 |
 |
- Search
Abstract
We present a rare case of intramuscular schwannoma originating from the dorsal ramus nerve in a 62-year-old woman. The mass grew slowly, with pain developing upon touch five years prior. No neurological deficit was detected. The mass was observed in the erector spinae muscles in magnetic resonance imaging (MRI), and surgical excision was performed. The mass was well encapsulated with clear margin. The lesion appeared to originate from the cranial side. We completely removed the mass including the origin. Histopathology confirmed a schwannoma diagnosis. This is the first report, to our knowledge, of a dorsal ramus-nerve schwannoma within the erector spinae muscles.
Schwannomas are benign tumors that originate from nerve sheaths composed exclusively of Schwann cells8,9,10). A major-nerve, intramuscular schwannoma is an extremely rare condition9). Due to low frequency of this tumor type and lack of specific instrumental signs and symptoms, pre-surgical diagnosis is difficult1). We present a rare case of intramuscular schwannoma originating from the dorsal ramus nerve in a 62-year-old woman.
A 62-year-old woman patient was admitted to the hospital because of a palpable back mass on her left side. The mass was identified eight years prior, and grew slowly, until pain developed upon touch five years prior. No neurological deficit was detected.
The mass was observed in the left erector spinae muscles (in the L2-4 region) by magnetic resonance imaging (MRI). The tumor had an oval shape and an approximate size of 4.5├Ś4├Ś7.5 cm. It was well defined, lobulated, and heterogeneously enhanced. T2- and T1-weighted images showed heterogeneous high signal intensity, and intermediate to low signal intensity, respectively (Fig. 1). The preoperative diagnostic evaluation suggested the growth was metastasis, sarcoma, or a peripheral nerve sheath tumor.
Following preoperative assessment, surgical excision was performed. The mass was well encapsulated, with clear margins in the erector spinae muscles. The lesion was thought to originate on the cranial side, and was completely removed, including the origin. When the mas was cut, the surface of the mass was mottled, whitish pale-yellow, and myxoid with hemorrhagic foci (Fig. 2). Microscopically, the tumor was composed of compact spindle cell regions (Antoni-A), with a nuclear, palisading and whirling cell pattern, and loosely arranged areas of lower cell density (Antoni-B), along with ectatic, irregularly-shaped hyalinized vessels (Fig. 3). Immunohistochemistry revealed diffuse, high S-100 protein expression.
The most common types of benign soft tissue tumor are lipoma and related variants (16%), and other types include fibrous histiocytoma (13%), nodular fasciitis (11%), hemangioma (8%), and schwannoma (5%)5). Approximately 25 and 45% of schwannoma cases occur in the head and neck areas, respectively12). The symptom frequencies reported among patients with benign schwannoma are 5-52% for tenderness, 20% for radicular pain, 60-96% for the Tinel sign, and 7.6-82% for motor weakness6). Intramuscular schwannomas are highly uncommon; however, reports have been documented for such tumors originating from the psoas and coracobrachialis muscles, with palpable masses that presented with either no symptoms or lower extremities numbness, but no characteristic symptomatic features1,2,4,8,9). Schwannomas typically originate from a small nerve branch within the muscle, and symptoms vary depending on the site of origin6,9,13). Because intramuscular schwannomas originate from motor branch nerves, neurological symptoms, including pain, motor weakness, paresthesia, are rare6,9). In our case, there was no radicular pain or motor weak ness; however slight tenderness was reported.
In our patient, intramuscular schwannoma occurred in the erector spinae muscles. The erector spinae muscles are dominated by the lumbar dorsal ramus nerve, which branches to form the spinae nerve. The dorsal ramus nerve runs dorsocaudally in the transverse domain, and generally separates into the medial, intermediate, and lateral branches3).
Schwannomas are typically well encapsulated and solid with membranes composed of a thin fibrous capsule pressing on perineural tissue1,2). However, if a schwannoma is large, it appears heterogeneous in radiological exams, indicating hemorrhage and tissue necrosis1).
In the present study, we observed a typical schwannoma pattern, with a relatively large tumor. However, hemorrhage and tissue necrosis were not observed. Histological results were consistent with previous findings. The histological hallmark of a schwannoma is varying proportions of two distinctive tissues: fascicular type (Antoni-A) and reticular type (Antoni-B)9,11). Antoni-A is highly cellular, with compact, spindle-shaped cells1,7,9,11). Antoni-B is highly vascularized and lacks distinctive structural features9,11). Immunohistochemically, schwannomas typically show diffuse, strongly S-100 protein expression11).
In the present case, we cautiously removed the encapsulated mass and excised the origin, which appeared to be the dorsal ramus nerve. Our tissue biopsy confirmed the presence of a very rare intramuscular benign schwannoma, with typical features.
To our knowledge, this is the first report of a dorsal ramus nerve schwannoma within the erector spinae muscles. When a patient has palpable, deep or intrinsic back muscle tissue mass, a radiological examination, such as a computed tomography (CT) or MRI should be considered. In the CT or MRI, a distinct pattern in the surrounding wall of the mass is suggestive of schwannoma, which we confirmed by needle biopsy. If histological findings suggested the presence of Antoni-A or -B and the S-100 protein is strongly expressed, a diagnosis of dorsal ramus schwannoma should be considered.
References
1. D'Silva KJ, Dwivedi AJ, Barnwell JM. Schwannoma of the psoas major muscle presenting with abdominal and back pain. Dig Dis Sci 2003 48:1619-1621. PMID: 12924657.


