Modified Open-door Laminoplasty Using Hydroxyapatite Spacers and Miniplates
Article information
Abstract
Objective
Cervical laminoplasty has been widely accepted as one of the major treatments for cervical myelopathy and various modifications and supplementary procedures have been devised to achieve both proper decompression and stability of the cervical spine. We present the retrospectively analyzed results of a modified unilateral open-door laminoplasty using hydroxyapatite (HA) spacers and malleable titanium miniplates.
Methods
From June 2008 to May 2012, among patients diagnosed with cervical spondylotic myelopathy and ossification of posterior longitudinal ligament, the patients who received laminoplasty were reviewed. Clinical outcome was assessed using Frankel grade and Japanese Orthopaedic Association score. The radiologic parameters were obtained from plain films, 3-dimensional computed tomography and magnetic resonance images.
Results
A total of 125 cervical laminae were operated in 38 patients. 11 patients received 4-level laminoplasty and 27 patients received 3-level laminoplasty. Postoperatively, the mean Frankel grade and JOA score were significantly improved from 3.97 to 4.55 and from 12.76 to 14.63, respectively (p<0.001). Radiologically, cervical curvature was worsened from 19.09 to 15.60 (p=0.025). The percentage of range of motion preservation was 73.32±22.39%. The axial dimension of the operated spinal canal was increased from 1.75 to 2.70 cm2 (p<0.001).
Conclusion
In the presenting study, unilateral open-door laminoplasty using HA spacers and miniplates appears to be a safe, rapid and easy procedure to obtain an immediate and rigid stabilization of the posterior elements of the cervical spine. This modified laminoplasty method showed effective expansion of the spinal canal and favorable clinical outcomes.
INTRODUCTION
After the introduction of the laminoplasty by Hirabayashi in 19779), the expansive open door laminoplasty has become a widely adopted surgical procedure for treating multilevel cervical spondylotic myelopathy (CSM), ossification of posterior longitudinal ligament (OPLL), spinal cord injury without fracture and dislocation with cervical spinal stenosis. Thereafter, various techniques for cervical laminoplasty were reported by several authors. Based on the results in these reports, laminectomy has been widely replaced by laminoplasty6,7,8,9,10,11,16,17,21,22,26).
Laminoplasty is usually classified as open door (single door) or double door (French door). Since then, various modifications and supplementary procedures have been devised for further improvement of safety and efficacy of the decompression and for stability of the spine.
Traditional laminoplasty has proven effective in resolving neurological symptoms. However, because of the absence of rigid fixation, secondary narrowing of the spinal canal and neurological deterioration over the long-term follow-up2,14), several types of rigid fixation have been introduced in an attempt to improve the surgery. Plate fixation combined with bone struts and ceramic spacers, or spacers alone, or plate fixation alone has also been used during laminoplasty to construct a complete laminar arch5).
Plate fixations alone are technically facile to insert. However, the absence of bone healing on the open side, cannot achieve the goal of recreating a stable laminar arch without solid bony union on the hinge side28). Bone struts and ceramic spacers have a benefit that they can recreate a lamina arch, as bony healing can occur on both the grafted side. However, it has a risk associated with graft kickout, which causes reclosure of the lamina and root or cord compression by spacer dislodgement into the spinal canal12,23).
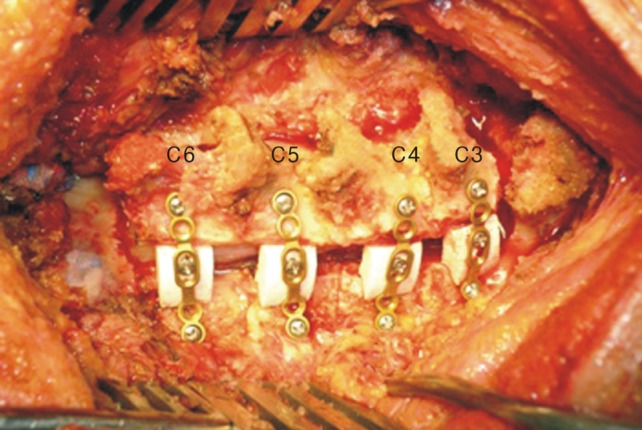
We have used a modified unilateral open-door laminoplasty using hydroxyapatite (HA: HOYA Corporation PENTAX, Tokyo, Japan) spacers and malleable titanium miniplates (Fig. 1). And we retrospectively analyzed its clinical and radiological results.
