Complications of Anterior Cervical Fusion using a Low-dose Recombinant Human Bone Morphogenetic Protein-2
Article information
Abstract
Objective
There are several reports, which documented a high incidence of complications following the use of recombinant human bone morphogenetic protein-2 (rhBMP-2) in anterior cervical fusions (ACFs). The objective of this study is to share our experience with low-dose rhBMP-2 in anterior cervical spine.
Methods
We performed a retrospective analysis of 197 patients who underwent anterior cervical fusion (ACF) with the use of recombinant human bone morphogenetic protein-2 (rhBMP-2) during 2007-2012. A low-dose rhBMP-2 (0.7mg/level) sponge was placed exclusively within the cage. In 102 patients demineralized bone matrix (DBM) was filled around the BMP sponge. Incidence and severity of dysphagia was determined by 5 points SWAL-QOL scale.
Results
Two patients had prolonged hospitalization due to BMP unrelated causes. Following the discharge, 13.2%(n=26) patients developed dysphagia and 8.6%(n=17) patients complained of neck swelling. More than half of the patients (52.9%, n=9) with neck swelling also had associated dysphagia; however, only 2 of these patients necessitated readmission. Both of these patients responded well to the intravenous dexamethasone. The use of DBM did not affect the incidence and severity of complications (p>0.05). Clinico-radiological evidence of fusion was not observed in 2 patients.
Conclusion
A low-dose rhBMP-2 in ACFs is not without risk. However, the incidence and severity of complications seem to be lower with low-dose BMP placed exclusively inside the cage. Packing DBM putty around the BMP sponge does not affect the safety profile of rhBMP-2 in ACFs.
INTRODUCTION
Anterior cervical fusion (ACF) is a commonly performed surgical procedure to treat degenerative disorders of the cervical spine9). Although the use of tricortical iliac crest bone graft in ACFs is associated with the excellent outcomes, the risk of donor site related complications have always incited the spine surgeon to use various contemporary graft substitutes. In 1965, Urist14) discovered a subset of protein extract, which had a significant potential of inducing new bone formation even at the non-osseous tissues. The proteins were termed bone morphogenetic proteins (BMPs). Recombinant human bone morphogenetic protein-2 (rhBMP-2) is a member of this family, which has gained a widespread popularity for its application in spinal fusions. Although, their role in lumbar fusions is well established, the safety profile of rhBMP-2 in ACFs is yet to be defined101113).
Baskin et al.1) were the first authors who conducted a prospective randomized controlled trial and reported that the use rhBMP-2 in ACFs is a safe and effective technique. Conversely several other authors reported a high incidence of neck swelling and dysphagia associated with the use of rhBMP-2 warranting either prolonged stay in the hospital or readmissions of the patients6101115). Despite the high fusions rates, some authors have even abandoned the use of rhBMP-2 for ACFs due to its cost, side effects and availability of safer alternatives15). On the basis of results of earlier trials, Food and Drug Administration (FDA) issued a warning in 2008 against the use of rhBMP-2 in ACFs until the sufficient evidence is available about its safety.
Shields et al.10) reported a high rate of complications and attributed it to the use of greater amount of BMP dose (2.1 mg/level) placed both inside and outside the cage. Further emphasis on the influence of the dose and delivery method of rhBMP-2 in ACFs was given by Dickerman et al.4) and in their letter they proposed that the containment of low dose (1.05 mg) rhBMP-2 within the cage and placing demineralized bone matrix (DBM) putty surrounding the INFUSE ensures a controlled delivery of rhBMP-2 in the vicinity of desired fusion site, which therefore is associated with excellent fusion rates with no adverse effects related to rhBMP-2. The purpose of our study is to share our clinical experience with low-dose of rhBMP-2 in ACF. We also aim to elucidate the impact of dose and delivery techniques of rhBMP-2 on the safety profile of its use in ACFs based on our clinical experience and review of the literature.
