Fusion Assessment of Oblique Lumbar Interbody Fusion Using Demineralized Bone Matrix: A 2-Year Prospective Study
Article information
Abstract
Objective
Although several studies have reported successful fusion rates after oblique lumbar interbody fusion (OLIF) using allografts or dimerized bone matrix (DBM) instead of autografts, whether OLIF can achieve satisfactory solid fusion without the use of autografts remains unclear. This study investigated the real fusion rates after OLIF using allografts and DBM, which were evaluated using both dynamic radiographs and computed tomography scans.
Methods
We enrolled 79 consecutive patients who underwent minimally invasive OLIF followed by percutaneous pedicle screw fixation. All patients were treated with OLIF between L2 and L5 and underwent radiographic and clinical follow-ups at 12, 18, and 24 months after surgery. Radiographic assessment of fusion was performed using the modified BrantigaSteffee-Fraser (mBSF) scale, which was categorized as follows: grades I (radiographic pseudoarthrosis), II (indeterminate fusion), and III (solid radiographic fusion). Other radiologic and clinical outcomes were evaluated using the following parameters: vertebral slippage distance, disc height, subsidence, Oswestry Disability Index (ODI), and visual analogue scale (VAS).
Results
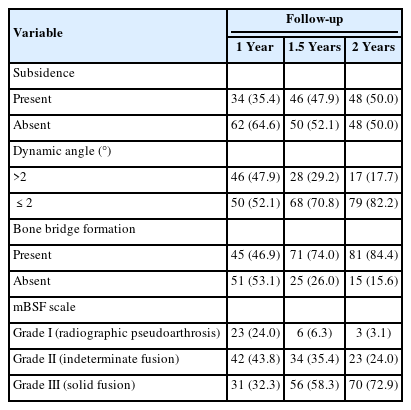
Clinical outcomes demonstrated significant improvements in the VAS scores for back pain, leg pain, and ODI after surgery. Subsidence was present in 34 cases (35.4%) at 12 months postoperatively, which increased to 47.9% and reached 50.0% at 1.5 years and 2 years after surgery, respectively. The solid fusion rate after OLIF was 32.3% at 1 year, increased to 58.3% at 1.5 years, and reached 72.9% at 2 years. Radiographic pseudoarthrosis was 24.0% at 1 year, which decreased to 6.3% at 1.5 years and 3.1% at 2 years.
Conclusion
OLIF is a safe and effective surgical procedure for the treatment of degenerative lumbar diseases. The mBSF scale, which simultaneously evaluates both dynamic angles and bone bridge formation, offers great reliability for the radiological assessment of fusion. Moreover, OLIF using allografts and DBM, which is performed on one or 2 levels at L2–5, can achieve satisfactory fusion rates within 2 years after surgery.
INTRODUCTION
Degenerative lumbar spine diseases, including spinal stenosis with or without spondylolisthesis, are a common problem in the aging population. Among various surgical techniques, lumbar interbody fusion remains widely accepted and effective in treating degenerative lumbar diseases and is more popular than other fusion techniques such as instrumented posterolateral fusion [1,2].
Traditionally, many kinds of lumbar interbody fusions have been conducted, such as posterior lumbar interbody fusion (PLIF), transforaminal lumbar interbody fusion (TLIF), anterior lumbar interbody fusion (ALIF), and direct lumbar interbody fusion using different approaches and fusion materials [2-9]. In recent years, TLIF can be performed via a minimally invasive surgical (MIS) approach, which can reduce the denervation of multifidus muscle as well as reduce the incidence of intramuscular degeneration and necrosis [4,6-8]. However, patients undergoing MIS-TLIF often suffer from chronic back pain after surgery, owing to the resection of paravertebral muscles and facet joints [6,9-11].
Oblique lumbar interbody fusion (OLIF) is also an MIS procedure that uses the retroperitoneal ante-psoas surgical corridor to treat degenerative lumbar disease. The procedure has several advantages over the traditional posterior open lumbar fusion, such as easy access and decreased tissue damage [12-14]. During OLIF surgery, spine surgeons insert a large cage between the vertebrae to achieve indirect decompression through the retroperitoneal space via the interval between the psoas muscle and major vessel as assisted by a retractor [9].