MATERIALS AND METHODS
We retrospectively reviewed the outcome of consecutive 38 patients who underwent modified unilateral open-door laminoplasty using HA spacers and malleable titanium miniplates between June 2008 and May 2012. There were 29 men and 9 women who ranged in age from 38 to 77 years (mean 55.2 years). CSM was present in 23 patients and OPLL was present in 15 patients. Of these, 17 patients had a history of trauma and 21 patients showed symptoms of cord compression without a history of trauma. For patients with a history of trauma, those who do not have a fracture or dislocation of the cervical spine were selected for the study. Mean follow up duration was 14.39 months (range 6-39 months).
Patient's neurological status was evaluated using the Frankel scale3) just before surgery and at the final visit. In this scale, the maximum score is 'E' (normal motor, sensory function) and the minimum score is 'A' (absent motor, sensory function). We calculated a scale of 1 to 5 (1=A, 2=B, 3=C, 4=D and 5=E). The presence of myelopathy was assessed using Japanese Orthopaedic Association (JOA) scale just before surgery and postoperative final visit. In this scale, the maximum score is 17 and the minimum score is 0. Recovery from myelopathy at postoperative final visit was calculated using the formula: (Postoperative final visit JOA scale-Just before surgery JOA scale)/(17-Just before surgery JOA scale)8).
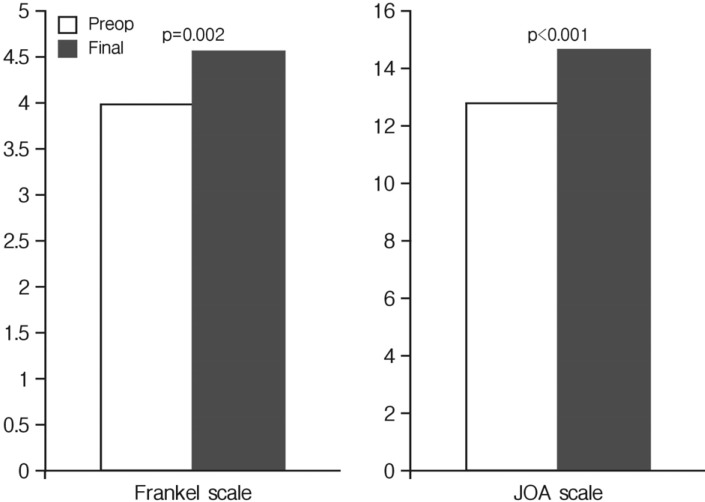
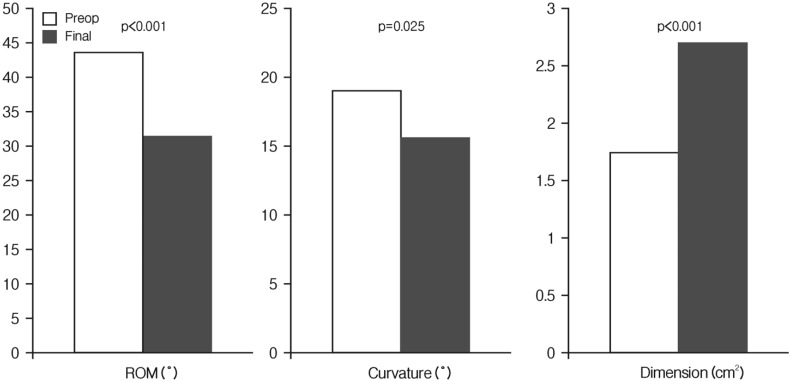
Radiologic evaluations of the cervical spine included plain radiography at preoperative, 1, 2, 4, 6, 12 months after surgery to assess for curvature of the cervical spine (Fig. 2), and 3-dimensional computed tomography (3-D CT) scans at 12 months after surgery to assess for dimension of the cervical spinal canal and HA position, implant-related complications (Fig. 3). And evaluation of the cervical spine magnetic resonance imaging was performed at 12 months after surgery to assess for expansion of dural sac and decompression of spinal cord.