MATERIALS AND METHODS
We performed a retrospective analysis of 197 patients who underwent ACF with the use of rhBMP-2 during 2007-2012. ACFs included mainly anterior cervical discectomy and fusion (ACDF, n=191), although few patients underwent anterior cervical corpectomy and fusion (ACCF, n=4). The remaining 2 patients underwent both ACDF and ACCF performed at different levels. All the surgeries were performed by the senior author. Institutional review board approval was taken to conduct this study. There were 80 males (40.6%) and 117 (59.4%) females included in our study. Surgeries were performed for herniated disc prolapsed in 91 patients, for spondylosis with or without instability in 104, and for pseudoarthrosis in 2 patients (revision ACF was performed in both these patients). Most common presenting symptom was neck pain (n=175), followed by arm pain (n=163), sensory deficit (n=102) and motor weakness (n=87). Other conditions affecting the outcome were evaluated. History of cigarette smoking was present in 53 patients (26.9%) and diabetes mellitus in 21 (10.65%). Thirty nine patients had a history of previous neck surgery, most of which had undergone discectomy or nerve decompression by foraminotomy (n=37) and 2 patients had anterior fusions performed at different levels.
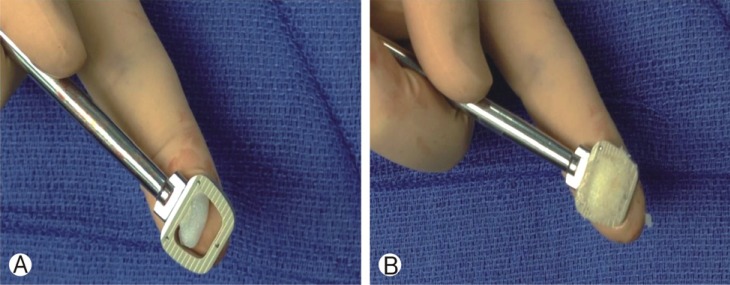
1. Implants and BMP
In the majority of cases (n=191) polyetheretherketone (PEEK) cages were used as a spacer device and the construct was supplemented with anterior cervical plate. In 6 patients, PEEK prevail (Medtronics Sofamor Danek) device was used, which has inbuilt slots for self drilling screws. Cages were filled with INFUSE bone graft substitute, which has 2 components: a reconstituted solution containing recombinant human bone morphogenetic protein-2 (rhBMP-2) and an absorbable collagen sponge (ACS). 1.4mL of rhBMP-2 containing 2.1mg was soaked with ACS measuring 5.08×2.54×0.5 cm. We placed only 1/3 of sponge within the cage (measuring 1.7×2.54×0.5 cm), which would deliver 0.7mg of rhBMP-2 per level considering a homogenous distribution of this protein within the sponge (Fig. 1A). No additional ACS was filled around the cage. In a large number of the patients (n=102), we also used demineralized bone matrix (DBM), which was placed from the top and the bottom over the centrally located INFUSE within the PEEK cage (Fig. 1B).
2. Surgical technique
Unless contraindicated, intravenous dexamethasone (8mg) was administered at the start of the procedure in all cases. Surgery was performed with the standard anterior approach. After achieving the decompression, interbody spaces were prepared for cage placement, which were filled with INFUSE substitute in a proportion already discussed. Anterior plate fixation was supplemented in all patients except in those in which Prevail PEEK device was used (n=6). In the patients with major anatomical deformities, a corpectomy was performed. A larger cage was impacted between the adjacent vertebral endplates following corpectomy. The amount of INFUSE was the same even if a larger spacer was placed after ACCF. Wound irrigation was avoided after the placement of cage. Closure was performed in layers without placing any drain. Unless it was contraindicated, all patients were given methylprednisolone orally (4mg) in taper doses during the first week of postoperative period.
3. Post-operative evaluation and dysphagia calculation
Plain x-ray of the cervical spine was taken within few hours of surgery to document the appropriate placement of hardware. During hospitalization, any events such as dysphagia, neck hematoma, incisional swelling, and vocal cord palsy were recorded. The majority of the patients were discharged within 24 hours of surgery and the patients hospitalized beyond 48 hours were considered to have a prolonged stay. After discharge, the patients were evaluated at 2 weeks, 6 weeks, 3 months, 6 months, 12 months and 24 months after surgery. Clinical and radiological assessments were carried out during each post-operative visit. Fusion was assessed with flexion/extension radiographs at 3 and 6 months postoperatively.
