated with infections or wounds were observed. Mild complications were reported, although none of the patients experienced worsening of symptoms.
DISCUSSION
The pathological prevalence of degenerative spondylolisthesis varies depending on the population and measurement method used to evaluate it. A large population-based study of patients aged > 65 years in China revealed that degenerative spondylolisthesis showed a higher preponderance in female patients, with a prevalence of 25.0% in women and 19.1% in men [19]. Despite improvements in spinal endoscopic surgical steps owing to the development of relevant equipment in recent decades, certain problems, such as iatrogenic instability caused by the violation of the facet joints, remain to be solved [8]. For sufficient exposure of the surgical field using the ipsilateral method, the encroachment of the facet is unavoidable. According to a previous report, the facet joints on the contralateral part were violated to a lesser degree than those on the ipsilateral section in unilateral laminotomy bilateral lumbar decompression [9], and the percentage reduction of the joint area undergoing the ipsilateral method was 22.6%. Based on that report, fractures in the inferior articular process accounted for 6% of cases treated using the ipsilateral approach. A high risk of facet joint damage in decompression has been reported for patients with an upper lumbar level lesion, a narrow lamina, and sagittal plane joint morphology [20]. A contralateral endoscopic method developed to reduce iatrogenic instability caused by laminectomy with violation of the facet joints has shown good medical and surgical results [11,12,21,22]. Based on this, we performed bilateral-contralateral UBE decompression in spinal stenosis with grade 1 spondylolisthesis and obtained good clinical results.
Our radiological outcomes showed that the percentage reduction of the facet joint plane was 4.4% after using the contralateral method, which was lower than the previously reported percentages of facet joint decrease when using the ipsilateral method. This finding demonstrates the efficacy of the contralateral method for decompression with facet joint preservation. Although less than one-third of the affected facet joints can tolerate vertebral shear forces [23] in cadaveric study and facet joint destruction does not lead to acute instability due to alternative pathways to support the spine [24], reducing the involvement of the facet joint is one of the final goals of preventing progressing instability in minimally invasive endoscopic surgery, and the bi-contralateral approach we implemented may minimize the destruction of the facet joint, potentially reducing the risk of instability.
Although randomized (level I) and prospective (level II) evidence has shown the benefits of the addition of fusion for spondylolisthesis surgery [25,26], other evidence indicates that fusion provides no distinct benefits in spinal stenosis with spondylolisthesis. Försth et al. [3] randomly selected 247 patients in a study that examined decompression alone and decompression with fusion. The findings showed that the application of fusion did not result in superior results, with similar ODI scores, 6-minute walk test scores, and reoperation percentages between the 2 groups at 2 years. However, the fusion group had a longer length of hospital stay, longer operative time, and greater volume of blood loss. More recently, Inose et al. [27] found that random participants with low-grade (< 30%) L4–5 spondylolisthesis who underwent decompression alone, decompression and fusion, or decompression and stabilization, had no significant differences in the VAS score for low back or leg pain or the Japanese Orthopedic Association score among the 3 groups.
Although minimally invasive fusion is being introduced [28-31], minimally invasive simple decompression has been reported to have medical outcomes equivalent to those of open fusion, with a lower cost, shorter operating time, reduced volume of blood loss, and shorter length of hospital stay than open fusion [3-5]. Some experts particularly prefer decompression only for treating older patients with “stable spondylolisthesis,” owing to the relatively lower morbidity and mortality rates associated with the procedure [4].
Jang et al. [32] retrospectively examined 21 patients who underwent minimally invasive lumbar laminoplasty such as microsurgical bilateral decompression via a unilateral approach for lumbar stenosis associated with grade I degenerative spondylolisthesis. In patients with preoperative evidence of sagittal movement on dynamic radiographs, a significant increase in slippage was noted, explaining why decompression was performed in rigorously selected stable spondylolisthesis with minimal sagittal motion. Kelleher et al. [33] examined data from 25 participants with grade I degenerative spondylolisthesis diagnosed with leg-dominant signs without noteworthy back pain or obvious dynamic instability. Surgical intervention consisted of minimally invasive bilateral decompression using a unilateral approach. In Kelleher’s study, the mean slip progression was 8.4%, which differs from our average slip percentage of 3.10%± 3.39%, despite the lack of a relationship between the degree of olisthesis or radiographic slip development and the need for revision surgery, It is necessary to observe increased slipping with a longer follow-up period.
