|
 |
- Search
Abstract
Objective
This study was conducted to compare radiologic changes and clinical outcomes in adjacent level of percutaneous pedicle screws with those of conventional (open) pedicle screws.
Methods
From January 2007 to December 2009, 51 patients underwent L3-5 decompression and spinal fusion. Percutaneous pedicle screws were used in 22 patients, and open pedicle screws were used in the remaining patients. For estimation of instability, we performed measurements of change in the lordotic and adjacent segment angles. A retrospective evaluation of the patients' data and several assessment scales was conducted for determination of clinical outcomes.
Results
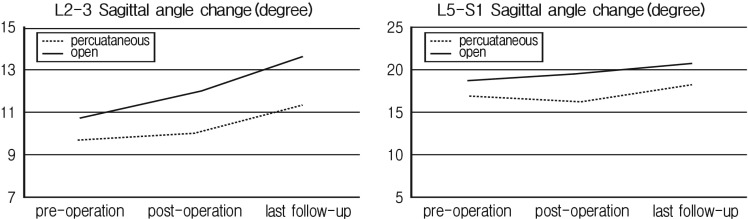
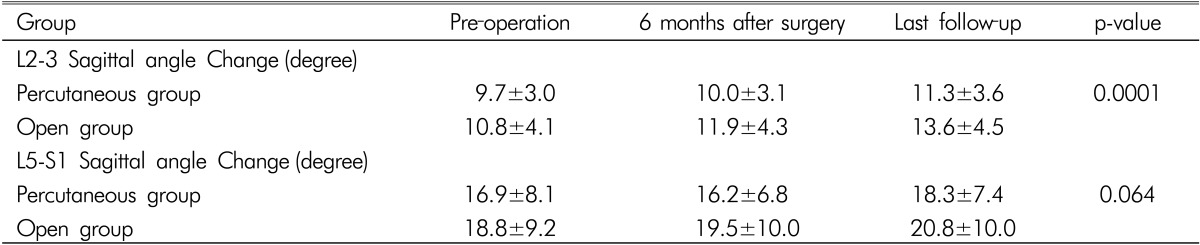
The radiological examinations revealed no significant differences, except the L2-3 sagittal angle change. The upper adjacent level angle change in the open group was larger than that in the percutaneous group. In the percutaneous group, the sagittal angle changed from 9.7±3.0° to 11.25±3.6° during the follow-up periods, and in the open group, the sagittal angle changed from 10.8±4.1° to 13.6±4.5°. Radiological instability was observed in 5 patients (17%) in the open group and in 2 patients (9%) in the percutaneous group. Both groups showed similar clinical outcomes.
To achieve spinal stability, posterior pedicle screw fixation is widely used as an effective treatment for degenerative diseases of the lumbar spine7,16,22). However, conventional (open) posterior pedicle screw fixation requires extensive dissection and excessive traction on muscle, causing weakening of the supporting structures of the spine11,18,26,27,29,30). It is associated with high medical expense and blood loss, and, most importantly, with degeneration of adjacent spines11,18,21,26,27,29,30).
In consideration of these problems, posterior spinal fusion using percutaneous pedicle screws has been presented as a technique for minimally invasive spine surgery20). A large number of studies have reported on effective treatment using percutaneous pedicle screws, resulting in decreased medical expense and blood loss, as well as protection of the supporting structures of the spine8,12,16,18,19,21,23,24,28).
This study provides a comparative analysis of degeneration in adjacent spinal levels and patient's clinical outcomes between conventional and percutaneous pedicle screws in the treatment of degenerative disease at the L3 to L5 level.
We conducted a retrospective examination of the radiographic images and medical records from patients with degenerative lumbar disease at L3-5, who were treated with posterolateral spinal fusion, or bilateral interbody fusion at our institution from January 2007 to December 2009. We compared and evaluated patients with spondylolisthesis, spinal stenosis, or spinal instability with neurologic sysmptoms or without improvement of pain by conservative treatment, and who had undergone conventional (open) or percutaneous pedicle screw fixation. We excluded patients whose surgery was performed for other indications, such as fracture or infection and severe spondylolisthesis Grade III or over, severe osteoporosis, or degenerative scoliosis because of the difficulty in com- paring these cases. In all the patients, time spent in surgery, mean blood loss, postoperative complications, and re-operation were evaluated with regard to whether preoperative simple radiography, computerized tomography and magnetic resonance imaging, and radiological tests were performed, which was confirmed by radiographic changes. We assessed plain radiographs (anterior-posterior, lateral, and flexion-extension lumbar views) preoperatively, 6 months, and at the final follow-up examination. The outcomes and patient satisfaction were assessed as of the last follow-up examination.