An increasing variety of osteobiologic materials, including autologous and allogenic bone grafts, bone marrow aspirate, demineralized bone matrix (DBM), ceramics, and growth factors are available to the spine surgeon [5,7,15]. Autografts remain the gold standard material, displaying successful fusion rates in the treatment of degenerative lumbar disorders. However, procuring too many autogenic bone grafts may result in donor site morbidities, especially resulting in pain or infection [5,15,16]. The use of other alternative osteobiologics in spine surgery is believed to improve pain, fusion rates, and clinical outcomes [5]. At present, autogenic bone grafting has been largely replaced by allogenic bone grafting with comparable results [5,17,18]. Additionally, DBM is a widely used allogenic bone substitute, which is produced by removing cellular and mineral components from human cortico-cancellous cadaver bone, thus leaving extracellular matrix molecules, including bone morphogenic proteins (BMPs) with some osteo-inductive effect. However, a large variation is observed among the data pertaining to the success rate of spinal fusion using DBM [17].
Unlike PLIF or TLIF, which can be performed by filling the interbody cage with a local autograft, using local autografts in OLIF is not easy. At our institute, the main surgical strategy for lumbar interbody fusion is OLIF, which fills the interbody cage with DBM instead of a local autograft. In a recent systematic review and meta-analysis, the proportion of patients in the OLIF group who experienced pseudoarthrosis following the procedure was 6.1% (95% confidence interval [CI], 3.8–9.6) [19]. Xu et al. [16] demonstrated an acceptable fusion rate of single-level OLIF using pure allograft combined with posterior instrumentation. In their 2-year follow-up study, the 1-year fusion rate of 73.5% on computed tomography (CT) scans proceeded to 82.4% at the 2-year follow-up period; the fusion rate was as high as 91.2%, according to the Bridwell interbody fusion grading system on radiographic images.
However, although several studies have reported successful fusion rates after OLIF using allografts or DBM instead of autografts [5,9,13,14,16], whether OLIF can achieve satisfactory solid fusion without the use of an autograft remains unclear. Accordingly, we designed this prospective observational study to investigate the real fusion rates after OLIF using DBM, which were evaluated using both dynamic radiography and CT at 12, 18, and 24 months after surgery.
MATERIALS AND METHODS
1. Patient Enrollment
This prospective observational study involved a cohort of 79 consecutive patients who underwent minimally invasive OLIF followed by percutaneous pedicle screw fixation at a single institution between February 2017 and November 2021. All surgeries were performed by one expert spine surgeon (DCC). The study protocol was approved by the hospital’s institutional review board (KNUH 2023-10-003), written informed consent was obtained from all participants.
The inclusion criteria were as follows: adult patients (>18 years) with degenerative lumbar diseases, such as spinal stenosis, spondylolisthesis, or degenerative disc disease. All patients were treated with minimally invasive OLIF at the levels of L2–5; they underwent radiographic and clinical follow-ups for the following 1, 1.5, and 2 years after surgery. To improve the homogeneity of the data, patients who had OLIF procedures performed at 3 or more levels and those at L5–S1 were also excluded.
The exclusion criteria were as follows: patients with a history of infection, trauma, tumor, or surgery on the operated segment; co-existing diseases; drugs that affect bone metabolism; history of cancer; and incomplete follow-up data. All patients underwent preoperative imaging studies, including plain radiography, dynamic radiography, CT scans, and magnetic resonance imaging (MRI).