Incidence and severity of dysphagia was retrospectively determined by the 5 point SWAL-QOL scale7). Score 1 indicates the patient almost always had difficulty; score 2 indicates the patient often had difficulty; score 3 indicates the patient sometimes had difficulty; score 4 indicates the patient hardly had any difficulty; score 5 indicates the patient never had difficulty. For the statistical analysis, patients with dysphagia were grouped into minimal (score 3-5) and substantial (score 1-2) dysphagia.
4. Statistical analysis
All statistical analyses were performed using the SPSS software, version 21.0 (IBM Corp., Armonk, NY). The data was analyzed for descriptive and inferential statistics. Descriptive statistics were conducted for frequencies, percentages and proportions. The comparison of incidence and severity of complications between DBM and non-DBM was performed by using Fisher's exact test.
RESULTS
A total of 197 patients with the mean age of 51.3 years and male to female ratio of 1.01 were included in the study. The mean duration of follow-up was 27.5 months (range 9-43 months). The majority of patients underwent single level ACFs (n=110, 55.8%), while 2, 3, 4 levels ACFs were performed in 72 (n=36.5%), 13 (6.6%), 2 (1%) patients respectively.
Hospital stay for the majority of patients was uneventful except in 2 patients who had prolonged hospitalization. An 83 year old patient, who underwent 2 levels ACDF, developed severe postoperative dysphagia on 2nd day of surgery. The clinico-radiological assessment did not reveal any neck swelling or hematoma, but the patient failed swallow tests. The patient was inserted a percutaneous endoscopic gastrostomy (PEG) tube until he started tolerating oral feeds over the next few weeks. The other patient was a 70 year old male with an existing pulmonary dysfunction, who underwent 3 levels ACDF, developed acute respiratory failure on the day of surgery. The patient was reintubated; however, no hematoma or fluid collection in the neck was detected.
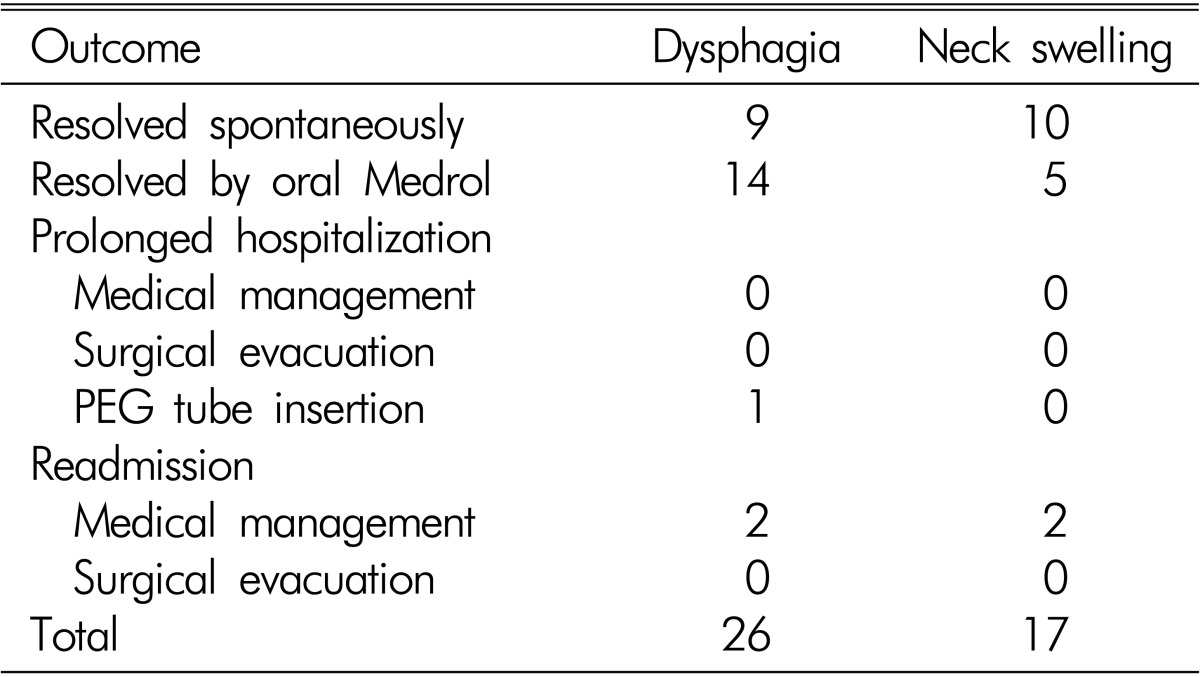
A total of 26 (13.2%) patients complained of dysphagia and the mean duration of onset was 9.2 (range 2-21) days. Of these patients, 15 patients had minimal discomfort (score 3-5) and the remaining 11 patients complained of a substantial degree of discomfort (score 1-2). Seventeen patients (8.6%) reported neck swelling following ACFs. Neck swelling occurred on average postoperative day 5.4 (range 2-12 days). In 9 (34.6%) patients with dysphagia, there was also an associated visible neck swelling. On the other hand, more than half (n=9, 