The Effect of Different Pillow Heights on the Parameters of Cervicothoracic Spine Segments
Article information
Abstract
Objective
To investigate the effect of different pillow heights on the slope of the cervicothoracic spine segments.
Methods
A prospective analysis of data from 16 asymptomatic adults (aged 20 to 30 years) was carried out. Exclusion criteria were history of injury or accident to the cervicothoracic spine, cervicothoracic spine surgery, or treatment for neck symptoms. We used three different pillow heights: flat (0 cm), 10-cm, and 20-cm pillows. Cervical sagittal parameters, measured with radiography, included; C2-7 Cobb's angle, T1 slope (T1S), thoracic inlet angle (TIA), and neck tilt (NT). Statistical analyses were performed using Spearman correlation coefficients.
Results
As the height of the pillow increased, the T1S & C2-7 Cobb's angle increased while the NT values tended to decrease. The TIA values, however, remained constant. Additionally, there was a statistically significant sex difference in T1S with the 0-cm pillow (p=0.01), and in NT with the 20-cm pillow (p=0.01).
Conclusion
From the data obtained in this study, we recommend that the most suitable pillow height is 10 cm, considering the normal cervical lordosis.
INTRODUCTION
Many patients present with symptoms related to the cervicothoracic spine, such as neck pain, scapular pain, and headaches7). Changing pillows can significantly relieve cervical pain, scapular pain, and headaches25679), although many people appear to have made poor pillow choices, as low pillow comfort and cervicothoracic symptoms upon waking are commonly reported4). While patients continue to seek advice on pillow choice, there has been limited research to assess the effects of varying pillow heights on cervical spine posture. As such, appropriate recommendations cannot as yet be made.