2. Surgical Technique
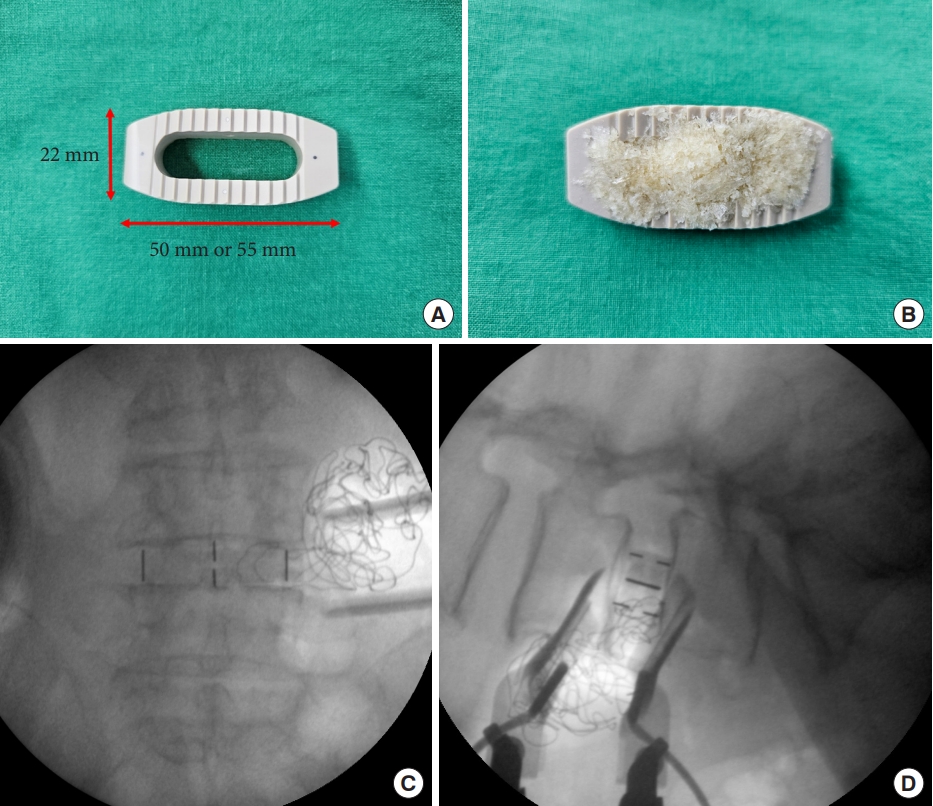
The surgical technique used for OLIF has been previously described at our institute [13,14,20]. The patients were briefly placed in the right lateral decubitus position for the left-sided retroperitoneal approach. The surgical level of the disc was marked on the skin in true lateral view under C-arm fluoroscopy. An oblique skin incision was made 3–5 cm ventral to the anterior margin of the intervertebral disc. After dissecting the 3 layers of the abdominal wall muscles, the peritoneal fat was identified. The disc annulus was exposed through an open corridor between the psoas muscle and peritoneum. At the anterior border of the psoas muscle, the plane between the disc annulus and the psoas muscle was bluntly dissected using a peanut gauze ball to not injure the psoas muscle bundle. A slight dorsal retraction of the psoas muscle was applied during tubular retractor fixation. The entire surgery was performed using a Medtronic OLIF system (Medtronic, Memphis, TN, USA) with a minimally invasive tubular retractor, fusion material (Grafton, Medtronic), and a percutaneous pedicle screw fixation system (either Sextant or Longitude system, Medtronic) (Fig. 1). Posterior decompression was not performed on any of the patients included in this study.
3. Clinical Outcome Measurements
Medical charts, imaging studies, and patient outcomes were analyzed. To estimate the clinical outcomes preoperatively, lower back and dominant leg pain were evaluated using a visual analogue scale (VAS, 0–10 points). The Oswestry Disability Index (ODI, 0–50 points) was used to evaluate the functional performance. The clinical outcomes after surgery were determined as the VAS scores for pain in the lower back and the most affected leg as well as the ODI score at 2 years after surgery.
4. Radiographic Outcome Measurements
Standing anteroposterior and lateral radiographs of the lumbar spine were obtained before surgery and at regular follow-up visits for 2 years after surgery. Dynamic views of lateral radiographs and CT scans before surgery and at 12, 18, and 24 months after surgery were collected from each patient. The results were determined by a spine surgeon who was blinded to patient information. Radiological parameters were measured in a manner blinded to the clinical results.
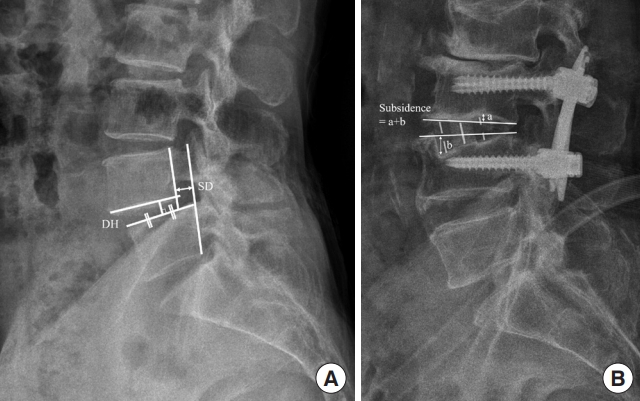
Disc height was measured as the length from the midpoint of the upper endplate of the lower vertebral body at the index level to the lower endplate of the upper vertebral body on a standing lateral radiograph. The vertebral slippage distance was defined as the distance between the extension lines of the posterior border of the vertebral bodies at the index level. The presence of subsidence was defined as the case where the sum of the subsidence of the upper and lower endplates of the cage exceeded 2 mm, thus considering the settling of the cage (Fig. 2).