We performed bilateral-contralateral decompression using UBE to protect the facet and overcome the shortcomings of a typical unilateral laminectomy bilateral decompression. In contrast to reports citing a cumulative reoperation rate as high as 34% [25], our study reported only 2 reoperation fusions among 42 cases (4.8%). Increases in the percentage of asymptomatic slippage and facet cysts were also reported in our study. Two patients had spinous fractures, although their conditions demonstrated sufficient improvement with conservative treatment. It is generally accepted that instability in the lumbar spine is caused by mobile degenerative spondylolisthesis with mechanical low back pain and that the recommended treatment is decompression with fusion [34]. According to a Washington State administrative data report, the rate of reoperation after laminectomy is close to 28% for spondylolisthesis [35]. Compared to other reports [25] in which at least one-third of patients with degenerative spondylolisthesis that underwent lumbar laminectomy required reoperation for nonmobile degenerative spondylolisthesis, our reoperation results are quite encouraging. Our results are complementary to the findings of a previous study that showed that patients in the fusion group had a lower reoperation rate than those treated with decompression alone [25]. To reduce both the sole application of the lumbar spinal fusion process and the possibility of complications, identifying patients whose spines appear to remain steady after decompression is recommended. The generalizability of the reoperation rate in this trial should be assessed in larger prospective registry studies.
The multifidus muscles that provide dynamic spinal stability are intended to sustain as little damage as possible during minimally invasive surgeries. Self-retaining retractors are no longer used, which lowers the intramuscular retraction pressure and risk of muscle crush damage. Focusing the surgical corridor directly over the surgical target site allows for less muscle stripping that may otherwise disrupt its tendinous attachments or damage its neurovascular supply [36]. Since the bilateral-contralateral approach using UBE invades the multifidus muscles on both sides, it may reduce the advantages of the existing minimally invasive surgery when compared to the conventional one-sided approach. However, the injury to the multifidus muscle after UBE surgery has been previously reported to be minimal, showing no difference from that before surgery within several months [37]. The invasion of the facet structure is minimized during contralateral decompression through endoscopic surgery [11,12]. We performed bilateral-contralateral UBE decompression to minimize the involvement of both facet joints in grade 1 spondylolisthesis. This approach can minimize the destruction of both facet joints and potentially minimize the delayed risk of instability that may occur after decompression of the spondylolisthesis. Although it is impossible to compare the impact of instability between bilateral-contralateral decompression and unilateral laminectomy with bilateral decompression using UBE in patients with spondylolisthesis due to the lack of literature.
To the best of our knowledge, this is the first report to provide clinical and radiological results on the extensive use of bilateral-contralateral decomposition via UBE for spinal stenosis in low-grade spondylolisthesis. The use of our bilateral-contralateral approach resulted in only minor complications. Although reoperation was needed in 2 patients with olisthesis due to increased delayed instability after decompression, this method is very promising, as it was associated with a low reoperation rate. Two patients had spinous process fractures, although these occurred due to inexperience in the early period performing bilateral-contralateral decompression. Conservative treatment was sufficient for back pain. Spinous fractures can occur when inexperienced surgeons perform the bilateral-contralateral approach. Although this can be alleviated with conservative treatment, it can also reduce the patients’ postoperative satisfaction. To prevent spinous process fractures, when performing left decompression through the right approach after completing right decompression through the left approach, the right approach rather than the left approach should go to the caudal side. It is possible to prevent additional laminectomy in the existing laminectomy, thereby minimizing the invasion of the spinous process base. Although not essential, using dual monitors was effective in reducing the operation time because the operator could move to the opposite side and initiate contralateral access without moving the UBE deck and monitor.