52.9%) of the patients with neck swelling had associated dysphagia. In a large number of the patients these adverse events resolved spontaneously (Table 1). However, several other patients were given oral methylprednisolone as an outpatient; only few required either prolonged hospitalization or readmissions. As already discussed, one patient with severe dysphagia who was found to have swallowing dysfunctions received a PEG tube and therefore, had an extended hospital stay. Two patients with neck swelling were readmitted for the management of associated dysphagia and respiratory difficulty (Fig. 2). Resolution of the symptoms could be achieved in both patients by administering intravenous dexamethasone, and the patients were also given oral methylprednisolone for 5 days following discharge. None of the patients necessitated surgical management for the aforementioned complications. In 102 patients DBM was placed around the INFUSE sponge. Overall the incidence of dysphagia, substantial dysphagia and neck swelling was lower in the patients who were inserted DBM putty around INFUSE. On the contrary, the rate of spontaneous resolution was more in the non-DBM group; although, none of these observations reached statistically significance (Table 2). There was no difference in the incidence of prolonged hospitalization and readmissions in two groups.

Gadolinium-enhanced cervical computerized tomography of a 57-year old male patient at 7th postoperative day following a 3-level ACDF. A large hematoma is visible in the prevertebral space, causing compression and displacement of the trachea and esophagus anteriorly. The patient responded well to intravenous steroids administered over 48 hours of admission.
Apart from the aforementioned events, we also observed other complications in this cohort. Four patients (2%) developed vocal cord palsies, which were transient and subsided over the period of few weeks in all of these patients. Pseudoarthrosis was seen in 2 patients. In the first patient, who was 50 year female with a 3 level ACDF, the fusion did not occur in the lower most vertebral segment. Patient deferred to any further intervention for the persistent symptoms arising from the involved segment. The second patient was a 66 year female, who underwent a single ACDF for the traumatic subluxation of C5/6 region. This patient underwent posterior fusion and stabilization due the radiological presentation of implant loosening and impending loss of fusion at 1 month. One patient developed postoperative deltoid weakness, which subsided spontaneously over the next few months.
