Lumbar Disc Herniation in a Patient With Congenital Vertebral Body Anomaly: A Case Report
Article information
Abstract
Lumbar disc herniation is characterized with low back and leg pain resulting from the degenerated lumbar disc compressing the spinal nerve root. The etiology of degenerative spine is related to age, smoking, microtrauma, obesity, disorders of familial collagen structure, occupational and sports-related physical activity. However, disc herniations induced by congenital lumbar vertebral anomalies are rarely seen. Vertebral fusion defect is one of the causes of congenital anomalies. The pathogenesis of embryological corpus vertebral fusion anomaly is not fully known. In this paper, a 30-year-old patient who had the complaints of low back and right leg pain after falling from a height is presented. She had right L5-S1 disc herniation that had developed on the basis of S1 vertebra corpus fusion anomaly in Lumbar computed tomography. This case has been discussed in the light of literature based on evaluations of Lumbar Computed Tomography (CT) and Magnetic Resonance Imaging (MRI). This case is unique in that it is the first case with development of lumbar disc herniation associated with S1 vertebral corpus fusion anomaly. Congenital malformations with unusual clinical presentation after trauma should be evaluated through advanced radiological imaging techniques.
INTRODUCTION
Walter Dandy was the first research to describe radicular pain as an extradural mass associated syndrome in 19293). Mixter and Barr, however, reported in 1934 that extruded disc materials cause sciatic pain and described the surgical approach11).
Intervertebral disc degeneration18), smoking, occupational and sports-related physical activity, microtrauma, such as obesity, environmental factors covered by the different forms of life12), genetic factors1), congenital defects of vertebral formation16) are involved in the etiology of lumbar disc herniation. The disc herniation depending on vertebral corpus developmental anomaly is available only one case in English Literature. Our case is the second in such nature.
CASE REPORT
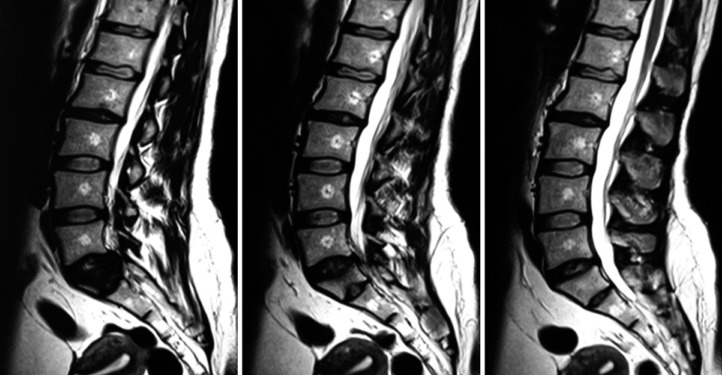
A thirty-year-old female patient was admitted to our clinic with complaints of low back and right leg pain after a fall 3 weeks ago. Physical examination was evaluated as normal and there were not any features identified in family history. The neurological examination was described as right straight leg raising test positive at 45 degrees, full muscle strength, norm active tendon reflexes, right S1 dermatome hypoesthesia. Lumbar computed tomography (CT) was planned because S1 lumbar vertebra fracture was suspected in the lumbosacral graph AP/L (Fig. 1) based on history of trauma. Lumbar magnetic resonance imaging (MRI) was performed as fusion anomaly was detected but S1 vertebral corpus was not broken on the lumbar CT (Fig. 2). L5-S1 right paramedian disc herniation was detected with the precipitation of trauma on the lumbar MRI (Fig. 3, 4). Development of the spinal canal due to congenital defects in the lumbar MR imaging was normal (Fig. 5). The patient did not consent to surgical treatment and was referred to Physical Therapy clinic for conservative treatment. The patient's complaints decreased with physical therapy after 3 weeks.

In magnified view of AP lumbosacral graphy, there was a right paramedian bone defect in S1 vertebrae.