This study had a relatively small sample size (42 patients); thus, further studies with larger sample sizes are required to verify these results.
In this case series, we encountered a lack of consensus regarding the definition of lumbar instability in the literature, including wide thresholds of 2–5 mm on flexion-extension radiographs [38]. In this study, a threshold of 3-mm sagittal translation and 10° sagittal rotation was used, based on flexion-extension imaging [39]. The actual percentage of patients with postoperative instability may be higher, as asymptomatic patients may have missed follow-up after 2 years. We performed the final radiography a minimum of 24 months after surgery. However, the final follow-up duration differed for each patient, which may have affected the outcomes. The error in the results could have been reduced if the follow-up time after surgery had been uniform for all patients.
Previous reports have shown that patients with lumbar degenerative spondylolisthesis tend to have a propensity for sagittal imbalance and a higher pelvic incidence than patients with degenerative spinal stenosis, and that sagittal imbalance in patients with degenerative spondylolisthesis is correlated with the loss of lumbar lordosis [40]. However, global sagittal parameters could not make pre- and postoperative comparisons. There are limitations to discovering an association between global sagittal parameters and slippage in spondylolisthesis after bilateral-contralateral UBE decompression.
Excellent results were obtained for the preservation of the facet joint in our study. However, although the rate of reoperation was lower than that after decompression, as reported in previous studies, no patient in the control group was treated with unilateral laminectomy bilateral decompression for specific comparisons. Therefore, whether unilateral laminectomy with bilateral decompression has clinical significance remains unclear. Further studies, particularly randomized controlled experiments and studies with control groups, are necessary to explore this subject further.
CONCLUSION
In our study, applying bilateral-contralateral UBE decompression in patients with lumbar spinal stenosis and grade 1 degenerative spondylolisthesis provided good clinical mid-term medical results with a low reoperation rate, despite a slight increase in slippage. We believe that bilateral-contralateral UBE decompression for lumbar spinal stenosis with grade 1 degenerative spondylolisthesis may be a good surgical option for lowering the rate of postoperative instability.
Supplementary Materials
Supplementary Figs. 1-4 can be found via https://doi.org/10.14245/ns.2346504.252.
(A) Preoperative axial T2-weighted magnetic resonance imaging (MRI) demonstrating lumbar spinal stenosis at the level of L4–5 in spondylolisthesis. (B) Postoperative axial MRI image shows decompression after the bilateral-contralateral decompression. (C) Preoperative computed tomography (CT) scan images demonstrating lumbar spinal stenosis at the level of L4–5 in spondylolisthesis. (D) Postoperative CT scan image with minimal facet resection.
Flexion (A) and extension (B). Digital plain radiographic images are used to determine the movement at the level of spondylolisthesis (3.76° motion in this case). (C) Disc height was gauged based on preoperative lumbar computed tomography scans by applying a midsagittal image and identifying the gap from the midpoint of the endplate at the level of the spondylolisthesis. (D) The facet angle was measured by calculating the angle generated by linking the 2 endpoints of each facet on a preoperative axial lumbar computed tomography (midcut through the disc) and a line linking the 2 dorsal points of each facet joint. When the facet angles were different (right side vs. left side), the average value was applied (69.5° in this example).
Measurement of facet joint preservation on preoperative (A) and final follow-up (B) via magnetic resonance imaging. The dashed lines highlight the extent of the laminotomy. The percentage of facet preservation=y/x×100%.
Progression of anterior slippage. The average overall slip percentage was 15.70%±5.25% preoperatively, which increased to 18.80%±5.41% at the last follow-up. PreOp, preoperation; PostOp, postoperation.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: DHL, DGL, CKP, JSH, SWL, SYH; Data curation: DHL, DGL, JWJ, JSH, JYK, YEC, DCL, BSH; Formal analysis: DHL, DGL; Funding acquisition: DHL, CKP; Methodology: DHL, JWJ; Project administration: DHL, DGL; Visualization: DHL; Writing - original draft: DHL; Writing - review & editing: DHL, DGL, CKP.