2. Hsu YC, Shih YY, Gao HW, Huang GS. Intramuscular schwannoma arising from the psoas muscle presenting with femoral nerve neuropathy. South Med J 2010 103:477-479. PMID: 20375951.


3. Hu ZJ, Fang XQ, Fan SW. Iatrogenic injury to the erector spinae during posterior lumbar spine surgery: underlying anatomical considerations, preventable root causes, and surgical tips and tricks. Eur J Orthop Surg Traumatol 2014 24:127-135. PMID: 23417108.


4. Knight DM, Birch R, Pringle J. Benign solitary schwannomas: a review of 234 cases. J Bone Joint Surg Br 2007 89:382-387. PMID: 17356155.


5. Kransdorf MJ. Benign soft-tissue tumors in a large referral population: distribution of specific diagnoses by age, sex, and location. Am J Roentgenol 1995 164:395-402. PMID: 7839977.

6. Kwon BC, Baek GH, Chung MS, Lee SH, Kim HS, Oh JH. Intramuscular neurilemoma. J Bone Joint Surg Br 2003 85:723-725. PMID: 12892197.


7. Li Q, Gao C, Juzi JT, Hao X. Analysis of 82 cases of retroperitoneal schwannoma. ANZ J Surg 2007 77:237-240. PMID: 17388825.


8. Muramatsu K, Ihara K, Yoshida Y, Taguchi T. Intramuscular schwannoma arising from the psoas major muscle. Clin Neurol Neurosurg 2008 110:532-533. PMID: 18358596.


9. Nishio J, Ueki T, Naito M. Intramuscular schwannoma of the musculocutaneous nerve: An uncommon clinical presentation. Exp Ther Med 2013 6:164-166. PMID: 23935739.



10. Park HS, Bong HJ, Kim JT, Jang KS. Benign Brachial Plexus Nerve Sheath Tumor: Schwannoma. Korean J Spine 2009 6:32-34.
11. Rodriguez FJ, Folpe AL, Giannini C, Perry A. Pathology of peripheral nerve sheath tumors: diagnostic overview and update on selected diagnostic problems. Acta Neuropathol 2012 123:295-319. PMID: 22327363.



12. Sahoo PK, Mandal PK, Ghosh S. Schwannoma of the hard palate. Natl J Maxillofac Surg 2014 5:39-41. PMID: 25298716.



13. Shimose S, Sugita T, Kubo T, Matsuo T, Nobuto H, Tanaka K, et al. Major-nerve schwannomas versus intramuscular schwannomas. Acta Radiol 2007 48:672-677. PMID: 17611877.


Fig.┬Ā1
Magnetic resonance image (MRI) of a mass in the left erector spinae muscle. (A) T1-weighted enhanced axial image showing a 4.5-cm round, bi-lobulated mass, with heterogeneous enhancement. (B) T1-weighted enhanced coronal image showing a 7.5-cm mass.
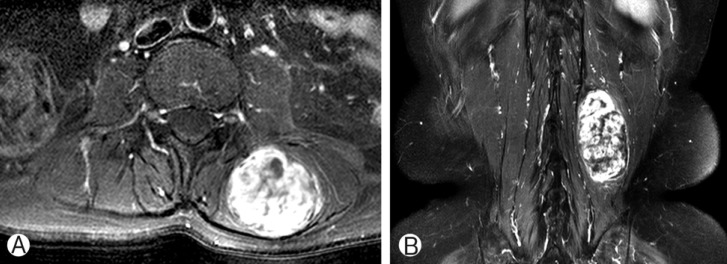
Fig.┬Ā2
Intraoperative and post-excision images of the mass removed from our patient. (A) Encapsulated mass in the muscle layer. (B) The mass is reddish-white, 7.5-cm long, and oval. (C) Cutting the tumor surface reveals solid and myxoid composition with focally-yellowish spots.

Fig.┬Ā3
Microscopy analysis results. (A) Compact Antoni-A with nuclear palisading, and loose, Antoni-B regions with hyalinized thick-walled vessels, creating a biphasic pattern (H&E; 100├Ś magnification). (B) Excised tumor immunohistochemical staining reveals strong cellular S-100 protein expression (image obtained using S-100 protein antibodies; 200├Śmagnification).


- TOOLS
-
METRICS

-
- 5 Crossref
- Scopus
- 8,189 View
- 86 Download
- Related articles in NS
-
Chronic Spinal Epidural Hematoma due to Repeated Epidural Block: A Case Report.2008 March;5(1)
Intramedullary Mature Teratoma of the Spinal Cord - A Case Report -2007 December;4(4)
Vertebral Pheochromocytoma of the Cervical Spine - A Case Report -2006 December;3(4)
Purely Intramedullary Meningioma of the Thoracic Cord - Cases Report -2006 March;3(1)
Dual Myxopapillary Ependymoma of the Cauda Equina - Case Report -2006 March;3(1)
-
Journal Impact Factor 3.2

