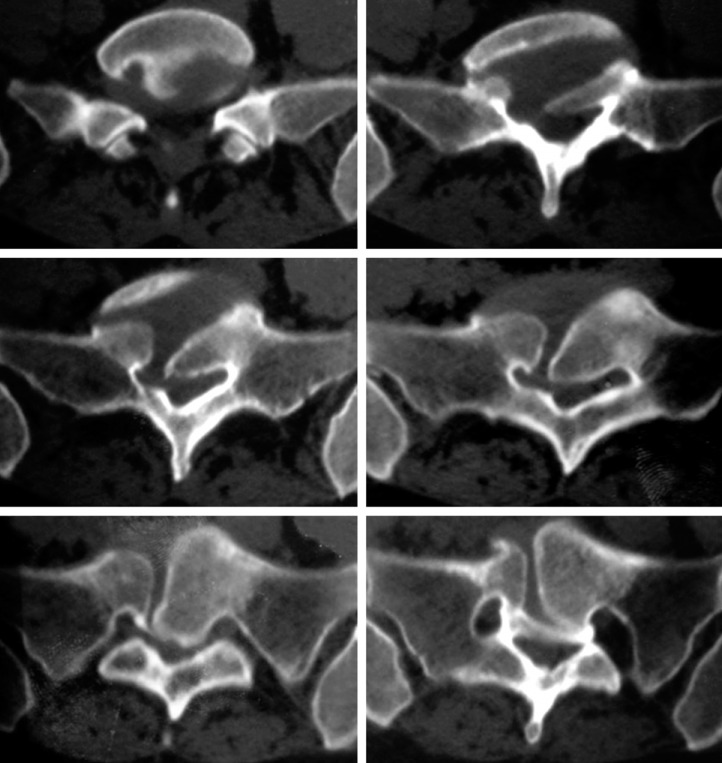
Lumbar computed tomography axial images show the fusion anomaly of S1 vertebrae corpus with sclerotic margins. The gap between non-fused corpus was filled with soft tissue which has the same density as that of intervertebral disc.
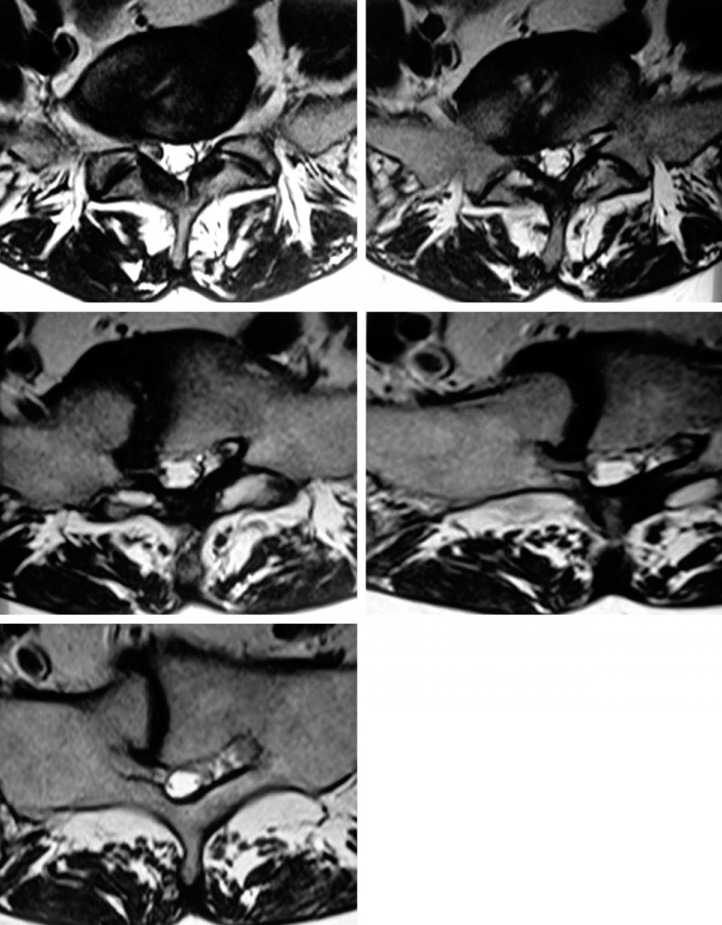
T2-weighted axial magnetic resonance images confirm the dark signal of disc that fills the gap completely and the herniation to the right S1 foramina.
DISCUSSION
Disc herniation occurs as a result of displacement of lumbar intervertebral disc annulus fibrosis and nucleus polyposis fibrosis in the vertebral canal7). Lumbar disc herniation can be symptomatic as a result of compression on the spinal nerves or roots. Radicular symptoms occur due to generation of nerve root ischemia because of the direct mechanical effect of the herniated disc material, or with an inflammatory response and the effect of secondary edema and compression of vascular structures9).