5. Radiographic Assessment of Fusion by Modified Brantigan-Steffee-Fraser Scale
Radiographic assessment of fusion was performed independently by an experienced neurosurgeon (PK) and a spine fellow (SWL) in a blinded manner based on dynamic radiographs and CT scans at 12, 18, and 24 months postoperatively; the modified Brantigan-Steffee-Fraser (mBSF) scale was used for the assessments. Findings were categorized as grades I (radiographic pseudoarthrosis), II (indeterminate fusion), and III (solid radiographic fusion) [4,11,21]. Implant breakage, screw pullout, segmental movement on dynamic radiography > 2°, radiolucency (> 1 mm) around the screws, or clear absence of bridging bone on CT were categorized as pseudoarthrosis (grade I). The presence of an uncertain bridging bone, a transverse radiolucent line with a segmental movement of < 2° without implant failure, or radiolucency around the cage was categorized as indeterminate fusion (grade II). The presence of trabecular bridging bones in more than half of the fusion area on sagittal or coronal CT without movement was categorized as solid radiological fusion (grade III) (Fig. 3).
6. Statistical Analysis
All variables were subjected to standard statistical evaluation. Categorical variables were denoted by their frequency and rate; continuous variables were denoted by their mean and standard deviation. A paired t-test was utilized for analyzing continuous variables assessing significant differences, which was contingent upon the data displaying a normal distribution. Statistical significance was set at p = 0.05. All computational and analytical procedures were performed using R ver. 4.2.2 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
1. Patient Demographics
A total of 79 patients were enrolled in this study; among the patients, 25 (31.6%) were males and 54 (68.4%) were females. The patients had a mean age of 65.70 ± 7.27 years, a mean height of 159.0 ± 8.28 cm, and an average weight of 62.8 ± 9.37 kg. This resulted in a mean body mass index of 24.8 ± 2.90 kg/m². Among the cohort, 62 patients (78.5%) underwent single-level surgery and 17 (21.5%) underwent 2-level surgery. In terms of the surgical segment, L4–5 was predominant, accounting for 65.6% of the cases; this was followed by L3–4 at 31.3% and L2–3 at 3.13%. Spondylolisthesis was the primary diagnosis of OLIF (n = 69, 71.9%). Other diagnoses included spinal stenosis in 20 patients (20.8%), adjacent segment degeneration in 5 (5.2%), and others in 2 (2.1%). Of the 52 female participants whose information was collected, 3 (5.77%) were premenopausal and 49 (94.2%) were postmenopausal. The average duration of postmenopause was 12.98 ± 6.99 years. When considering smoking status, most patients (63; 79.7%) had never smoked, 14 (17.7%) had quit smoking, and 2 (2.5%) still smoked. Upon investigating for underlying diseases, hypertension was identified in 42 patients (53.2%), dyslipidemia in 26 (32.9%), and diabetes in 24 (30.4%). With regards to bone health, 35 patients (46.1%) had normal bone density, 26 (34.2%) with osteopenia, and 15 (19.7%) with osteoporosis. Complications related to the sympathetic trunk occurred in 5 patients (6.3%), which mostly improved over time, whereas pseudohernia occurred in 1 patient (1.3%). No other complications were observed. The patient demographics are displayed in Table 1.
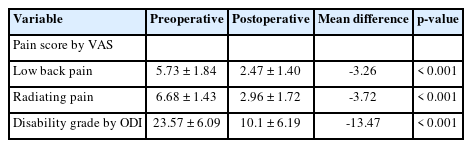
2. Clinical Outcomes
Significant improvement in postoperative clinical symptoms was observed after outcome analyses. The VAS pain score for lower back pain reduced from an average preoperative value of 5.73 ± 1.84 to 2.47 ± 1.40 postoperatively, exhibiting a significant difference with a mean of -3.26 (p < 0.001). Radiating pain displayed a similar trend, decreasing from a preoperative value of 6.68 ± 1.43 to 2.96 ± 1.72 postoperatively, with a mean difference of -3.72 (p < 0.001). The ODI, a marker for disability grade, declined from a preoperative average of 23.57 ± 6.09 to 10.1 ± 6.19 postoperatively, with a mean of -13.47 (p < 0.001). The clinical outcomes are presented in Table 2.