Under general anesthesia, partial laminectomy and foraminotomy for decompression were performed on all the patients, depending on the degree of stenosis. After opening midline minimally, using mixed autograft and allograft bones, the patients underwent bilateral or unilateral L3-4 and L4-5 interbody fusion with open or percutaneous pedicle screw fixation.
For the analysis of the postoperative results, we compared blood loss during the operation, subsequent blood transfusion, and operation time in each group. In addition, we retrospectively reviewed postoperative complications, such as postoperative infection, that occurred during the follow-up period, and whether or not re-operation was necessitated.
The Brantigan and Steffee classification was used for estimation of the postoperative fusion state5). We defined bone fusion Brantigan-Steffee classification grade 4 or 5 in the final radiological follow-up image.
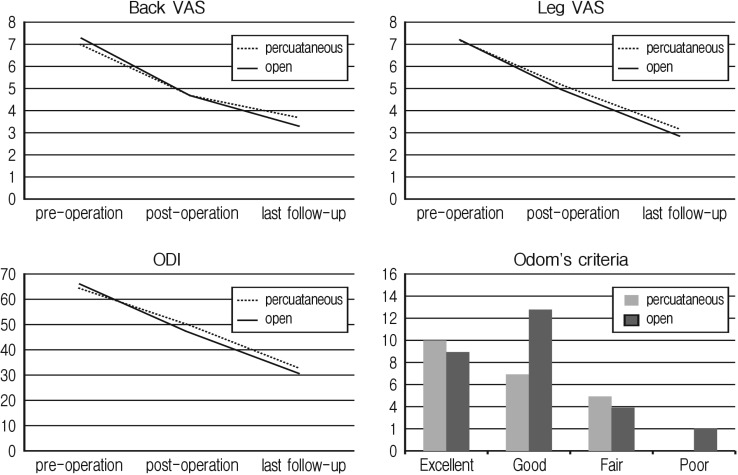
Odom's criteria, the visual analogue scale, and the Oswestry disability index (ODI) were used in analysis of postoperative patient satisfaction and degree of functional recovery. The visual analogue scale measures back and leg pain, and the ODI was used to assess 10 aspects of daily activity as they related to pain, except for sexual activity. All the clinical outcome scales were measured at preoperatively, postoperatively, and at the time of the last follow-up examination.
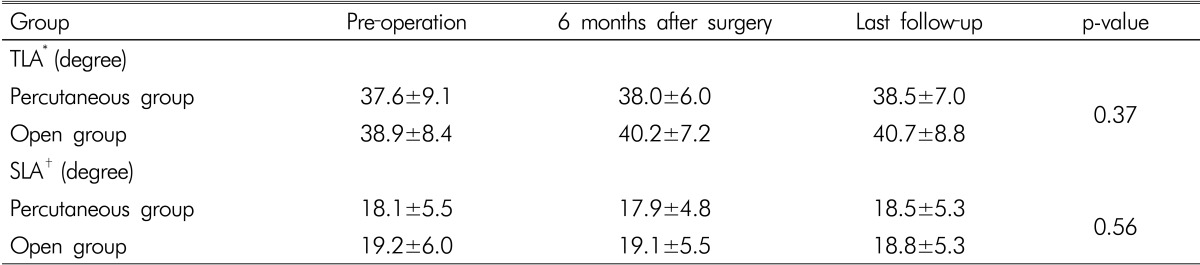
The total lordotic and segmental lordotic angles of the L3-5 lumbar fixation site were measured in a simple lateral view to estimate the stability of the spinal segment after posterior lumbar fusion. Cobbs method was used for estimation of the total lordotic angle; the angle formed by parallel lines on the tops of the L1 and S1 vertebrae2). The segmental lordotic angle was estimated by the angle formed by parallel lines on the top of the L3 vertebra and the bottom of the L5 vertebra2). The lordotic angles were measured using simple lateral view taken before surgery, 6 months after the operation, and at the last follow-up examination.
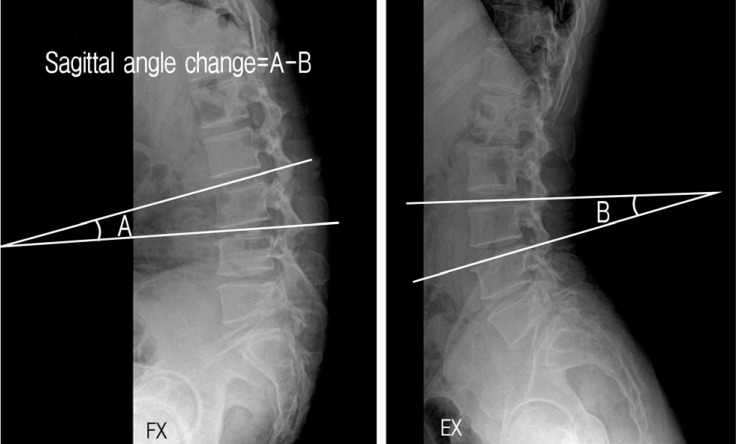
To determine instability of the adjacent segments after fixation, the segmental angle changes of L2-3 and L5-S1 were measured using simple lateral and flexion-extension views (Fig. 1). In the flexion-extension view, the angle made by parallel lines on the bottom of the upper lumbar body next to the fixed spine and the top of the lower lumbar body were measured and changes in the angle were extracted from the angle of flexion and extension31). Changes in the segmental angle exceeding 15° at L2-3 and 25° at L5-S1 are defined as potential instability31). Also, lordotic angle and adjacent instability measured preoperatively, 6 months after the operation, and during the last follow-up period were noted.
The data were processed using the SPSS version 19; X2-test, independent samples T-test, and repeated measures ANOVA at a significance level of 5% were performed for verification. First, X2-test was performed to estimate whether there was a differences with regard to the need for blood transfusion between the patients who underwent traditional screw fixation and those who underwent percutaneous screw fixation. Second, a parametric T-test was conducted for comparison of intraoperative bleeding, operative time, hospital stay, and degree of bone fusion between the groups. Finally repeated measures and the visual analogue scale, ODI, total lordotic angle, segmental lordotic angle, and change in segmental angle were used for evaluation of spinal instability in the patients in each group and were compared using repeated measures ANOVA.
From January 2007 to December 2009, at Gachon Gil Medical Hospital, 51 patients underwent posterior lumbar fusion, of whom 29 underwent conventional open posterior spinal fusion with pedicle screw fixation and 22 underwent percutaneous pedicle screw fixation. Seventeen patients were male. The mean age of the female patients was 34 to 57 years (range, 29-82 years). The mean follow-up period was 35.6 months for the open screw group and 30.28 months for the percutaneous screw group. Twenty-five patients were found with spinal stenosis, 15 with spondylolisthesis, and the others with spinal instability.