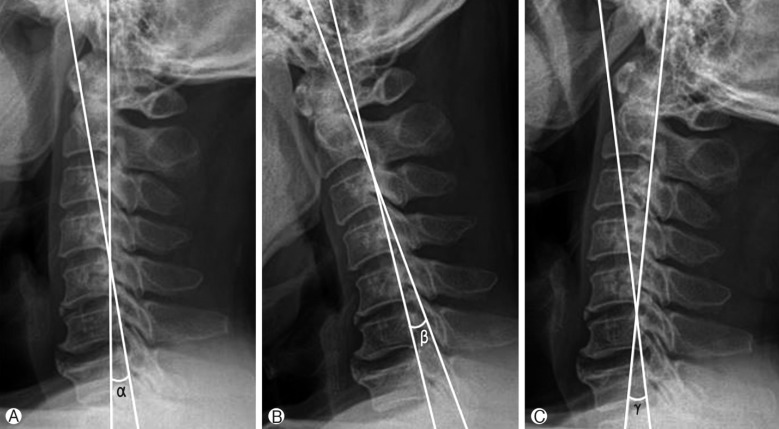
Line drawing showing the method of measurement of the cervical curvature and ROM of the cervical spine in the plain radiographs. Two lines are drawn along the posterior borders of C2 and C7 in the neutral (A), flexion (B), and extension (C) positions. The angle formed at the crossing point of these two lines is measured in each position. The angle in neutral position is expressed as cervical curvature (α), and the sum of cervical curvatures at maximum flexion (β), and maximum extension (γ) as the ROM. ROM; Range of motion.
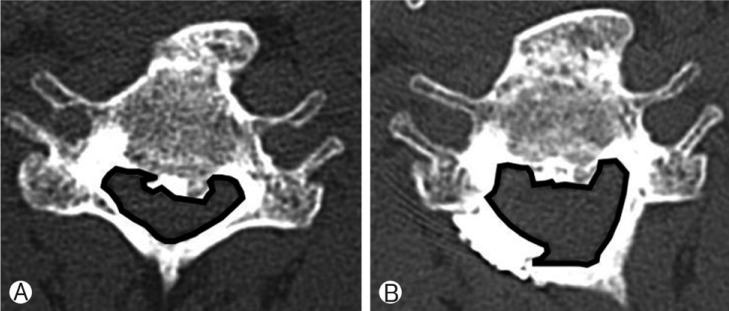
Spinal canal dimension measurements (inside the black line) in axial CT images: Preoperative (A) and postoperative (B) axial CT images.
The curvature of the cervical spine was measured by the angle formed by two lines extending from the posterior borders of the C2 and C7 vertebral bodies in the neutral position13), and the range of motion (ROM) was measured by the summation of the cervical angles in flexion and extension (Fig. 2)13). The axial dimension of the cervical spinal canal was measured at the same lamina level on the axial CT image at preoperative and 12 months after surgery, and the number of pixels of spinal canal was calculated by Image J program version 1.47 (NIH, USA) (Fig. 3).
1. Operative Technique
All surgical procedures were performed with patients in prone position in slightly flexion of neck in a Mayfield head fixator. A standard posterior midline approach allowed exposure of the cervical laminae at the targeted operative levels and laterally to the facet joints. Trough preparation in the hinged and opening sides of the laminofacet junction was performed with high-speed drill and Kerrison punch. From rostral to caudal, each lamina was gently lifted using Raney appliers. And after selecting proper size of HA laminar spacer (10mm or 12mm), the selected HA spacer and a malleable titanium miniplate was assembled using a miniscrew(6 mm) (Fig. 3). Each lamina was secured with the assembled HA spacer and miniplate complex using another miniscrews (6 mm) (Fig. 4).
2. Statistical Analysis
Parameters were analyzed using the Mann-Whitney U-test. Differences were considered significant when p-values were <0.05. All results are expressed as mean±Standard deviation (SD). Analyses were performed using the IBM Statistical Package for the Social Sciences version 18.0 (SPSS Inc., Chicago, IL).