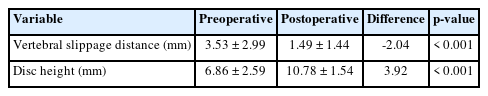
3. Radiological Outcomes
Upon evaluating the segmental parameters pre- and postoperatively, the vertebral slippage distance demonstrated a substantial reduction from a preoperative mean of 3.53 ± 2.99 mm to 1.49 ± 1.44 mm postoperatively, with a mean of -2.04 mm (p < 0.001). Additionally, disc height increased from 6.86 ± 2.59 mm preoperatively to 10.78 ± 1.54 mm postoperatively, with a mean of 3.92 mm (p < 0.001). The findings are summarized in Table 3.
In the subsequent postoperative follow-up, variations were observed between fusion rates and associated variables. At the 1-year mark, subsidence was present in 34 cases (35.4%), which increased to 46 (47.9%) at the 1.5-year mark and reached 48 (50.0%) by the 2-year mark. The dynamic angle, which was indicative of the segmental motion, steadily decreased over the given period. Specifically, 46 segments (47.9%) demonstrated angles ≥ 2° at 1 year. This dropped to 28 segments (29.2%) at the 1.5-year mark and further diminished to 17 (17.7%) at the 2-year mark. Bone bridge formation, which was indicative of successful fusion, displayed steady improvements over time. The presence of a bone bridge was recorded in 45 segments (46.9%) at the 1-year time point, escalating significantly to 71 (74.0%) at the 1.5-year mark, and further intensifying to 81 (84.4%) at the 2-year mark.
The fusion rate was evaluated using the mBSF scale grading method as previously described. The results, which comprehensively considered both the dynamic angle and bone bridge formation, were as follows: 23 segments (24.0%) were grade I at 1 year, which decreased to 6 (6.3%) at 1.5 years and 3 (3.1%) at 2 years. Grade II was observed in 42 segments (43.8%) at 1 year, which decreased to 34 (35.4%) at 1.5 years, and then dropped to 23 (24.0%) at 2 years. At the same time, grade III displayed an upward trajectory, starting at 31 (32.3%) at 1 year, increasing to 56 (58.3%) at 1.5 years, and finally reaching 70 (72.9%) at 2 years. Changes in fusion grades and long-term radiological data are summarized in Table 4.
4. Illustrative Case
An 85-year-old male presented at our spine center with complaints of lower back pain radiating to both buttocks and lower extremities. His lower back and leg pain were rated 6 and 5 on the VAS scale, respectively. He also reported intermittent claudication after walking over 100 m. Neurological examination revealed partial sensory dullness in both L5 dermatomes with the absence of motor weakness. Plain radiographic and MR studies indicated degenerative spondylolisthesis at L4 with severe central canal stenosis. The patient underwent OLIF at L4–5. The surgery was deemed successful, with temporary mild sensory dullness on the anterior side of the left thigh as the only complication. After a 2-week postoperative care, the patient was discharged to a local hospital.
The patient regularly attended outpatient follow-up appointments. Moreover, CT scans of the lumbar spine at 1- and 1.5-year postsurgery displayed gradual development of a small bone bridge, although a transverse radiolucent line remained visible. At the 2-year follow-up, the bone bridge had enlarged but had not reached the endplate of the upper vertebra. No movement exceeding 2° in flexion or extension was observed on dynamic radiographs, a condition that persisted up to the 2-year mark. Furthermore, no implant breakage, screw pullout, or radiolucency was observed around the screws during this period. No solid radiological fusion was observed. Consequently, the patient’s fusion state was classified as grade II on the mBSF scale during the 1-, 1.5-, and 2-year follow-up periods. The dynamic radiographs and CT images at the 2-year mark are depicted in Fig. 4.