In the etiology of the disease, cumulative microtrauma was held responsible and it is reported to be more frequently encountered in those driving motor vehicles, those with sedentary life style and in smokers12). Disc herniation triggered by congenital lumbar vertebra anomaly is a rare occasion16).
Congenital vertebrae corpus defects are rare anomalies. These anomalies are classified as disorders of formation, segmentation disorders and the composition of the two complex disorders5). Although the pathophysiology of spina bifida can be described, the embryological pathogenesis of vertebral corpus fusion anomaly is not fully known.
Mesoderm structure emerges after the second week of embryological development of the vertebrae that make up the spine. Skeletal system develops from the para-axial mesoderm and the lateral plates (somatic layer), and crista neuralis. Paraaxial mesoderm creates a series of segmented tissue block known as the somite towards caudal from both sides of the neural tube, somatomeres and occipital region. Somite differentiates in ventromedial termed as sclerotome and dorsolateral part termed dermomyotome10).
The position of the sclerotome cells changes to surround the notochord and the spinal column in the fourth week of development. This positional change occurs with the differentiation of surrounding structures and not the active migration of those sclerotome cells13). Thus, the resulting mesenchymal column retains segmental traces by leaving less-dense areas containing intersegmental arteries of sclerotomies blocks. The caudal part of each sclerotome segment is heavily divided and collected in the ongoing stages of development. This division is so intense that it moves towards the environment intersegmental tissue and thus, a caudal part of the sclerotome is connected to cephalic part of another sclerotome. Thus, vertebral body becomes intersegmental with the connection of intersegmental tissue and the pre-cartilaginous vertebra body10). Among sclerotomes that are poor in cell count in cranial and rich in cell count in caudal forms, the one that contains the poo r area forms the intervertebral disc, while the one that contains the rich area constitutes a section of vertebral body10). These formation defects occurring in the embryological period cause anomalies regarding the vertebra and the disc10). Among congenital vertebral anomalies, double facet joint formation8), the absence of pedicle17), and absence of lumbar articular processes are reported; however, vertebral corpus fusion defect as in our case was reported before only one time2). Cho and friends described vertebra fusion anomaly as the butterfly vertebra2). Butterfly vertebra is an uncommon congenital disorder characterized by a symmetrical fusion defect resulting in a sagittal cleft vertebra2). Our case is vertebra fusion anomaly too, but not symmetrical.
Intervertebral disc was filled due to the lack of development of annulus fibrosis in cavity associated with the defect of embryological development of the vertebral corpus and trauma as a result of weakness in our case and it caused the patient to develop lumbar disc hernia. Therefore disc herniation could occur more easily in patients with vertebral body defect than in patients with normal vertebral body. Congenital vertebra corpus fusion anomalies are typically asymptomatic. However, these anomalies incidentally detected during routine radiographic investigations and post-traumatic radiological evaluations6). The specific radiological examinations usually include direct roentgenogram, CT and MRI15). In our case, vertebral fusion defects were determined with lumbar radiograph performed due to back pain after trauma. Lumbar CT and MRI were taken in pursuit of radiograph. We thought that the defect occurred during the development in the embryological period of the vertebral body. However, that intervertebral disc was the weakest link as sufficient circular annulus fibrosis had not developed here. Thus annulus fibrosus resulted in herniation after the trauma depending on the weakness. There were no other osseous pathologies such as spina bifida occulta, facet abnormalities, and/or pedicle anomaly in our case.
Disc herniation in patients with congenital bone deformities associated with congenital developmental defects are considered related problems in the spinal canal. On the level of the patient's filum terminale, whether tethered cord syndrome should be investigated14). There was not a congenital defect of development of the spinal canal in our case (Fig. 5). Presenting with similar symptoms, such as back and leg pain, especially adult clinical presentation patients with lumbar disc herniation group tethered cords can be confused with tethered cord. And therefore Lumbar MRI examinations should be well evaluated in the preoperative period4).
CONCLUSION
These types of cases after trauma can be misevaluated and overlooked as congenital malformation without treatment. Especially, patients with congenital malformations and an unusual clinic should be examined carefully with advanced radiological imaging techniques.