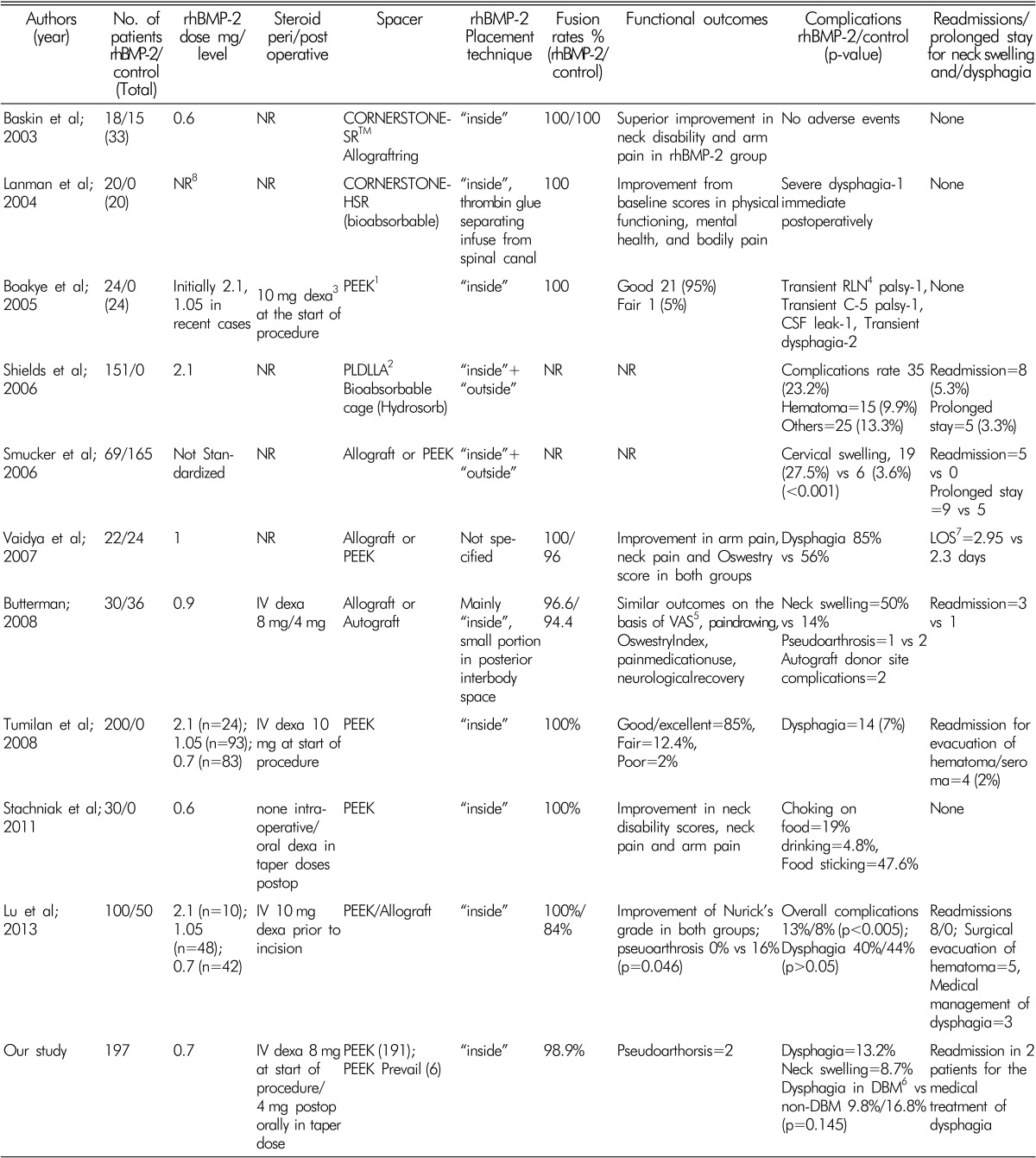
DISCUSSION
The reports of high incidence of complication following its use in ACFs invoked the debate on the safety profile of rhBMP-2 in these procedures. One of such reports was from Schilds et al.10), who documented a significant rate of complications resulting after the use of a high dose rhBMP-2 in ACFs. Interestingly, the incidence of the adverse events in the literature ranges from none to very high rates of complications (Table 3)123561011121315). Lower incidence of the complications in some of the studies has been correlated with the lower dose of rhBMP-2 and methods of delivery241013).
Boakye et al.2) produced the first report of rh-BMP-2 filled in a PEEK spacer, which is what we use at our institution. The authors studied 24 patients that underwent ACDFs with PEEK implants and rh-BMP-2. Two patients were found to have transient dysphagia. Three patients were found to have heterotopic bone formation, while the authors were using half of the amount of a small INFUSE kit (2.1mg rhBMP-2/level). Subsequently, the authors decided to use one-fourth of the sponge (1.05mg rhBMP-2/level) and found no heterotopic bone formation. The results of BMP in ACFs were convincing until Schilds et al.10) presented their study, which documented alarmingly high incidence of complications. However, one glaring difference was the amount of rh-BMP-2 used per level (2.1mg). They also suspected that higher amount of INFUSE used in vertebrectomies led to a greater risk of the adverse events (7.9% vs 38.8% hematoma). The impact of BMP dose was also evident from the study by Tumialan et al.13), who were initially using 2.1mg/level. The authors noticed excess interbody bone formation in the first 24 patients and subsequently reduced the dose to 1.05mg of rh-BMP-2 per level in the next 93 patients. The authors went on to reduce the dose even more (0.7 mg/level) as more studies supported using a smaller dose.
