Comparative Efficacy of Surgical Interventions for Osteoporotic Vertebral Compression Fractures: A Systematic Review and Network Meta-analysis
Article information
Abstract
Objective
We aimed to comprehensively compare surgical methods for osteoporotic vertebral compression fracture (OVCF) using systematic review and network meta-analysis to understand their effectiveness and outcomes, as current research provides limited overviews.
Methods
We followed PRISMA (preferred reporting items for systematic reviews and meta-analyses) guidelines, preregistering our protocol with PROSPERO. We analyzed English-published randomized controlled trials (RCTs) on adults with OVCFs that evaluated pain intensity or functionality using tools like visual analogue scale (VAS) or Oswestry Disability Index (ODI). Exclusions included non-RCTs, malignancy-related fractures, and certain interventions. Using the RoB 2 tool, we assessed bias and visualized results with Robvis. Our primary outcome was pain intensity, with secondary outcomes including disability, new fractures, and cement leakage. Results were synthesized using Stata/MP.
Results
Thirty-four RCTs from 10 countries, totaling 4,384 patients, were analyzed. Short-term VAS indicated kyphoplasty with facet joint injection (KIJ) as the top treatment at 87.7%, while unipedicular kyphoplasty (UKP) led to long-term at 74.9%. Short-term ODI favored vertebroplasty with facet joint injection (VIJ) at 98.4%, with kyphoplasty (KP) leading long-term at 66.0%. All surgical techniques were superior to conservative treatment. Vertebral augmentation devices reported the fewest new fractures and curved vertebroplasty had the least cement leakage. SUCRA (surface under the cumulative ranking) analyses suggested UKP and VIJ as top choices for postoperative pain relief, with VIJ excelling in postoperative disability improvement.
Conclusion
Our analysis evaluates 12 OVCF interventions, underscoring KIJ for short-term pain relief and VIJ and UKP for long-term efficacy. Notably, VIJ stands out in disability outcomes, emphasizing the need for comprehensive OVCF management.
INTRODUCTION
A pivotal linkage exists between osteoporosis and osteoporotic vertebral compression fractures (OVCFs). This association has garnered considerable attention as an escalating health challenge and has become even more pronounced, especially among women populations that are progressively aging [1,2]. Given the global demographic tilt towards an older population, the prevalence of OVCF is anticipated to soar. The European Commission’s projections paint a worrisome scenario with a forecasted 57% surge in OVCF incidences in the European Union in the forthcoming 5 decades [3-5]. Parallel trends are evident in the United States, highlighting the widespread nature of this health predicament [6]. On a broader scale, approximately 1.4 million individuals globally are clinically diagnosed with OVCF each year, leading to a spectrum of outcomes from debilitating physical constraints to significant economic strains [7].
OVCF, characterized by intense pain and spinal deformities, substantially hinders the patient’s overall daily life activities. Disturbingly, while as many as 25% of women aged over 50 and 40% over 80 possess OVCF annually, an alarming two-thirds of such cases often remain undiagnosed or unattended [8]. The consequences of these fractures span from intense physical discomfort and loss of mobility to a palpable deterioration in overall quality of life [5]. While a majority of OVCF patients find success in conventional treatments such as bed rest, pain management, and rehabilitative exercises [9], there is a fragment of those for whom surgical interventions become imperative, especially when earlier treatments fail or the progression of deformities, or neurological deficits [9]. Although the current literature demonstrates many studies investigating varied available OVCF interventional options, there is still a lack in terms of a holistic, encompassing investigation of all available techniques. Moreover, those studies, often confined to the pairwise methods in their methodology, pose a challenge to obtaining a comprehensive overview. Therefore, we aim to provide an expansive investigation, juxtaposing all current surgical interventions for OVCF to evaluate their relative efficacies and clinical outcomes. Leveraging the usefulness of systematic review and the recently developed network meta-analysis (NMA) protocols, we intend to shed light on this potentially important underexplored area in this research.
MATERIALS AND METHODS
1. Search Strategy and Eligibility Criteria
This study was reported in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [10]. The protocol for our systematic review and meta-analysis was preregistered with PROSPERO (Registration No. CRD42023472135). We conducted comprehensive searches across PubMed (MEDLINE), Web of Science, Embase, and the Cochrane Library, covering from database inception to September 2, 2023. Adhering to the Cochrane Handbook for Systematic Reviews of Interventions. During the study selection process, 2 investigators independently assessed each study’s title, abstract, and full text, with disagreements arbitrated by a third reviewer. YT and SS extracted data into Microsoft Excel using a predefined standardized template. The extraction encompassed a comprehensive range of clinical and methodological trial characteristics, as outlined in the protocol. In instances of data extraction disagreements, a third reviewer (JSK) facilitated consensus. Key data points extracted from eligible studies included author, identifier, journal, country, publication year, duration, center, interventions, control group, follow-up duration, participant count by gender, age, outcome measurements, and utilized instruments.