This study reports the effects of three different pillow heights on the slope of the cervicothoracic spine segments when resting in the supine position.
MATERIALS AND METHODS
1. Study Participants
A cohort of 16 asymptomatic adult volunteers, aged between 20 and 30 years, were enrolled in this study. All participants provided written informed consent prior to inclusion. We included individuals who had no history of any spinal diagnosis, symptoms, or treatment, and excluded cases where there was an accident or injury to the cervicothoracic spine in the preceding year. Patients currently receiving treatment for neck symptoms were also excluded.
2. Preparation and Test Position
Participants were permitted to sit up briefly to stretch and move their necks between each pillow trial. Participants assumed a standard supine position with their head resting on the pillow with the external occipital protuberance at the center of the pillow. Participants lay with their eyes facing the ceiling.
3. Analysis of Simple Radiographs
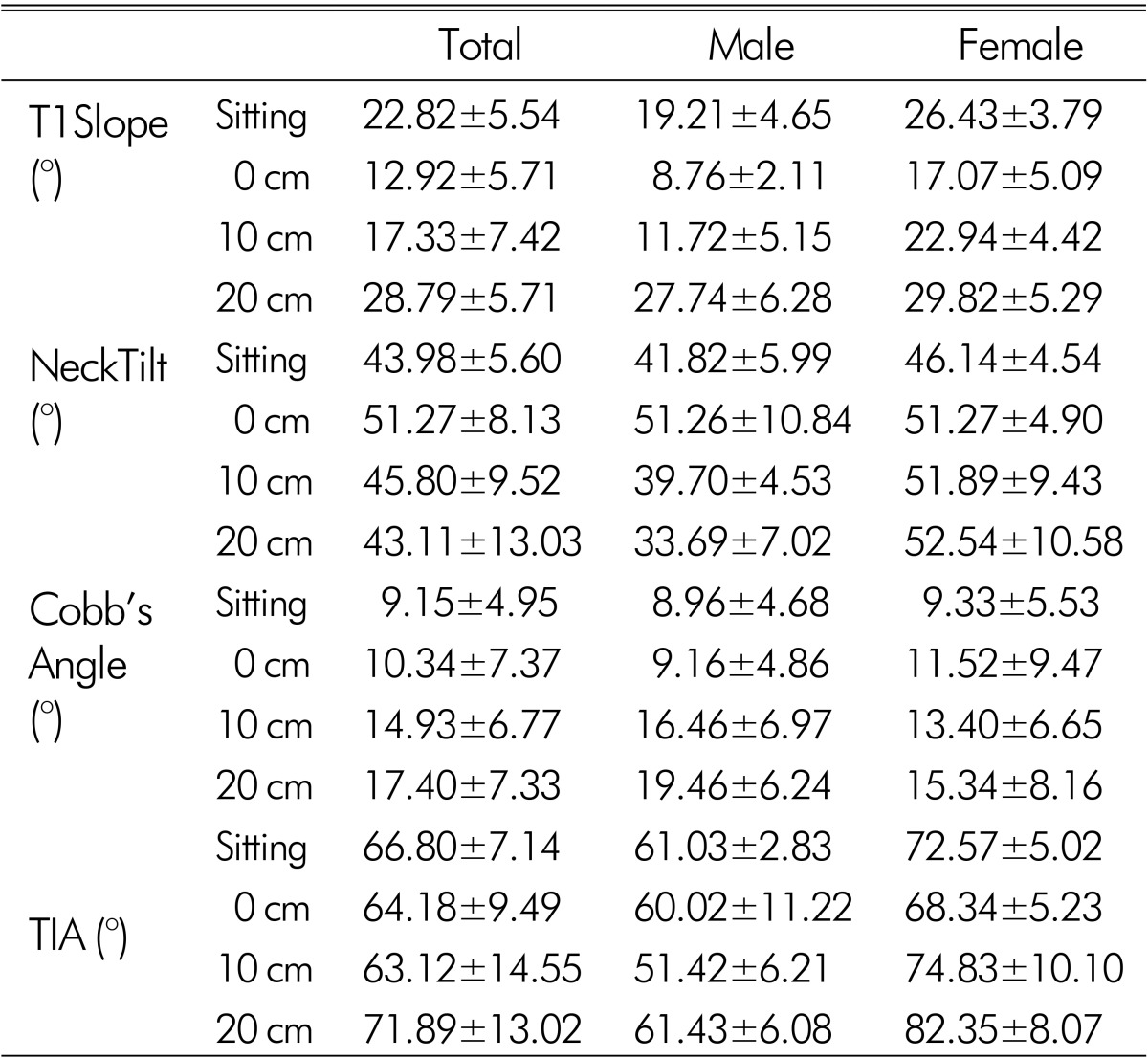
We measured four morphological parameters. These parameters consisted of the thoracic inlet angle (TIA), T1 slope (T1S), neck tilt (NT), and C2-7 Cobb's angle. As depicted in Fig. 1, the TIA was considered the angle formed by a line from the center of the T1 upper endplate (T1UEP) vertical to the T1UEP, and a line connecting the center of the T1UEP and the upper end of the sternum. The T1S was defined as the angle formed between the horizontal plane and the T1UEP. The NT was defined as the angle formed by a line drawn in the upper end of the sternum and a line connecting the center of the T1UEP and the upper end of the sternum. The C2-C7 angle was measured by the formal Cobb methods as the angle between the horizontal line of the C2 lower endplate and the horizontal line of the C7 lower endplate (Fig. 1 and 2).