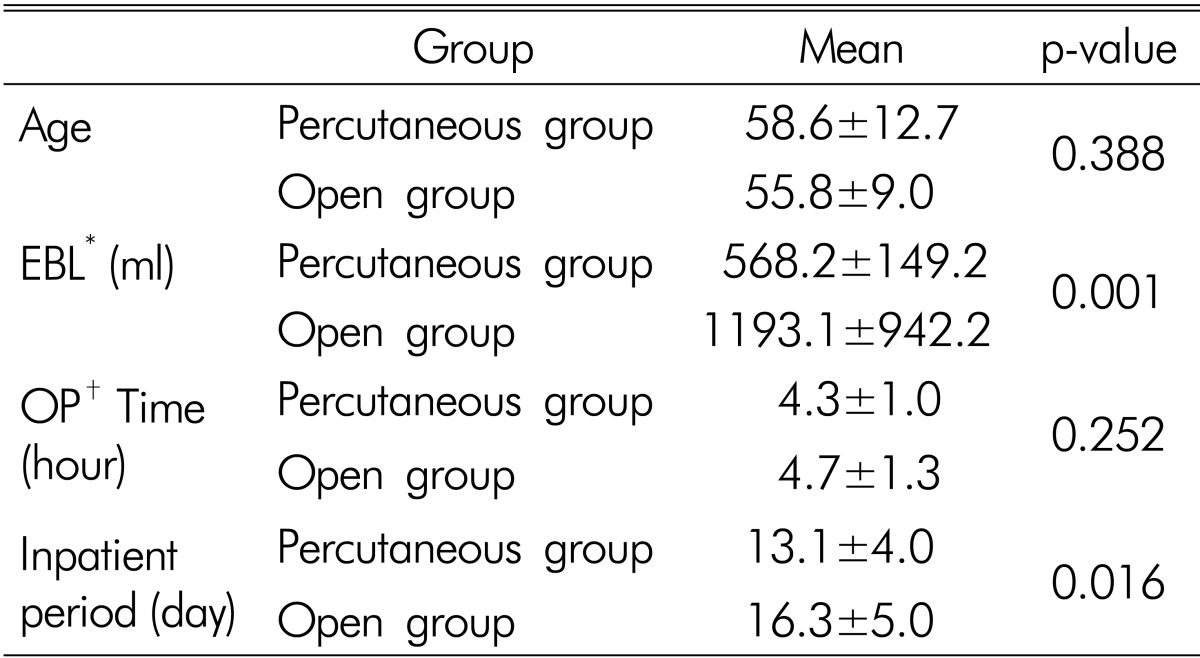
The patients in the percutaneous pedicle screw fixation group had significantly shorter in-hospital stay (13.8 days), than the patients in the open pedicle screw fixation group (16.3 days.) (Table 1).
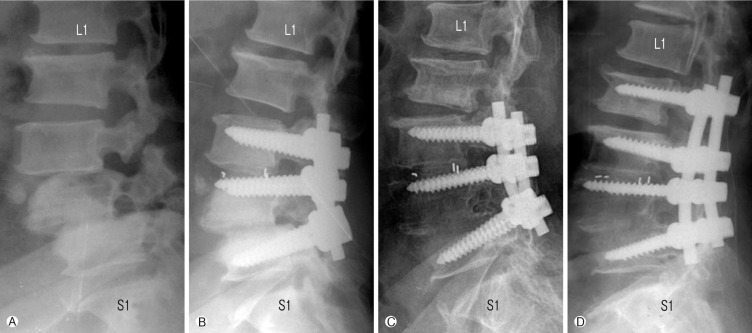
The operative time was approximately 4.5 hours for each patient, and no significant difference was observed between the patients; however-, the mean blood loss in the open pedicle screw fixation group (1193.1mL) was higher than that in the percutaneous pedicle screw fixation group (568.2mL) (Table 1). No serious postoperative complications, such as motor weakness, were observed; however, 2 patients who underwent open pedicle screw fixation and 1patient who underwent percutaneous pedicle screw fixation developed superficial wound infections after the surgery. All the patients recovered without sequelae after treatment with antibiotics. One patient in the open pedicle screw fixation group, who had severe back pain with segmental instability in the L2-L3 segment, required re-operation involving posterior lumbar fusion of L2-L3 (Fig. 2). In addition, the postoperative results for each group showed no statistically significant differences (Table 1). The Brantigan and Steffee classification was used for determination of fusion after the surgery. According to the classification, grade 4 or 5 can be regarded as a good bone fusion state; 20 (90.9%) of 22 patients in the open pedicle screw group and 28 (96.6%) of the 29 patients in the percutaneous pedicle screw group were classified as grade 4 or 5. No statistically significant differences were observed between the 2 groups.
After the surgery, patient satisfaction was measured according to 3 scales (the visual analogue scale, ODI, and Odom's criteria). The results for each scale are as follows. The visual analogue scale (VAS) scores for back pain (back VAS) and radiating pain (leg VAS) showed a consistent decrease after the operation to the last follow-up period (Fig. 3). The back VAS score decreased from 7.0 to 3.7 in the percutaneous screw group and from 7.2 to 3.3 in the open screw group. The leg VAS score decreased from 7.2 to 3.2 in the percutaneous screw group and from 7.2 to 2.9 in the open screw group. The changes in the postoperative VAS scores were similar in each patient group, with no statistically significant differences between the 2 groups. The ODI also, showed a gradual decrease in both groups after the surgery (Fig. 3). The ODI decreased from 64.5 to 32.5 in the percutaneous screw group and from 66.3 to 30.8 in the open screw group. According to Odom's criteria, 19 persons had excellent grades, 20 persons had good grades, and 9 persons had poor grades (Fig. 3). No statistically significant differences were observed between the 2 groups.
The total lordotic angle change showed a slight increase during the follow-up period in the open pedicle screw group. In the percutaneous pedicle screw group, the total lordotic angle showed a slight decrease. However, this difference was not statistically significant (Table 2).
As shown in the graph, the segmental lordotic angle change in the patients who underwent posterior open pedicle screw fusion, showed a decrease during the last follow-up period. In the percutaneous pedicle screw group, the graph shows changes in the segmental lordotic angle, making a V-shape. These changes with time are insignificant. Likewise, no statistically significant difference was observed between the 2 groups (Table 2).