To be eligible for this research, included studies must meet the following criteria: they should be fully published randomized controlled trials (RCTs) in English that involve adult participants (≥18 years) diagnosed with OVCF. These studies should comprise a control group receiving conservative treatments (Cts) and an intervention group exposed to treatments. The study outcomes should encompass pain intensity or functioning status measured through certificated clinical measurement tools like the visual analogue scale (VAS) or Oswestry Disability Index (ODI). If there are multiple publications from the same dataset, we will consider the one with the most comprehensive data and the longest follow-up period. Conversely, studies will be excluded if they are not RCTs, trials, reviews, case studies, conference abstracts, meeting proceedings, and editorials; deal with vertebral compression fractures stemming from malignancy or trauma, such as Kümmell Disease; employ stem cell therapy or minor modified technique, like novel design opening cannula; Intravenous Zoledronic acid infusion as variable intervention accompany with vertebroplasty (VP) or kyphoplasty (KP).
2. Risk of Bias Assessment and Outcomes Measurements
Two reviewers, YT and JL, independently evaluated the risk of bias (RoB) within the incorporated studies utilizing the RoB 2 tool specifically crafted for RCTs [11]. This robust assessment tool classifies biases into 5 distinct domains for individually randomized trials: (1) bias stemming from the randomization process, (2) bias resulting from deviations from the intended intervention, (3) bias owing to absent outcome data, (4) bias in the quantification of the outcome, and (5) bias in the selection of the reported result. For a more transparent and comprehensive depiction of the RoB evaluations, we employed the Robvis visualization tool to elucidate and present our findings in this systematic review and NMA [11].
The primary endpoint in our NMA model focused on pain intensity, gauged both short- and long-term through tools such as the VAS or Numerical Rating Scale. As for the secondary outcomes, they encompassed short- and long-term disability indices quantified through the ODI. Furthermore, the data took into account the number of new fractures and assessed instances of cement leakage during procedures involving cages.
3. Data Synthesis and Statistical Analysis
In our analysis, the NMA was executed using Stata software, taking advantage of the specialized “network” and “mvmeta” modules. We adopted a random-effects approach framed within the frequentist paradigm for aggregating the data extracted from RCTs. The software’s architecture presupposes that heterogeneity variance remains constant across all contrasted treatments within the study pool. A graphical network topology was generated to offer a visual depiction of the interrelationships among the selected studies [12]. In terms of research categorization, the studies were classified into Indirect Treatment