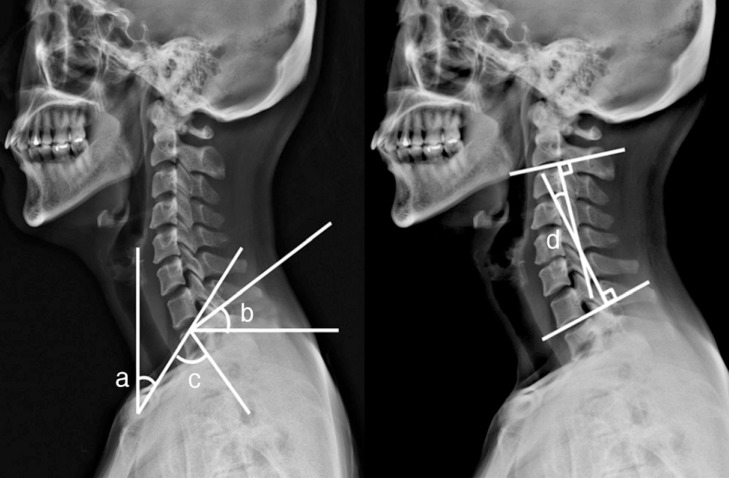
Schematic drawing of the measured angles of the cervicothoracic spine segments. a: Neck tilt; b: T1 slope; c: Thoracic inlet angle; d: C2-7 Cobb's angle.
4. Statistical Analysis
The PACS system(p view, INFINITT, Seoul, Korea) was determined by one observer for the measurement. Each parameter was independently measured twice. The mean and standard deviations of all measurements were calculated.
Correlations between parameters of interest in this study were analyzed with the Mann-Whitney test and Spearman coefficients. All statistical analyses were performed using SPSS (version 18.0, SPSS, Chicago, IL, USA). Data are presented as mean±standard deviation. A p<0.05 was considered statistically significant.
RESULTS
The mean ages of the study participants were 29.38±2.23 and 29.25±3.11 years for men and women, respectively. Table 1 shows the mean values for each of the measured parameters stratified by sex. With a greater pillow height, the T1S and C2-7 Cobb's angle seen on radiographs were greater. For pillow heights of 0, 10, and 20 cm, the T1S were 12.92±5.71°, 17.33±7.42° and 28.79±5.71°, respectively; and the C2-7 Cobb's angles were 10.34±7.37°, 14.93±6.77°, and 17.40±7.33°, respectively. Additionally, with increasing pillow height, the NT value tended to decrease, and the TIA values remained constant with the 0 cm and 10 cm pillow. However, the TIA values with 20-cm pillow were different from the other pillow heights.
The TIA with the 10 cm pillow had a significant correlation (p<0.05) with the T1S with the 10 cm pillow(r=0.829) and the NT with the 10 cm pillow(r=0.812). In addition, the TIA with the 20 cm pillow had a significant correlation (p<0.05) with the NT with the 20 cm pillow(r=0.821).
There were, however, no statistically significant differences in the measured parameters between male and female study participants, with the exception of differences in T1S with the 0 cm pillow(p=0.01) and the NT with the 20 cm pillow(p=0.01).
DISCUSSION
As is already known, optimal sagittal alignment of the spine occurs when all components are in proper balance14). The global balance and regional balance alignment is maintained in each curvature8). If this balance is altered, clinical symptoms related to unbalanced alignment arise.
The T1S and other cervical parameters have been identified as radiographic parameters that are greatly correlated with cervical sagittal balance10). Indeed, the T1 sagittal angle is a measurement that may be very useful in evaluating sagittal balance. In particular, it has great utility where long films cannot be obtained11). Lee et al.12) reported that the TIA and T1S could be used to predict the physiological alignment of the cervical spine on radiographs. Patrick et al.11) demonstrated that patients whose T1S value falls outside the range of 13° to 25° should be sent for full-column radiographs for complete evaluation of their sagittal balance. On the other hand, although patients with a T1S value between 13° and 25° mostly had better sagittal balance than patients with values outside this range, its occurrence does not guarantee normal sagittal balance. Unfortunately, there are no studies to date that have established normative sagittal T1S values. However, in the aforementioned study by Patrick et al.14), their analysis has shown that when the T1S was higher than 25°, all patients had at least 10 cm of positive sagittal imbalance. Their study also showed that patients with a negative sagittal balance had mostly low T1S values, usually below 13° of angulation11). In our study, we found that the T1S value with the 10 cm pillow height was between 13° and 25° for normal sagittal balance. We could advise that the 10 cm pillow height is most suitable for optimal cervical alignment. However, the pillow height of 10 cm is just a numerical value taking into consideration only the cervical parameter and not considering the comfort and satisfaction of patients. Therefore, this value is not an absolute figure.