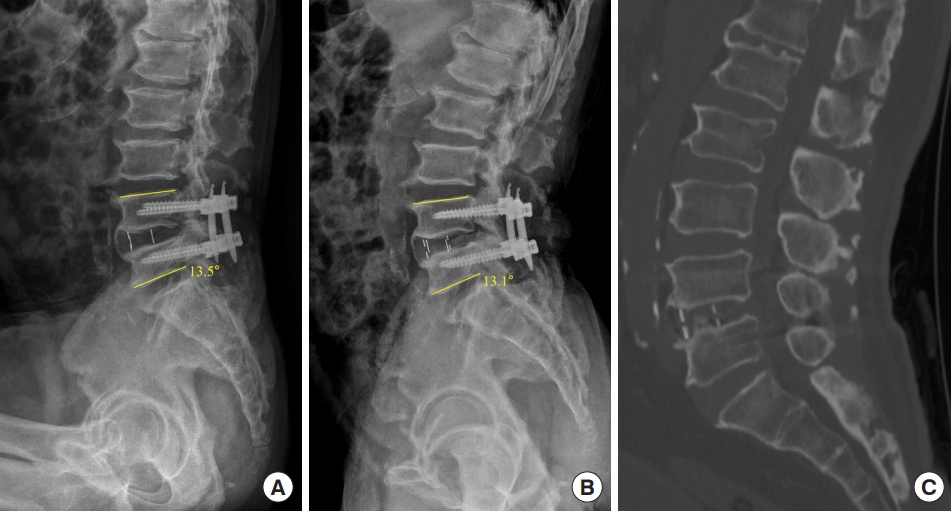
An 85-year-old male underwent an L4–5 oblique lumbar interbody fusion due to degenerative spondylolisthesis with severe stenosis at L4. (A, B) No evidence of implant breakage, screw pullout, segmental movement exceeding 2 degrees on dynamic radiographs, or radiolucency around the screws was observed. (C) By the 2-year mark, the bone bridge had not extended to the endplate of the upper vertebra. Consequently, the patient is classified as grade 2 on the modified Brantigan-Steffee-Fraser scale up to the 2-year mark.
DISCUSSION
OLIF is an MIS technique that utilizes a retroperitoneal ante-psoas corridor [13,22]; and has become the preferred surgical treatment for degenerative lumbar diseases owing to its several advantages over the traditional posterior open lumbar fusion, such as easy access and decreased back muscle damage [12-14]. For OLIF surgery, a large cage with a large window and hollow cavity can be packed with an autograft and/or allogenic bone graft, or DBM [4,17,19,23,24]. We started performing OLIF for degenerative lumbar diseases at our institute from 2016 onwards. Currently, OLIF has become the first surgical strategy for lumbar interbody fusion for patients with spinal stenosis and/or spondylolisthesis. To avoid donor site pain and morbidity, we used an allograft and DBM (Grafton, Medtronic) instead of an autograft to pack the OLIF cage.
Owing to the retroperitoneal approach, OLIF inherently carried the risks of sympathetic nerve, visceral, and vascular organ injuries as compared to other nonretroperitoneal approaches. However, as demonstrated in our study and previous studies, the frequency of such complications remains exceedingly low, and their severity tends to be minor. Although MI-OLIF can be easily and safely performed for degenerative lumbar diseases, pseudoarthrosis or delayed fusion may occur due to the absence of autograft usage. Autograft remains the gold standard graft material and has displayed successful fusion rates in the treatment of degenerative lumbar disorders [2,5,17-19,22,23,25,26].
The concept of fusion rate after lumbar interbody fusion is subject to interpretation in various studies; different studies have used nonidentical and heterogeneous criteria to assess bone fusion [11,16,21,26-28]. Many studies regarded patients without clear pseudoarthrosis as having successful fusion. Thus, this could lead to a misunderstanding regarding the real fusion rates and may result in artificially increasing fusion results upon performing different lumbar interbody fusion procedures [11,29]. Therefore, understanding the realistic fusion grade of each method remains crucial for both patients and surgeons when making informed decisions. Additionally, pseudoarthrosis is associated with poor outcomes and may require revision surgery [11,12,30].
Many different imaging techniques are used for evaluating pseudoarthrosis, including static and dynamic plain radiographs, CT scans, MRI, and bone scintigraphy [31-33]. Interpreting the fusion status is often difficult; findings are skewed by surgeon bias.
Flexion-extension radiographs are commonly used among other imaging studies; in the presence of a nonunion, detectable movement is observed within the grafted segment. However, a lack of consensus exists concerning the degree of detected movement that equates with a nonunion [34,35]. If the cutoff value of motion by dynamic radiography indicating a nonunion is increased, the fusion rates can be overestimated. In our study, we considered a movement > 2 mm on dynamic radiographs as a nonunion; we believe that this is a strict criterion for classifying detectable motion as a nonunion.