Comparisons or Mixed Treatment Comparisons based on the emergent loop configurations within the network architecture. In cases of data unavailability, relevant statistical imputation techniques were employed. To ensure the reliability of the composite effect size, preliminary statistical assumptions were scrutinized to affirm the internal coherence of the NMA framework. To ascertain if heterogeneity originated from external or internal factors, node-splitting was conducted to evaluate the persistence of heterogeneity among the included studies. We computed effect sizes and their associated variances in direct and indirect pairwise comparisons, utilizing confidence and predictive intervals to adjust for varying levels of heterogeneity. We took additional steps to ascertain the uniformity of the aggregated data, applying logical inference hypotheses that account for potential inconsistencies.
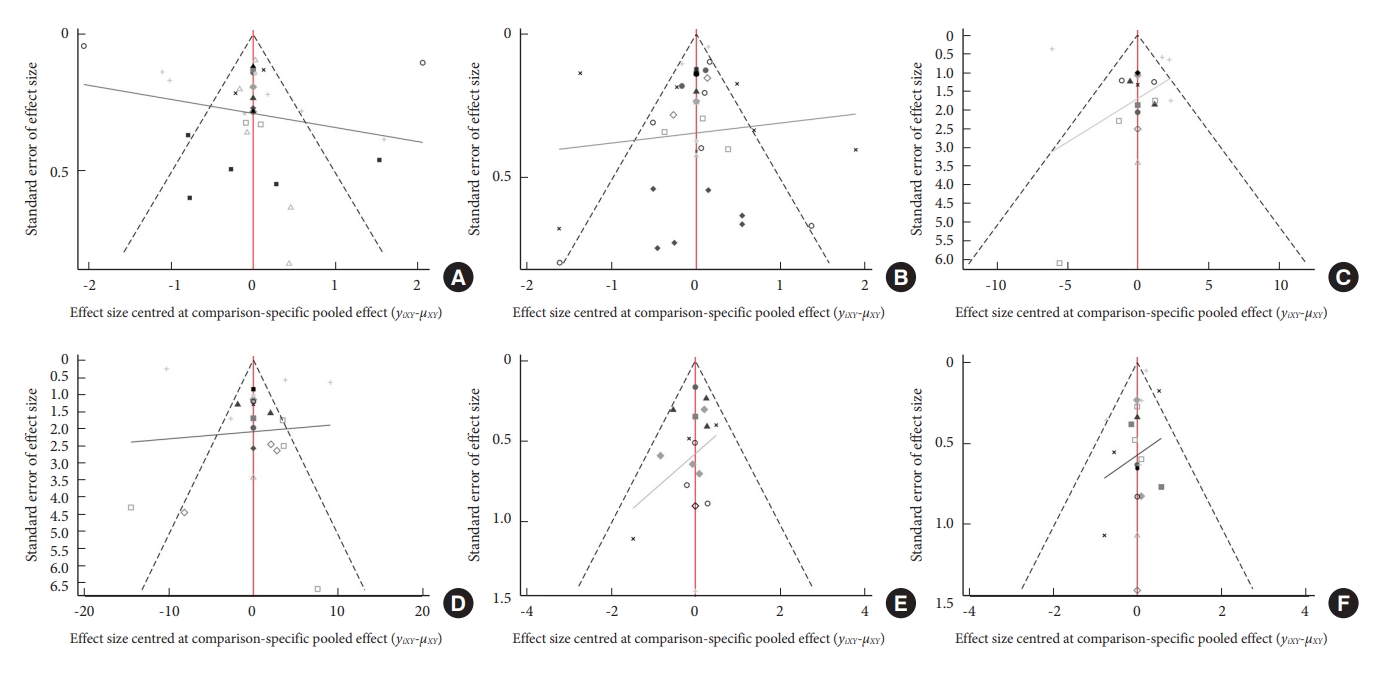
The net league square matrix is designed to encapsulate all pairwise comparisons in NMA. This methodology provides a comprehensive view of both direct and indirect evidence, enabling efficient interpretation of comparative treatment effects. Our analysis employed the surface under the cumulative ranking (SUCRA) methodology to formulate a treatment hierarchy. This method allowed for a data-driven, probabilistic stratification of the various therapeutic interventions and estimated the potential order of superiority for each clinical intervention by comparing their probability values against others [13]. SUCRA values range from 0% to 100%. Leveraging these SUCRA percentages, we executed a cluster analysis aimed at quantifying the holistic efficacy probabilities associated with each treatment option. Formal checks for publication bias were conducted through an asymmetrical analysis of comparison-adjusted funnel plots to spot any undue influence of smaller studies. All statistical computations and graphical renderings were facilitated using the comprehensive suite of network analysis tools available in Stata/MP (Release 17, StataCorp LLC, College Station, TX, USA).
RESULTS
1. Study Characteristics
The database search yielded 2,982 records, which were initially filtered using automation tools. A hands-on review of the titles and abstracts led to the exclusion of 138 articles that failed to satisfy the inclusion criteria. Consequently, we identified 34 RCTs spanning 10 countries, which collectively represented 4,384 patients, for inclusion in the NMA (Fig. 1). A detailed breakdown of the characteristics of these RCTs is provided in Table 1 [14-47]. Across these RCTs, 12 interventions were evaluated (Fig. 2), including VP, KP, unipedicular VP or KP (UVP or UKP), VP or KP with subsequent facet block or medial-branch-block injection (VIJ or KIJ), curved VP or KP (CVP or CKP) technique, pedicle screw fixation/fusion with or without vertebral augmentation (PSV), vertebral augmentation devices (VA), Sham procedure (SP), or Ct. The average participant age was 73.36 years. A significant proportion of the studies (70.59%) were undertaken in the United States, Australia, or China between 2009 and 2023. A thorough risk analysis revealed that 44.11% of the studies exhibited a low RoB, while 3 studies had notable risks tied to their randomization and intervention methodologies (Fig. 3).