RESULTS
The 38 patients who underwent 'modified unilateral opendoor laminoplasty using HA spacers and malleable titanium miniplates' are summarized in Table 1. In total, 125 cervical laminae were operated in 38 patients. And the number of laminoplasty levels ranged from 3 to 4 (mean 3.29). Eleven patients received 4-level laminoplasty and 27 patients received 3-level laminoplasty. Of these, 9 patients underwent additional anterior cervical discectomy and fusion (ACDF) due to marked herniated nucleus pulposus.

Basal characteristics of 38 patients who underwent modified open-door laminoplasty using hydroxyapatite spacers and miniplates
The mean operation time was 226.1min (110-465min), and the mean volume of intraoperative blood loss was 715.5 cc (350-1,500 cc). But if excluding the patients with ACDF, the operation time was 185.9 minutes.
1. Clinical Outcome
Postoperatively, the mean Frankel scale was improved from 3.97 to 4.55 (p=0.002) (Fig. 5). And mean JOA scale was also increased from 12.76 to 14.63 with mean calculated recovery rates of 62.82±40.57%. There was a statistically significant increase of postoperative final visit JOA scale (p<0.001) (Fig. 5).
2. Radiological Outcome
Neuroimaging data were obtained in the 38 patients who were followed up more than 6 months postoperatively. Postoperative MR imaging revealed good expansion of dural sac and decompression of spinal cord in minimum follow up period of 1 year in all patients. Postoperative 3-D CT scanning demonstrated reconstructed laminae in satisfactory position (Fig. 6). There were no implant-related complications such as breakdown or dislocation of HA implants, delayed dural laceration in any case. And stability/fusion of the reconstructed laminae was found at minimum follow up period of 1 year in all patients.

Representative sagittal T2-weighted MR images of operated patient obtained from preoperatively (A) and postoperatively (B). Follow up 3-D CT scan (C) confirmed properly inter-positioned hydroxyapatite spacers at C3, C4, and C5.
Postoperatively, the overall cervical ROM was changed from 43.93±9.20° to 31.60±10.24° (p<0.001). The percentage of ROM preservation was 73.32±22.39%(Fig. 7). The lordotic curvature of the cervical spine was decreased from 19.09° to 15.60° (p=0.025). The difference of pre- and postoperative curvature of the cervical spine was ranged -3.50±8.64° (Fig. 7) Postoperative kyphotic deformity, however, was not observed in our series. The axial dimension of the cervical spinal canal was significantly improved from 1.75±0.48 cm2 to 2.70±0.58 cm2 (p<0.001) (Fig. 7).
DISCUSSION
Laminoplasty is usually classified as open door (single door) or double door (French door)25). The single open door laminoplasty can be divided into classical suture fixation and titanium miniplate fixation25). There have been various modifications and supplementary instruments for laminoplasty to maintain hinge patency and provide secure fixation. For example, there are HA spacer, ceramic lamina, miniplate osteosynthesis, and allogenic or autogenous bone grafting33). The classical suture fixation is not only technically difficult but also do not provide rigid fixation. Furthermore, the neurological deterioration due to re-closure of opened lamina which is associated with cutout, breakage or stretching over time has been reported8,25,28). In one series using only suture fixation, up to 34% of patients demonstrated some degree of re-closure at one or more levels19). Also, the titanium miniplate fixation has a risk of dislodgement19). Allogenic or autogenous bone graft and a ceramic block have been used for the maintenance of opened lamina. These spacers have advantages such as a bony healing of the grafted side and maintenance of the laminar arch. But, they have a disadvantage such as root or cord compression due to graft kickout12,23,30).
We found that our surgical technique was relatively easy compared with other techniques such as classical open-door laminoplasty and double-door laminoplasty5,8,9,24). Because making "small" holes and sutures on the lateral masses in the deep operative field and bone grafting was not necessary, laminoplasty-associated morbidities like graft kickout and spacer dislodgement were not observed in our series.
While laminoplasty can provide sufficient decompression of the cervical spinal cord, preserving the motion of cervical spine, consistent reconstruction of the expanded laminae of the vertebral arches is needed for clinical recovery from the symptoms and to prevent postoperative kyphosis of the cervical spine and adhesion of scar tissue. A sinking or nonunion of the expanded laminae may lead to neurologic regression, segmental motor paralysis. A laminoplasty method should be technically simple, safe and provide immediate strong and rigid fixation. So it is important to successful reconstruction of the lamina after laminoplasty30).