For evaluation of spinal instability, the flexion-extension sagittal angle change in the adjacent segments (L2-L3, L5-S1) was measured until the last follow-up period. With the passage of time, the patients in the open pedicle screw group and percutaneous pedicle screw group showed an increased angle change in L2-L3 (Fig. 4). The angle change over time (the slope of the graph) in the open pedicle screw group was much greater than that in the percutaneous pedicle screw group (Table 3). On the other hand, angle change was observed at the lower adjacent level (L5-S1), but showed a similar increase with time as the angle change in L2-L3, with no statistically significant differences between the 2 groups (Table 3). Six patients showed instability at L2-L3, including 5 of 7 in the open pedicle screw group. One patient in each group showed instability at L5-S1.
Use of percutaneous pedicle screw fixation, a minimally invasive operative technique, can result in decreased injury to paraspinal structures and facet joints. Its advantages include reduced intraoperative bleeding and postoperative back pain, compared with open pedicle screw fixation. The pedicle screw was first introduced in 1959, by Boucher3). Several years later, Roy-Camille etale23) established a constituency of pedicle screw fixation by creation of the dorsal construct composed of screw and rod. Since that time, pedicle screw fixation has been widely used in the treatment of many degenerative spinal diseases. Because of the need to secure an entry point and cortical bone, conventional pedicle screw fixation requires extensive dissection, causing injury to the supporting structures of the spine. It has been associated with increased medical expense, increased amounts of blood transfusion and higher rates of postoperative infection11,18,21,26,27,29,30).
Several studies have reported that pedicle screw fixation, which minimizes injury to supporting structures of the spine, could alleviate some of these problems and reduce pain caused by damage to facet joints and atrophy of paraspinal muscles6,8,12,17,21,24,28).
In this study, we compared patients who underwent open pedicle screw fixation and those who underwent percutaneous pedicle screw fixation with regard to duration of operation, postoperative complications, in-hospital stays, blood loss, and amount of blood transfusion. Each factor showed a slight difference; in particular, blood loss and amount of blood transfusion were significantly greater in the open pedicle screw group than in the percutaneous pedicle screw group. The in hospital stay was also longer in the open pedicle screw group. These results, which are identical to those of previous studies, show statistical significance and demonstrate the advantage of percutaneous pedicle screw fixation. We speculate that although the patients in the percutaneous pedicle screw group had a midline incision for interbody fusion, less muscle dissection and less violation of the facets joint made for the decrease in blood loss. In a previous study involving 1 level spinal fusion, we reported that no difference was observed between open and percutaneous pedicle screws with regard to the above-mentioned factors15). Judging from the 2 studies reported by our group, we suppose that, in a multi-level spinal pedicle screw fixation, the advantage of the pedicle screw is more emphasized.
The clinical outcomes were good in both groups and the VAS scores and ODIs revealed a decrease with time. No difference was observed between the 2 groups. As reported in previous studies7,21,32), this result demonstrates that the percutaneous pedicle screw can also be effective in the treatment of degenerative spinal diseases.