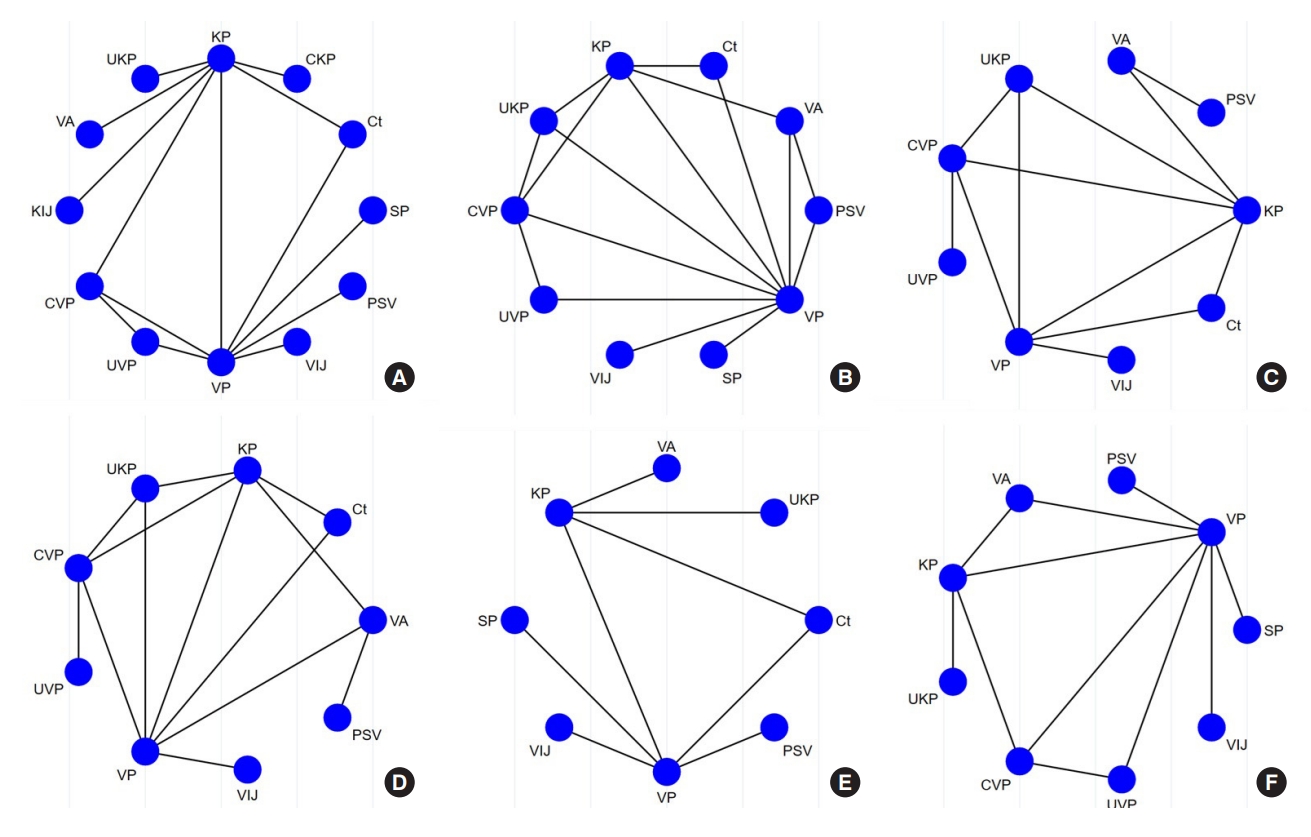
Network geometry of the network meta-analysis. Network meta-analysis diagrams. (A) Short-term VAS. (B) Long-term VAS. (C) Short-term ODI. (D) Long-term ODI. (E) New fracture. (F) Cement leakage. VAS, visual analogue scale; ODI, Oswestry Disability Index; KP, kyphoplasty; CKP, curved kyphoplasty; Ct, conservative treatment; SP, Sham procedure; PSV, pedicle screw fixation/fusion with or without vertebral augmentation; VIJ, vertebroplasty with facet joint injection; VP, vertebroplasty; UVP, unilateral vertebroplasty; CVP, curved vertebroplasty; KIJ, kyphoplasty with facet joint injection; VA, vertebral augmentation devices; UKP, unipedicular kyphoplasty.
2. NMA and Ranking Probabilities
Within a sample of 4,049 participants from 29 RCTs, pooled results of short-term VAS showed that Ct as a reference, CKP (mean 3.52, 95% confidence interval [CI] 1.23 to 5.81), CVP (mean 3.25, 95% CI 1.69 to 4.81), KIJ (mean 4.91, 95% CI 2.55 to 7.28), and other measurements illustrate the nonsignificant difference of improvement. Moreover, no significant difference was found among other pairwise comparisons. Furthermore, the long-term VAS outcomes displayed a similar trend when set Ct as a reference, with the exception that the groups treated with UKP (mean, 1.09; 95% CI, 0.08–2.09), VP (mean, 0.76; 95% CI, 0.07–1.45), and KP (mean, 0.86; 95% CI, 0.04–1.67) demonstrated significantly greater improvements compared to the SP group. The results were observed in the pairwise forest plot or netleague square matrix (Supplementary File). The cumulative probability for efficacy in short-term VAS indicates a marked preference for KIJ at 87.7%, followed by CKP and other treatments. In a broader sample involving 33 RCTs and 4,107 participants, when evaluating long-term VAS, UKP led the chart at 74.9%, with VIJ and other treatments following closely. Notably, nearly all surgical and SPs showcased a pronounced reduction in short-term VAS in contrast to Cts, with no discernible statistical difference in short-term pain intensity across surgical interventions. The net league diagram in Fig. 4 and Supplement Material provides a visual representation of comprehensive head-to-head comparisons for all measured metrics among various interventions.
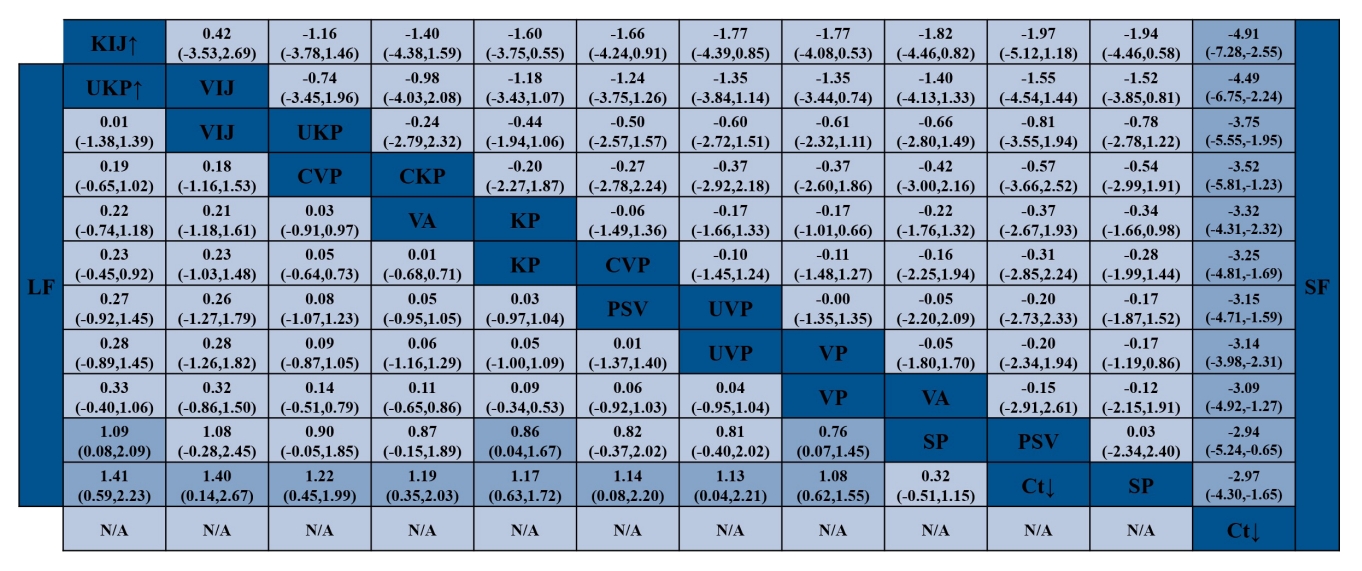
Netleague square matrix from the network meta-analysis detailing all pairwise treatment comparisons. KP, kyphoplasty; CKP, curved kyphoplasty; Ct, conservative treatment; SP, Sham procedure; PSV, pedicle screw fixation/fusion with or without vertebral augmentation; VIJ, vertebroplasty with facet joint injection; VP, vertebroplasty; UVP, unilateral vertebroplasty; CVP, curved vertebroplasty; KIJ, kyphoplasty with facet joint injection; VA, vertebral augmentation devices; UKP, unipedicular kyphoplasty; LF, long-term follow-up; SF, short-term follow-up; N/A, not applicable.