Fine-cut CT scans with reconstruction are known to have a considerably greater degree of inter- and intraobserver agreement than anteroposterior and flexion-extension radiographs. Although most observers agree when definite fusion has been achieved, the main problem in assessing fusion status with CT scans was the uncertainty of suspecting a nonunion [31]. Sugiyama et al. [33] revealed that the capacity of plain radiography alone to correctly predict fusion or pseudoarthrosis was 43%; the capacity was not improved using plain and dynamic radiography even with 43% accuracy. Additional assessments of plain radiographic techniques by reformatted CT imaging increased the capacity to predict fusion outcomes by 86%. Furthermore, Shah et al. [36] compared the accuracy of plain radiography with that of CT scans to evaluate interbody fusion following the use of titanium interbody cages. In their study, both observers identified bridging trabeculations surrounding 90% of cages on CT scans; this was only 8% on plain radiographs. Although many radiologic lumbar interbody fusion grading scales to assess solid bone fusion exist to date, none are perfect [4,11,28,37-39]. In our study, fusion was independently evaluated and subsequently categorized as solid fusion, indeterminate fusion, or pseudarthrosis using the mBSF grade scale by both dynamic radiography and CT scans [4,11].
Fogel et al. [4] assessed interbody fusion grade using the BSF scale in patients with radiolucent cages after PLIF. In their study, fusion assessment using plain radiographs and helical CT scans demonstrated equal accuracy after PLIF, which was confirmed by surgical exploration. Their results indicated that when plain radiograph films exhibited strong evidence of fusion or pseudoarthrosis, the helical CT was unlikely to provide useful new information. In contrast, many studies demonstrated that evaluating fusion rates using both radiographs and CT scans was more effective [6,32,34,40]. Therefore, in the present study, we adopted the mBSF scale with both dynamic radiographs and CT scans.
The problem with many studies published thus far is that the criteria for assessing fusion rates remain heavily diverse and heterogeneous, even with different follow-up periods. Therefore, evaluating and comparing solid fusion rates between heterogeneous studies was difficult [27,37-39,41]. In particular, among older patients with osteoporosis, the judgment for solid fusion should not be made in a short period as achieving complete fusion takes sufficient time. In our study, we believe that the 2-year follow-up period was sufficient to determine the fusion status after OLIF.
In a recent 2-year follow-up study of single-level OLIF using a pure allograft [16], the fusion rate was as high as 91.2% according to the Bridwell interbody fusion grading system on dynamic radiographs and CT scans; the clinical outcomes in patients with incomplete fusion were similar to those with complete fusion. Lin et al. [42] compared the fusion rates of OLIF and TLIF in their meta-analysis. Their results displayed a better fusion rate in the OLIF (86.2%) than in the TLIF group (79.6%) at the final follow-up (odds ratio, 1.66; 95% CI, 1.08–2.56; p = 0.02). In our study, the solid fusion rate after OLIF was 32.3% at 1 year, increasing to 58.3% at 1.5 years, and finally reaching 72.9% at 2 years. Radiographic pseudoarthrosis was 24.0% at 1 year, which decreased to 6.3% at 1.5 years and 3.1% at 2 years. The fusion rate observed in this study is somewhat lower compared to previous research. However, this is thought to be due to the adoption of a more stringent criterion for evaluation, which considered not only the formation of bone bridges on CT scans but also intersegmental movement observed in dynamic x-rays, using the mBSF scale. Nevertheless, it is noteworthy that incomplete fusion at the 1-year follow-up proceeded to complete fusion at the 2-year follow-up (Fig. 5).
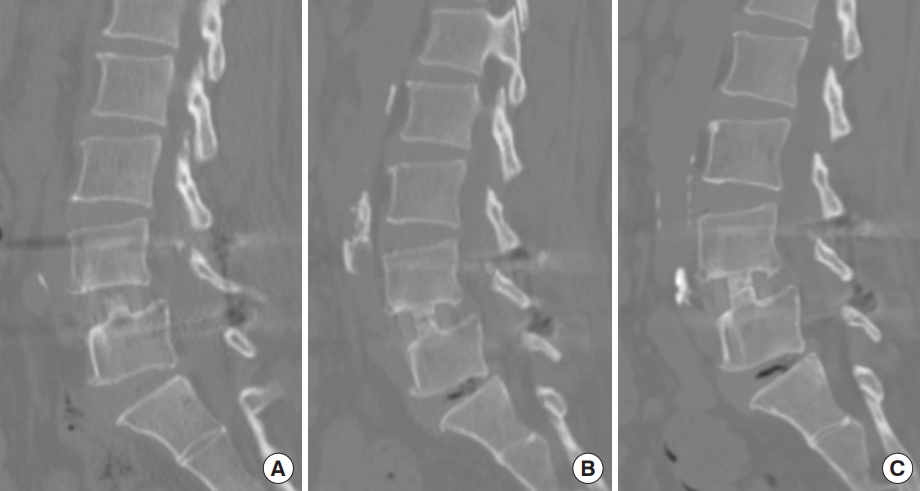
Computed tomography findings of fusion progression. (A) Bone bridge formation with minimal trabecular bridging bone at 1 year. (B) Progressive formation of a bone bridge with no solid fusion at 1.5 years after surgery. (C) Solid fusion without radiolucency around the cage at 2 years after surgery.