Although T1S is influenced by aging or posture, it is not a constant parameter. On the other hand, TIA does not change with position or increase of thoracic kyphosis under any condition, similar to the pelvic inlet of the pelvis. The TIA is a constant parameter because, anatomically, the cervical spine is placed on top of the TI, a fixed circular bony structure without range of motion that is composed of the T1 vertebral body, the first ribs on both sides, and the upper part of the sternum17). The sagittal balance of the cervical spine adjusts and can be influenced by the shape and orientation of T1. They concluded that the C2-C7 angle increases with increasing T1S by radiography. Park et al.14) assessed the sagittal parameters of the cervical spine using CT scans in the supine position and concluded that the C2-C7 angle increased as the T1S increased. They also reconfirmed that the TIA can be considered as a fixed reference value14). However, in our study, we measured different TIA values with the 20 cm pillow than other pillow height. Although there are many reasons for this, we thought an error possibly occurred when measuring the angle and the higher pillow height changed the TIA. Additional investigations and considerations of the differences in T1A are necessary.
Loss of cervical lordosis is a complicating factor in the treatment of the cervical spine, and understanding the effects and prognosis of a loss of cervical lordosis is crucial to treatment. However, an embryological basis can be helpful for understanding the pathogenesis of cervical lordosis. In 1977, Bagnall et al.1) demonstrated that cervical lordosis is formed at 9.5 weeks of gestation. In 195 fetuses, they found that at 9.5 weeks, 83% of fetuses have cervical lordosis, 11% have a military configuration, and only 6% of fetuses are in the kyphotic position of the cervical spine1). In other words, by 9.5 weeks 94% of fetuses begin to use their posterior cervical muscles to begin forming the cervical curve. The lordosis begins to form before birth, and once the child begins to lift his/her head, the lordosis becomes clearer. Cervical lordosis has been theorized to exist for biomechanical reasons related to weight distribution, structural support, energy efficiency, and shock absorption. In daily activity, cervical lordosis better distributes forces than a cervical spine which has lost its normal lordosis3). Some studies also reported that an asymptomatic cervical spine did not always show normal lordotic alignment, as kyphotic alignment was revealed in 2% to 35% of individuals81316).
Although the Cobb method works well for the rectangular vertebrae of the thoracic and lumbar spine, it may be less precise for measuring the cervical spine, which has trapezoidal vertebrae13). The Gore method, which uses the posterior vertebral body line as opposed to the superior and inferior end plate lines used by the Cobb method, is considered to be more reproducible when measuring the cervical sagittal alignment15). In the present study, however, we did not use the Gore method, because the Cobb method was more familiar and generally known.
A limitation of the present study is the uneven distribution of data in the cohort. To estimate the result for a normative cohort we included only 16 individuals. Since our cohort might not contain all the representative patterns of sagittal alignment, we analyzed the non-parametric statistical test. An additional study, with a larger number of cases, is still needed to be able to carry out an age, body weight, height, and sex-matched controlled investigation and confirm the result of the current study. In other words, our study is a preliminary study, so further studies with more participants are needed in the future. Nevertheless, the study participants included were healthy, young, and without a history of spinal problems. In addition, our study did not evaluate the comfort, pain relief, and level of satisfaction of each pillow, Therefore, further study is required. An active discussion about the T1S and cervical sagittal alignment is also in progress. Some studies propose an approximate average value for cervical sagittal alignment, but there is no "gold standard" established as yet, and additional investigations of cervical alignment are still necessary.
CONCLUSION
From the data obtained in this study, we recommend that the most suitable pillow height is 10 cm considering the normal cervical lordosis. Additionally, the NT value decreased with increasing pillow height, whereas TIA values tended to remain constant.