For the ODI, evaluations showed distinct probabilities for both short- and long-term outcomes. Analyzing data from 17 RCTs with 2,087 participants for short-term outcomes, pooled results of all available measurements illustrate significant differences when conservative as reference. Additionally, the short-term improvements in ODI were significantly greater in the VIJ group compared to those observed in the KP (mean, 7.31; 95% CI, 0.80–13.83), UVP (mean, 11.71; 95% CI, 2.25–21.17), VA (mean, 10.51; 95% CI, 0.73–20.29), and VP (mean, 9.11; 95% CI, 3.37–14.85) groups. For the long-term ODI, pooled results only showed KP (mean, 10.46; 95% CI, 3.52–17.40) and VP (mean, 8.69; 95% CI, 3.16–14.21) demonstrated significantly greater improvements compared to the Ct group. The VIJ emerged as the leading intervention for OVCFs with a 98.4% probability, followed by UKP at 77.3%, KP at 69%, and CVP at 59.2%. In an evaluation focusing on long-term outcomes with 19 RCTs and 2,219 participants, KP topped the list with a 66.0% probability, trailed by VIJ at 63.1%, CVP at 56.7%, and VP at 49.2%. Notably, every surgical intervention displayed a significant advantage over Ct. Specifically, VIJ exhibited pronounced benefits in enhancing postoperative short-term ODI compared to most other treatments, such as KP, CVP, VP, VA, and UVP. Nevertheless, for long-term ODI outcomes, statistical comparisons between various clinical interventions did not yield significant disparities.
In assessing the occurrence of new fractures, data was drawn from 17 RCTs involving 2,087 participants. Interestingly, no marked differences were observed in the rates of new fractures among the VIJ, VP, KP, UKP, SP, Ct, VA, and PSV groups (Supplementary File). The SUCRA plot further highlighted that the VA intervention exhibited the lowest propensity for new fractures. Contrastingly, the incidence of cement leakage, analyzed from another set of 17 RCTs with 2,075 participants, showcased pronounced leakage variances in KP (relative risk [RR], 1.91; 95% CI, 1.02–3.60) and VP (RR, 1.73; 95% CI, 1.01–2.98) groups compared to the CVP group, as well as in the comparison between VP and UVP (RR, 8.69; 95% CI, 1.03–2.67) group. In this context, the SUCRA plot revealed that the CVP intervention had the least likelihood of cement leakage.
The SUCRA plot, as presented in Fig. 5, systematically ranks the surgical interventions based on both absolute and cumulative effects. Insights drawn from the SUCRA cluster analyses, illustrated in Fig. 6, suggest that UKP and VIJ potentially offer optimal relief from postoperative pain, both in the short and long run. Moreover, when focusing on postoperative disability outcomes over both short and long durations, VIJ may emerge as the most favorable intervention.