Recent attention has also been directed to the methods of delivery. While reviewing their results, Schilds et al.10) pointed out that the placement of BMP sponge outside the cage could be related to the high incidence of complication in their series. Some surgeons have also used thrombin glue to control the diffusion of BMP into the surrounding tissues5). The influence of delivery techniques gained more ground when Dickermann et al.4) shared their experience with using DBM around BMP sponge to minimize its leakage. The authors reported excellent results with no adverse effects of using rhBMP-2 in ACFs.
In the present study, we used a low-dose rhBMP-2 (0.7mg/level) and placed it exclusively inside the cage. In approximately half of the patient, we also used DBM around the BMP sponge. The incidence of dysphagia and neck swelling in our series was 13.2% and 8.6% respectively. Only 2 patients necessitated readmission and both of them responded well to the intravenous dexamethasone. Surgical evacuation was not required in any of the patients. The incidence and severity of complications were lower in the patients, in whom DBM was used, though these observations were not statistically significant. Interestingly, in a large number of the patients, the aforementioned symptoms resolved spontaneously.
A careful evaluation of previous studies also gives a clue to the effect of dose and delivery methods on the safety profile of rhBMP-2 in ACFs (Table 3). As already discussed, higher dose and placing BMP sponge outside the cage were probably responsible for the greater incidence of adverse events in the case series presented by Schilds et al.10). Apparently, Buttermann3) used a smaller dose of BMP as compared to Boakye et al.2) (0.9 vs 1.05mg); however, the incidence of complications was lower in the later study. Placement of INFUSE both within and outside the cage may be a possible explanation for higher incidence of adverse events observed by Buttermann. Usage of rhBMP-2 in ACFs has been described as a safe technique by several authors11213). It is also evident from the review of these studies that the authors either used low-dose BMP or placed it exclusively inside the cage or both (Table 3). On the basis of our findings, it appears that low dose BMP placed only inside the cage has a lower complication rate than previously reported higher doses (Table 3). Unlike higher readmission and reexploration rate in these reports, we had only 2 readmissions with BMP related complication and none of them required any surgical intervention. However, the risk of complications associated with the use of low-dose BMP seems to be greater than risk without its use. In a recent report from our institution, we documented relatively a lower risk of morbidity in a large group of patients who underwent ACDF without BMP (overall 8.4%, dysphagia 3.3%, neck hematoma 0.1%, and recurrent laryngeal nerve palsy 0.1%)8).
There are other factors, which may also influence the risk of complications in ACFs using BMP. Tumilian et al.13) stated that irrigation should be avoided after the placement of BMP to minimize any displacement of the protein into surrounding structures that can lead to inflammatory reactions in the adjacent tissues or cause heterotopic bone formation. This is something that is practiced at our institution as well. Perioperative steroid administration is also found to reduce the complaints of dysphagia and neck swelling3). Unless contraindicated, we also gave steroid in all patients and as discussed earlier. This may be responsible for spontaneous resolution of the symptoms in some patients. The authors in the past used several different designs of cages. The impact of type of spacer on the safety profile of BMP in ACFs is unknown.
Evaluation of outcomes in a retrospective manner is a major limitation of our study. The amount of rhBMP-2 in INFUSE sponge cannot be accurately measured and it is also difficult to determine that how precisely 1/3rd portion was separated from the remaining sponge. The impact of selection bias related to the surgeon's choice of using DBM in approximately half of the cases also cannot be denied. We also believe that the cost-effectiveness of rhBMP-2 and DBM should also be evaluated, which is another limitation of the present study.
CONCLUSION
The use of low-dose rhBMP-2 in anterior cervical fusion is not without risk. However, in comparison to previous reports with high dose BMP placed both inside and outside the cage, a low-dose of BMP placed exclusively within the spacer is associated with lower incidence and severity of complications. Placing DBM putty around the BMP sponge does not seem to affect the safety profile of BMP in ACFs.