The angle change in the adjacent segment fixed by the pedicle screw showed an increase over the course of time, particularly in L2-L3; some patients presented with spinal instability. Although the angle change increased in L5-S1, no statistically significant difference was observed between the 2 groups. This result demonstrated that adjacent segment syndrome occurred more frequently in the upper segment of the screw-fixed spine1,14,22). In addition, this result was clearly observed in the open pedicle screw group. Open pedicle screws showed a greater association with injury to the facet joint of the upper body, compared with percutaneous pedicle screws. In consideration of these results, we hypothesized that patients who undergo open pedicle screw fixation are more likely to contract adjacent segment disease than patients who undergo percutaneous pedicle screw fixation. In fact, 1 patient in the open pedicle screw group in our study underwent re-operation for treatment of adjacent segment disease in L2-L3. On the other hand, use of percutaneous pedicle screws can result in preservation of facet joints of the upper body and minimize injury to paraspinal supporting structures6,10). On the basis of these facts and the results of our study, our hypothesis that development of adjacent segment disease occurs more often in patients who undergo open pedicle screw fixation than in patients who undergo percutaneous pedicle screw fixation was confirmed.
Of course, percutaneous pedicle screws have disadvantages. The accuracy of percutaneous pedicle screws is stills controversial issue13). Open pedicle screws make it easier to achieve the natural lordotic curve of the lumbar spine, than percutaneous pedicle screws2). Thus, the success rates of bone fusion tend to be higher with open pedicle screws. However, because of the 2 level fusion and small study' group, in our study the bone fusion rates show no statistically significant difference between the 2 groups.
Our study has several limitations. Because the study is a retrospective one, all the data were obtained from medical charts and radiological studies from the past. Therefore, we were not able to control all the variables, which may have influenced the results of the study. Moreover, the study did not include a large number of patients for comparison. However, the patients in the 2 groups were statistically similar in age, follow-up period, and diagnosis. We were, then, able to perform identical operative methods and radiological studies, during the same period. Therefore, the results of this study are considered to have significant value.
It is of fore most importance to note that this study is preliminary. To identify adjacent segment disease, clinical symptoms caused by degeneration of adjacent segments should be observed over a long-term period9,19). The identification of relationships between degeneration of adjacent levels of the spine and clinical symptoms with long-term follow-up is needed. Moreover, we need to assess another radiological change such as spondylolisthesis. To validate our results, larger-scale prospective study will be needed.
Our retrospective study was conducted to investigate and analyze the clinical outcome and postoperative radiological change in patients who underwent posterior L3-L4-L5 fusion using percutaneous and open pedicle screws. We found that the use of percutaneous pedicle screws may be more effective in preventing adjacent segment syndrome than the use of open pedicle screws. In addition, as we perform longer levels of spinal fusion, the advantages of percutaneous pedicle screws have become more apparent. If a prospective study of associated changes in clinical symptoms with a long-term follow-up period can be conducted, we may be able to prove that use of percutaneous pedicle screws can decrease the incidence of adjacent segment disease.
References
1. An SD, Cho TH, Park YK, Kim SH, Park JY, Seo JK. Adjacent segment instability after posterior lumbar fusion: comparison between subtotal laminectomy and total laminectomy. Korean J Spine 2010 7(3):150-154.
2. Anand N, Baron EM, Thaiyananthan G, Khalsa K, Goldstein TB. Minimally invasive multilevel percutaneous correction and fusion for adult lumbar degenerative scoliosis: a technique and feasibility study. J Spinal Disord Tech 2008 21:459-467. PMID: 18836355.