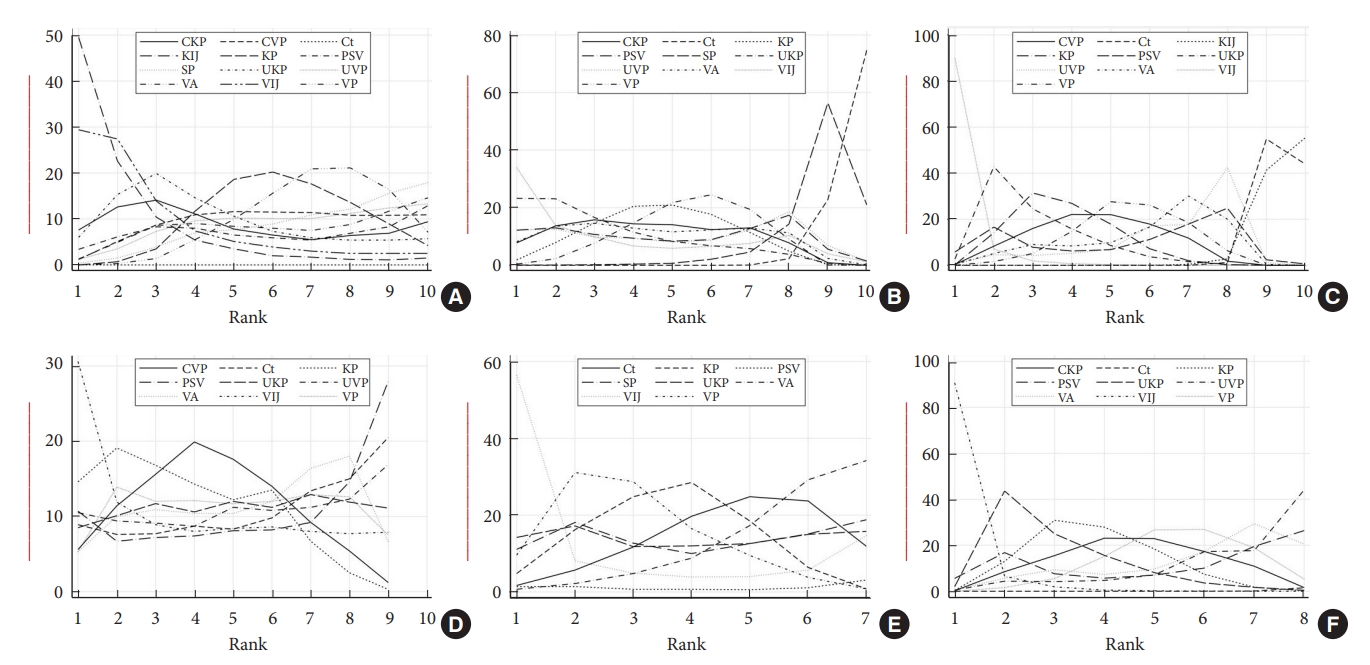
SUCRA (surface under the cumulative ranking) plots that rank surgical interventions based on absolute and cumulative probability of effect. (A) Short-term VAS. (B) Long-term VAS. (C) Short-term ODI. (D) Long-term ODI. (E) New fracture. (F) Cement leakage. VAS, visual analogue scale; ODI, Oswestry Disability Index; KP, kyphoplasty; CKP, curved kyphoplasty; Ct, conservative treatment; SP, Sham procedure; PSV, pedicle screw fixation/fusion with or without vertebral augmentation; VIJ, vertebroplasty with facet joint injection; VP, vertebroplasty; UVP, unilateral vertebroplasty; CVP, curved vertebroplasty; KIJ, kyphoplasty with facet joint injection; VA, vertebral augmentation devices; UKP, unipedicular kyphoplasty.

Hierarchical plots displaying the ranking of intervention probability on the impact of pain (A) intensity and disability index (B). UKP, unipedicular kyphoplasty; VIJ, vertebroplasty with facet joint injection; CVP, curved vertebroplasty; VA, vertebral augmentation devices; KP, kyphoplasty; VP, vertebroplasty; UVP, unilateral vertebroplasty; PSV, pedicle screw fixation/fusion with or without vertebral augmentation; Ct, conservative treatment; SP, Sham procedure.
3. Consistency Test and Heterogeneity Analysis
In our network analysis, we observed controlled consistency between different treatments in terms of VAS, ODI, new fracture, and cement leakage (p ≥ 0.05). Only several arms showed significant inconsistency between different treatments for VAS, ODI, and adverse events, those considered the potential sources of populations or surgical techniques across the included studies. According to our statistical analysis, the design-by-treatment interaction inconsistency model is fit with no evidence for inconsistency in each outcome measurement using the restricted maximum likelihood. The global inconsistency values were p = 0.521 for short-term VAS, p = 0.983 for long-term ODI, p = 0.931 for short-term ODI, p = 0.373 for long-term ODI, p = 0.575 for new fracture, p = 0.931 for cement leakage, respectively.
Node-splitting analysis revealed low statistical inconsistency between direct and indirect evidence for the assessed treatment comparisons, suggesting our NMA results for these comparisons are robust. The comparison-adjusted symmetrical funnel plots demonstrated promising results, indicating a lower likelihood of publication bias or small-study effects. Notably, a minimal number of studies were located outside the funnel’s boundaries, further reinforcing the overall reliability and robustness of our findings (Fig. 7). Furthermore, due to the limited number of loops present, the potential for loop inconsistency was diminished. Therefore, we did not evaluate loop inconsistency that was made based on the specific structure of our network.