The fusion rates of patients after ALIF and TLIF with a minimum 2-year follow-up were evaluated in a recent study of L5–S1 fusion grade with mBSF. The solid radiographic fusion rate was higher in the ALIF group than in the TLIF group at the final follow-up, even with the use of BMP (75% vs. 47.9%, p = 0.006) [11]. Han et al. [43] analyzed fusion rates between L4–5 and L5–S1 in single-level PLIF. The radiographic fusion rates were 89.8% in the L4–5 group and 19.2% in the L5–S1 group for an average of 34 months. An inferior fusion rate in the L5–S1 group may be due to the anatomical and biomechanical differences between the L4–5 and L5–S1 levels; the local environment remains less favorable for successful bone fusion at the L5–S1 level than at other lumbar segments [2,11,30,43]. In the present study, we excluded patients with involvement of more than 3 levels and those who underwent L5–S1 OLIF surgery for comparison with other studies that have a relatively homogenous patient group.
Woods et al. [44] analyzed the complications and fusion rates after OLIF at L1–5 (OLIF25) and at L5–S1 (OLIF51). All patients were provided with anterior polyether ketone cages (Medtronic CLYDESDALE) packed with recombinant human bone morphogenetic protein-2 (rhBMP-2) (Medtronic INFUSE) and DBM (Medtronic MASTERGRAFT) mixed with bone marrow aspirate. The facets were packed bilaterally with a BMP sponge rolled over a core of DBM soaked in bone marrow aspirate. Based on a CT scan obtained at 6 months after surgery, 94.9% of the patients had successful fusion with successful fusion at 97.9% of surgical levels. All patients with pseudoarthrosis were asymptomatic and were monitored clinically. However, although it was generally agreed that the benefits of rhBMP-2 in certain populations outweigh the risks, such as those associated with poor bone quality, revision surgery, and heavy smoking, further cost-utility analyses are needed owing to the high cost of rhBMP-2.
OLIF has several advantages owing to its use of a large and long cage that can touch both sides of the apophyseal ring. A significantly large contact surface between the interbody cage and endplates can decrease the cage subsidence after OLIF surgery [4,17,19,23,24]. In our study, we used a polyetheretherketone (PEEK) cage (Medtronic CLYDESDALE) with a 22-mm width and a 50-mm length; the PEEK cage had a contact surface area twice larger than that of conventional PLIF or TLIF cages. At the 1-year mark, subsidence was present in 34 cases (35.4%), which increased to 46 (47.9%) at the 1.5-year mark and reached 48 (50.0%) at the 2-year mark after OLIF surgery. These findings indicated a relatively higher subsidence rate as compared with other studies. We measured subsidence by taking both the upper and lower endplates of the cage into account. This suggested that our criteria for identifying subsidence might be more stringent than those used in other studies [14,16,45,46]. Therefore, we believe that a high number of participants may be classified as having subsidence during the study period.
This study has certain limitations. This study was conducted on a relatively limited number of patients and exhibited sex disparities in the cohort. The surgical level was restricted to L2–5; the cohort only included patients operated at 2 levels or less. Due to these specific cohort attributes, this study may not fully represent the general population.
CONCLUSION
OLIF is a safe and effective surgical procedure for the treatment of degenerative lumbar diseases. The mBSF scale, which simultaneously evaluates both dynamic angles and bone bridge formation, offers great reliability for the radiological assessment of fusion. OLIF using allografts and DBM, which is performed on at least one or 2 levels at L2–5 can achieve satisfactory fusion rates within 2 years after surgery.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean Government (MSIT) (NRF-2022R1A2C1092952).
Author Contribution
Conceptualization: DCC; Data curation: Sangseok L, JWJ, SWL, KTK, HDK, YSK, PK; Formal analysis: Sangseok L, SWL, KTK, Subum L, PK; Funding acquisition: DCC; Methodology: Sangseok L, SWL, PK, DCC; Project administration: PK, DCC; Visualization: JWJ; Writing - original draft: Sangseok L; Writing - review & editing: Sangseok L, JWJ, HDK, DCC.