3. Bennett GJ. Spondylolysis and spondylolisthesis. In: Youmans JR editors. Neurological surgery. ed 4. Philadelphia: W.B. Sauders company; 1996.Vol 3: p.2416-2431.
5. Brantigen JW, Steffee AD. A carbon fiber implant to aid interbody lumbar fusion; Two-year clinical results in the first 26 patients. Spine 1993 18:2106-2107. PMID: 8272967.


6. Foley KT, Gupta SK, Justis JR, Sherman MC. Percutaneous pedicle screw fixation of the lumbar spine. Neurosurg Focus 2001 10:E10PMID: 16732626.

7. Gaines RW Jr. The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am 2000 82:1458-1476. PMID: 11057475.


8. Gejo R, Matsui H, Kawaguchi Y, Ishihara H, Tsuji H. Serial changes in trunk muscle performance after posterior lumbar surgery. Spine 1999 24:1023-1028. PMID: 10332796.


9. Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am 2004 86:1497-1503. PMID: 15252099.


10. Holly LT, Schwender JD, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications. Neurosurg Focus 2006 20:E6PMID: 16599422.

11. Kang JS, Lee YK, Cho J, Moon CT, Chang SK. Changes of muscle related enzymes after posterior approaches to the lumbar spine. J Korean Neurosurg Soc 2004 35:23-28.
12. Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery. Part 2: Histologic and histochemical analyses in humans. Spine 1994 19:2598-2602. PMID: 7855687.


13. Kim HS, Park KH, Ju CI, Kim SW, Lee SM, Shin H. Minimally invasive multi-level posterior lumbar interbody fusion using a percutaneously inserted spinal fixation system: technical tips, surgical outcomes. J Korean Neurosurg Soc 2011 50:441-445. PMID: 22259691.



14. Lehmann TR, Spratt KF, Tozzi JE, Weinstein JN, Reinarz SJ, el-Khoury GY, et al. Long-term follow-up of lower lumbar fusion patients. Spine 1987 12:97-104. PMID: 2954220.