DISCUSSION
In the present NMA, we undertook an assessment of the clinical outcomes stemming from 12 interventions used for OVCFs. These outcomes were delineated by their short-term and long-term results. The VAS was employed to measure pain intensity, while the ODI gauged the extent of disability, serving as an indirect indicator of patients’ overall quality of life. When considering short-term results using the VAS, KIJ was pre-eminent. For long-term results, however, UKP took the lead but was also closely followed by VIJ. These findings underscore the pivotal role of subsequent injection procedures in pain management, both in immediate and enduring terms, as corroborated by contemporary research [48,49]. Prior studies have pinpointed the posterior segment of the vertebral body—particularly the facet joints —as a primary source of pain in certain situations. Age-related degeneration within spinal tissues, compounded by fractures, may intensify this discomfort. Notably, while VP targets pain arising from vertebral fractures, it demonstrates diminished efficacy in addressing pain attributed to residual injuries typically associated with posterior spinal trauma. For pain relief, targeting these nerves via facet joint injections has been proven efficacious [50]. A pioneering study by Kim et al. [51] evaluated the impact of combining percutaneous VP with facet block across 612 vertebral levels of OVCF. They deduced that this combined approach is advantageous owing to its minimal risks, expedited procedure, and heightened probability of facilitating pain alleviation and rapid return to mobilization. A recent RCT juxtaposed the efficiency and safety of VP combined with a subsequent facet joint block against VP alone. Although both methods proved beneficial, the combined approach exhibited superior back pain alleviation in the short term [17]. This convergence with ODI outcomes corroborates our findings, positioning VIJ at the forefront or near the top of our analysis. Therefore, this also underscores the amplified efficacy of postoperative injections in OVCF cases. Additional comprehensive RCTs, paired with an evaluation of cost-effectiveness relative to alternative interventions, are both essential and warranted in the future.
Concerning complications and safety, the most frequent severe issues postintervention in OVCF patients are new fractures and cement leakage. While no discernible differences exist in the rates of new fractures across our studied interventions, VA intervention exhibited the lowest propensity for new fractures according to the SUCRA analysis. Tutton et al. [30] have demonstrated the safety and effectiveness of the novel vertebral augmentation system (Kiva system) for the treatment of OVCF and found that it was noninferior to balloon KP to relieve pain and improved the overall function of the patients with superiority toward cement leakage and the new fracture rates. However, from our study, there is a notable discrepancy in cement leakage rates between the CVP group and the VP or KP groups. Two potential explanations arise for this distinction, both possibly related to the unique curved technique employed in the featured studies. Firstly, the amount of cement injected in the CVP group might be less than what is typically utilized in the standard KP or VP methods. Additionally, by strategically injecting the cement at the anterior zone of the vertebra with the aid of a flexible guide curving from one pedicle side, the procedure not only augments load support but also offers the advantage of administering the cement more anteriorly than traditional methods. As a result, the risk of cement leakage from the posterior wall of the vertebral body, which could gravely compress neurological structures, is likely to be diminished. Echoing our findings, Shi et al. [16] executed a 1:1 RCT, contrasting traditional KP with the innovative CVP technique on 90 OVCF patients. Both groups evidenced roughly comparable improvements in clinical outcomes. However, the CVP group fared significantly better in terms of lessening radiation exposure, operative duration, and the volume of cement required for injection. Intriguingly, despite the absence of statistical significance, there is an observable lessen trend toward a cement leakage rate in the CVP group. Similar optimistic results have been reported in other research [15,19,20]. Future studies encompassing a broader participant base are essential. Such investigations could potentially underscore the superior efficacy of CVP, particularly regarding its decreased propensity for cement leakage.
Intriguingly, our analysis found that SP significantly reduced the short-term VAS compared to Ct, a decrease that was on par with other interventions. This suggests the potential influence of the placebo effect, particularly during the initial stages of treatment. Therefore, caution is advised when interpreting results from such studies. This observation aligns with findings from several preceding studies. Numerous reputable RCTs have indicated no substantial difference in primary endpoints ranging from 6 months to 2 years between VP and SP, inferring that VP may not offer significant advantages over SP [22,37,47,52,53]. It is essential to clarify that referencing the “placebo effect” does not insinuate that the associated therapeutic outcomes are illusory. Comprehensive research, especially related to pain, has conclusively demonstrated that the placebo response is a genuine neurobiological event capable of delivering clinically significant advantages [54]. Some perspectives on this matter posit that the continuation of such procedures in clinical practice is hard to justify [55]. Even if a substantial component of improved clinical outcomes can be attributed to the placebo effect, there is skepticism about whether the placebo response from VP is substantial enough to warrant the associated risks. This is also considering numerous studies that have lauded the merits of VP [35,40,42,56]. However, in our NMA, although SP was shown to be efficacious, its SUCRA ranking did not eclipse that of other treatments. This observation, consistent with previously postulated theories, suggests that while a placebo effect might be present, it may not be dominant enough to overshadow the merits of existing treatments. This further underscores the value of our study’s NMA approach, allowing a comprehensive simultaneous comparison of multiple interventions, thereby providing a deeper understanding of the relative efficacy and standing of each treatment modality.