Though, laminoplasty relatively preserves the posterior elements compared with laminectomy, postoperative decrease of ROM was frequently described27). There are several reported reasons for decrease of ROM after laminoplasty. Seichi et al. reported that only 22% of preoperative ROM was maintained after laminoplasty. These authors also mentioned that the loss of ROM after laminoplasty was caused by unexpected fusion of the facet joints29). The high fusion rate in their series may have occurred because they used iliac crest as struts for the laminoplasty.
Machino et al. reported that 88% of preoperative ROM was maintained after a laminoplasty preserving the C2 muscle and active rehabilitation18). Fujimori et al. reported that ROM preservation rate was 75% in the CSM group, and 61% in the OPLL group. In their study, the loss of ROM was caused mainly by a decrease in the extension angle in both groups. They assumed that this restriction of extension may have occurred partly as a result of impingement of the opened lamina because the spinous processes were preserved in all their cases. Another reason would be scarring of the cervical extension muscles4). Meyer et al. noted that plated laminoplasty led to a loss of ROM in extension20). In our study, the percentage of ROM preservation was 73.32±22.39%. We assume that this decrease of ROM may have occurred partly as a result of impingement of the opened lamina and leading to mild restriction of extension.
Recently, several authors have presented new technique of cervical laminoplasty using hydroxyapatite laminar spacers and titanium miniplates. Tanaka et al. reported that hardware failure or screw loosening did not occur during 36.3 months mean follow-up period after a single open door laminoplasty using hydroxyapatite laminar spacers and titanium miniplates in 22 patients31). Goto et al. reported that hardware failure or screw loosening did not occur during 24.3 months mean follow-up period after a single open door laminoplasty using hydroxyapatite laminar spacers and titanium miniplates in 25 patients5). We first fixated the lifted lamina with spacer at the laminofacet junction before screw fixation. Due to stable lamina manipulation during the operation, it has less possibility of cord injury and prevents over-lifting of laminae. As it is once more fixed with miniplate, it helps to maintain continuous expansion of lamina. We suggest that it is not only technically safe, but also provides stable reconstruction, which can be an alternative method to avoid re-closure and dislodgement.
The main component of HA spacer is hydroxyl compound of calcium phosphate that produces natural bone matrix. In the last 20 years, it has been used efficiently as oral, plastic, otological and orthopedic surgery instead of bone. It is known to have biocompatibility and safety5).
Some authors used synthetic HA for cervical interbody fusion15,17). Some experimental studies reported successful bone healing around HA by bone ingrowth into the pores and formation of bridging bone on the surface of the implant, proving osteoconduction1,32). In comparison with autografts, HA space has many advantages such as good biomechanical stability, reductions in operation time, blood loss, and donor site morbidity24).
The laminae could be solidly fixed without using the soft malleable miniplates, because there existed no space between bone edge of lamina and HA spacer. Since there is no gap between bone edge of lamina and HA spacer, the laminar space is the main structure that takes the mechanical force compressing laminae vertically or laterally. The spacer was helped to decrease the force to miniplate. Also, malleability of miniplates helped in cutting down the force to screws. Goto et al. described that the screw loosening was more frequently occurred in cases in which only hard miniplates were used for laminar fixation without spacers because the miniplate and screws directly bear the stability of the laminae5). In our study, we found no implant-related complications in any case documented during the follow-up period.
Our technique has drawbacks, such as additional cost of spacer, supplement time for spacer and plate assembly. Another shortcomings of this study include the small patient population and the brief follow-up duration. Nevertheless, it has advantage compared with 'plate alone technique' and 'spacer alone technique'. HA spacer generates bone healing at the open side of lamina and it can reduce complication due to 'graft kickout' as HA spacer fixed to plate. Future studies, enrolling more patients with longer periods of follow-up, will be necessary to evaluate postoperative axial pain and the longterm stability.
CONCLUSION
Unilateral open-door laminoplasty using HA spacer and miniplates appears to be not only a safe, rapid, and easy procedure but also an efficient method by which to obtain an immediate, rigid stabilization of the posterior elements of the cervical spine after laminoplasty.