15. Lim TK, Lee SG, Park CW, Kim WK. Comparative Analysis of Clinical Outcomes and Adjacent Level Angle Change on Single-level Lumbar 4-5 Fusion Using Percutaneous Screw Fixation and Open Screw Fixation. Korean J Spine 2010 7(4):228-233.
16. Lowery GL, Kulkarni SS. Posterior percutaneous spine instrumentation. Eur Spine J 2000 9:S126-S130. PMID: 10766069.



17. Magerl F. External skelectal fixation of the lower thoracic and the lumbar spine. In: Uhthoff HK, Stahl E editors. Current Concepts of External Fixation of Fracture. New York: Springer-Verlag; 1982. p.353-366.
18. McLaughlin MR, Haid RW Jr, Rodts GE Jr, Subach BR. Posterior lumbar interbody fusion: indications, techniques, and results. Clin Neurosurg 2000 47:514-527. PMID: 11197722.

19. Okuda S, Iwasaki M, Miyauchi A, Aono H, Morita M, Yamamoto T. Risk factors for adjacent segment degeneration after PLIF. Spine 2004 29:1535-1540. PMID: 15247575.


20. Oppenheimer JH, DeCastro I, McDonnell DE. Minimally invasive spine technology and minimally invasive spine surgery: a historical review. Neurosurg Focus 2009 27:E9PMID: 19722824.


21. Park Y, Ha JW. Comparison of one-level posterior lumbar interbody fusion performed with a minimally invasive approach or a traditional open approach. Spine 2007 32:537-543. PMID: 17334287.


22. Penta M, Sandhu A, Fraser RD. Magnetic resonance imaging assessment of disc degeneration 10 years after anterior lumbar interbody fusion. Spine 1995 20:743-747. PMID: 7604353.


23. Prafulla KS. Percutaneous pedicle screw and rod insertion for fracture of the lumbar spine. Indian J Neurotrauma 2005 2:143-148.

24. Rantanen J, Hurme M, Falck B, Alaranta H, Nykvist F, Lehto M, et al. The lumbar multifidus muscle five years after surgery for a lumbar intervertebral disc herniation. Spine 1993 18:568-574. PMID: 8484147.


25. Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop Relat Res 1986 203:7-17. PMID: 3955999.

26. Sihvonen T, Herno A, Paljarvi L, Airaksinen O, Partanen J, Tapaninaho A. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine 1993 18:575-581. PMID: 8484148.


27. Steffee AD, Sitkowski DJ. Posterior lumbar interbody fusion and plates. Clin Orthop Relat Res 1988 227:99-102. PMID: 3338227.


28. Styf JR, Willen J. The effects of external compression by three different retractors on pressure in the erector spine muscles during and after posterior lumbar spine surgery in humans. Spine 1998 23:354-358. PMID: 9507625.


29. Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG. Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine 1997 22:210. -219. discussion 219-220. PMID: 9122804.


30. Thomsen K, Christensen FB, Eiskjaer SP, Hansen ES, Fruensgaard S, Bunger CE. 1997 Volvo Award winner in clinical studies. The effect of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spinal fusion: a prospective, randomized clinical study. Spine 1997 22:2813-2822. PMID: 9431617.


31. White AA, Panjabi MM. Clinical Biomechanics of the Spine. 2nd ed. Philadelphia, PA: Lippincott Company; 1990. p.349-360.
32. Yuan HA, Garfin SR, Dickman CA, Mardjetko SM. A Historical Cohort Study of Pedicle Screw Fixation in Thoracic, Lumbar, and Sacral Spinal Fusions. Spine 1994 19:2279S-2296S. PMID: 7817243.


Fig. 2
Series of lumbar spine of patient who underwent reoperation caused Adjacent segment syndrome. (A) Pre-operative lateral view revealed degenerative spondylolisthesis of L3-4-5. (B) Post-operative lateral view revealed posterior lumbar interbody fusion and posterolateral spinal fusion on L3-4-5. (C) The last follow-up lateral view revealed newly degenerative spondylolisthesis of L2 on 3 and disc space narrowing. (D) Post-operative lateral view revealed additional posterolateral spinal fusion on L2-3-4-5.

- TOOLS
-
METRICS

-
- 4 Crossref
- Scopus
- 6,699 View
- 67 Download
- Related articles in NS
-
Journal Impact Factor 3.2