More from our findings, it is evident that every interventional technique outperformed Ct in every interested outcome. Based on prior research, Ct often falls short in alleviating pain and enhancing mobility, particularly in instances where there is a continued loss of vertebral body height or an exacerbation of kyphotic deformity. Additionally, if not meticulously diagnosed and managed, Ct can exacerbate disability, provoke intolerable side effects from narcotic analgesics, and induce bone demineralization [57]. Amidst the rapidly evolving therapeutic landscape for OVCFs and the broader domain of osteoporosis, a wealth of innovative evidence has surfaced, illuminating prospective and promising treatment directions. A seminal study by Shim et al. [58], for instance, investigated the combined use of Wharton’s jelly-derived mesenchymal stem cells and teriparatide in treating OVCFs. Their phase I/IIa research revealed that this combined modality is not only feasible and safe but also exceptionally effective in enhancing bone structure and expediting fracture healing. This groundbreaking work emphasizes the significance of amalgamating stem cell therapy with existing treatment modalities, offering a compounded benefit that might be transformative for OVCF management. As we navigate the surgical strategies for OVCFs, it becomes paramount to incorporate these cutting-edge developments, given their potential to elevate patient outcomes, diminish recuperation periods, and possibly curtail complications associated with conventional modalities. Merging stem cell therapy with relatively contemporary anabolic agents like teriparatide could usher in a revolutionary phase in OVCF treatment, warranting attention for future investigations and clinical applications.
We prioritized a stringent focus on RCTs, aiming to offset the known placebo effects common to invasive treatments and to address the complexities present in open-label studies adeptly in our study. A notable observation from our research was the pronounced heterogeneity across study findings. This could be linked to evolving surgical techniques, differences in practitioner expertise, and subjective variations in pain thresholds among participants. An interesting demographic pattern was the marked presence of females in OVCF cases. Methodologically, our study displayed several commendable attributes, including a thorough search protocol, the integration of a RoB evaluation to diminish inherent biases, and the strategic application of SUCRA analysis to assess the superior intervention comprehensively.
Despite these strengths, some limitations exist and need to be mentioned. First, a palpable lack of standardized criteria for discerning types and definitions of cement leakage—whether into the disc, perivertebral veins, pulmonary system, or spinal canal —was observed. Such an absence of consensus leads researchers to establish their own benchmarks, potentially obfuscating risk factor computations, especially when a meta-analysis is unduly reliant on a specific study. The lack of a further classification of the nature of fractures, whether adjacent or subsequent, or how much the extent of the pedicle screw fixation levels, whether it was short or long segments, or adjunctly use the augmentation or not, were not investigated in detail. All of these may also add another layer of heterogeneity, complicating comparisons across studies. Second, our research, while extensive, did not provide a detailed classification of osteoporosis severity. Undoubtedly, treatment recommendations for vertebral fractures vary depending on whether the patient has acute, chronic, severe, or generalized osteoporosis. The underreporting of detailed patient characteristics and their respective protocols of treatment related to OVCF in the included studies altered the choices of treatment and could make it vary between studies. Moreover, information on fracture types, severity, and duration, which are pivotal for tailoring treatment modalities and predicting outcomes, was inconsistently documented. This lack of granularity limits the depth of our analysis and the generalizability of our findings. Future research is thus encouraged to delve deeper into these nuances. We also recommend that forthcoming studies embrace a uniform reporting framework, including registering each RCT and providing an openly accessible detailed protocol. Enriching reports with visual data and related values would enhance transparency and comprehension. Third, the SUCRA rankings, although structured, are not infallible. These rankings might be grounded in evidence of inconsistent quality, thus leading to potentially shaky conclusions. SUCRA tends to emphasize singular outcomes, sidelining the intricate dynamics inherent in multi-dimensional medical treatments. It does not factor in critical considerations such as cost implications, practitioner familiarity with specific treatments, or nuanced differences in treatment impact. Additionally, the role of random chance on treatment outcomes is overlooked, potentially skewing perceptions of their comparative effectiveness. Thus, our conclusions, while informed, should be interpreted with a measure of restraint, not as incontrovertible evidence. To validate the efficacy of the diverse interventions, more extensive multi-arm RCTs are still essential.
CONCLUSION
In conclusion, the recent NMA meticulously assesses the effectiveness and safety of 12 interventions for OVCF. The data underscores KIJ’s prominence in short-term pain relief, while VIJ and UKP excel in long-term efficacy. VIJ consistently stands out in disability outcomes, emphasizing the complex nature of OVCF management. The success rates of KIJ and VIJ further accentuate the significance of injection procedures in pain management, suggesting the need for holistic treatment approaches that address both symptoms and root causes of OVCF pain. However, while our analysis is comprehensive, it is not exempt from the typical limitations, particularly concerning standardization in reporting cement leakages and fracture classifications. Future studies should entail a nuanced categorization of osteoporosis severity to ensure more precise treatment outcomes. With the ever-evolving medical field, integrating innovative treatments like stem cell therapy into OVCF procedures might be the way forward, affirming the continuous pursuit of enhanced patient outcomes.
Supplementary Material
Notes
Conflict of Interest
Jin-Sung Kim is a consultant of RIWOSpine, GmbH, Germany; Elliquence, LLC, USA; and Stöckli Medical AG, Switzerland. The other authors have no conflicts of interest to declare.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: YL, SS, IH, JSK; Formal analysis: YL, JL; Methodology: YL, JL; Project administration: IH, JSK; Visualization: IH, JSK; Writing - original draft: YL, SS, JL; Writing - review & editing: YL, SS, IH, JSK.