|
 |
- Search
Abstract
Objective
To analyze the effect of vertebroplasty on costal pain which develops following osteoporotic thoracic compression fractures (OTCFs).
Methods
The authors reviewed the medical records of 35 patients who underwent vertebral augmentation for the treatment of OTCFs over a five year period. The patients were divided into two groups: the costalgia group included patientswho had costal pain after a vertebral fracture and the non-costalgia group included patients without costalgia. To evaluate the effect of vertebroplasty on costal pain and factors related to costal pain, several factors including: vertebral body fracture type, pedicle injury, bone mineral density, the fracture level and clinical outcome were confirmed with magnetic resonance imaging and chart reviews.
Results
Among 35 patients, ten patients (28.6%) complained of costal pain with back pain. Only five of the ten patients (50%) had improved costal pain after a vertebroplasty. In the remaining 5 patients, the costal pain was improved through the use of medication including pain killers or a costal block during the follow-up period. Although the incidence of wedge deformity in the costal group was low(10%), there was no significant relationship to the incidence of costal pain statistically. Pedicle injury, bone mineral density and the fracture level had no significant relation to costal pain.
Conclusion
The patients with wedge type, OTCFs may have a low incidence of costal pain as compared to those patients with bi-concave and crush deformities. The vertebroplasty effect on costal pain may not be effective. Therefore, before doing vertebroplasty, the surgeon should advise patients of this potential outcome in those treated for OTCFs.
Since percutaneous vertebroplasty as a treatment option for vertebral angioma was reported in 1987, minimally invasive management including vertebroplasty (VP) and kyphoplasty (KP) using bone cement has been a popular treatment option for osteoporotic compression fractures2,8,15,24). Several studies showed the comparable outcome of patients without VP to patients with VP, and many articles have presented the effectiveness of a VP on the clinical outcome1,3,7,12). However, some patients who exhibit osteoporotic compression fractures in the thoracic spine complained of back pain and pain of nonmidline areas such as the rib, chest, hip, groin, and buttocks, simultaneously6,10,18,19). Among the non-midline pains, the ribs were the most common site and, the overall response of VP for the non-midline pain was 83%10).
The purpose of this study was to evaluate the effect of vertebroplasty on costal pain and to identify factors related to costal pain for patients with osteoporotic thoracic compression fractures.
We retrospectively reviewed the charts and radiographs of patients who were treated with vertebral augmentation for vertebral compression fractures from January 2005 to January 2010. Thirty-five patients were selected according to the following inclusion criteria: (1) the patients were diagnosed with osteoporosis (T score <-2.5 in vertebral body or femur neck) before vertebral augmentation, (2) both the MRI and radiography revealed a recent thoracic vertebral fracture, and (3) vertebral augmentation, such as percutaneous VP or KP was performed on osteoporotic compression fractures. Patients were divided into two groups: the costalgia group consisted of 10 patients with concordant costal pain to the fractured level and the non-costalgia group which consisted of 25 patients without costal pain. The patients with costal pain who also represented rib fractures were excluded. The costal pain must have developed before a VP or KP and, the costal pain must not have been induced by direct compression on rib. The amount of cement at vertebroplasty was around 3.5-4 cc in all cases with thoracic vertebral fracture. A costal block procedure was performed in the following manner: the patient lay on the surgical table in a prone position. The surgeon palpated the intercostal space and inserted the needle until it contacted the inferior edge of the rib. The needle would scrape underneath the inferior border of the rib and reach the subcostal groove. After the injection of contrast materials to identify the neurovascular bundle under fluoroscopy guidance, 2 cc of mixed fluid (0.5 cc triamcinolone and 1.5 cc bupivacaine) would be injected into the space.
Information including bone mineral density (BMD) of the vertebral body, the level, and type of fracture, the presence of pedicle injury, age, sex, unilateral or bilateral injection of bone cement and the amount of bone cement were obtained from the patients' medical records and magnetic resonance imaging (MRI). The fracture types of the vertebral body were classified as three deformities: (1) wedge, (2) biconcave, and (3) crush deformities9). The pedicle injury is described as the signal change like the high signal intensity on T2 weighted image in the pedicle and not a fracture of pedicle. Parameters such as the fracture type and the pedicle injury were taken to assess whether an injury to the foraminal area in the thoracic veterbra had a relationship to costal pain. Clinical outcomes regarding costal pain were assessed for up to one year following VP or KP.
The student's T-test and Fisher's exact test were used for statistical analysis. p<0.05 was considered statistically significant. Pearson's chi-square test was used to evaluate the statistical significance of several parameters. Statistical analyses were performed using SPSS version 17.0 ( SPSS, Chicago, IL, USA).
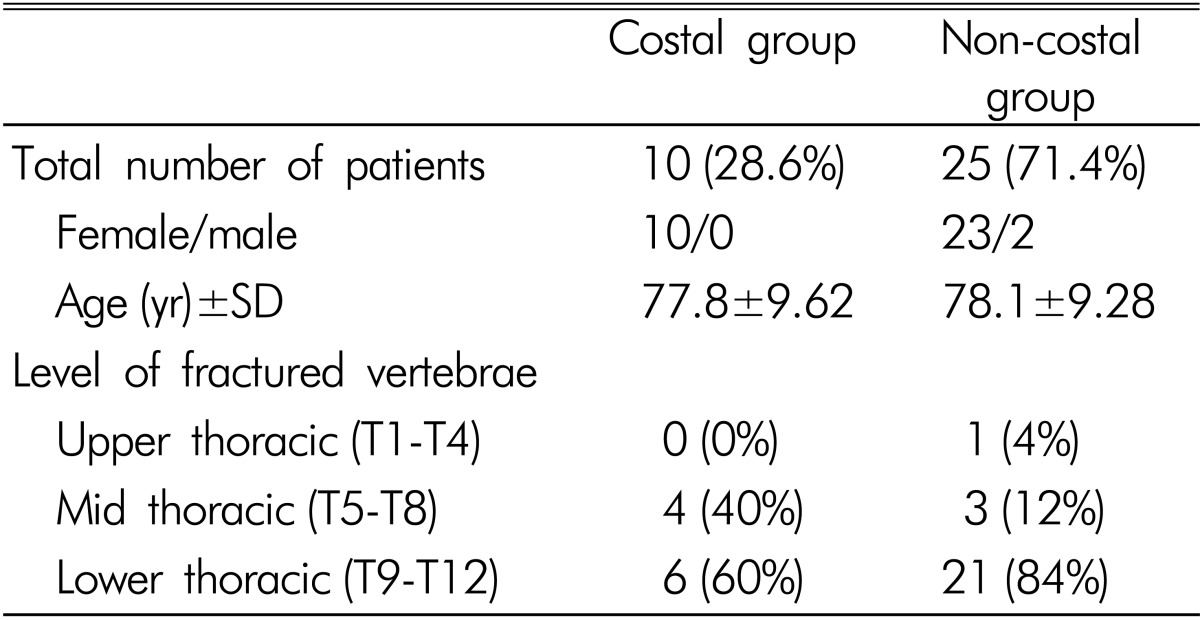
We identified thoracic vertebral fractures with an incidence of costal pain in 10 (28.6%, costal group) of the 35 total patients. Twenty-five patients (the entire non-costal group) did not suffer from costal pain. The average ages of the patients in the costal and non-costal groups were 77.8┬▒9.62 years and 78.1┬▒9.28 years, respectively. In both groups, the lower thoracic level (T9-T12) was the most common level of fracture identified (Table 1).
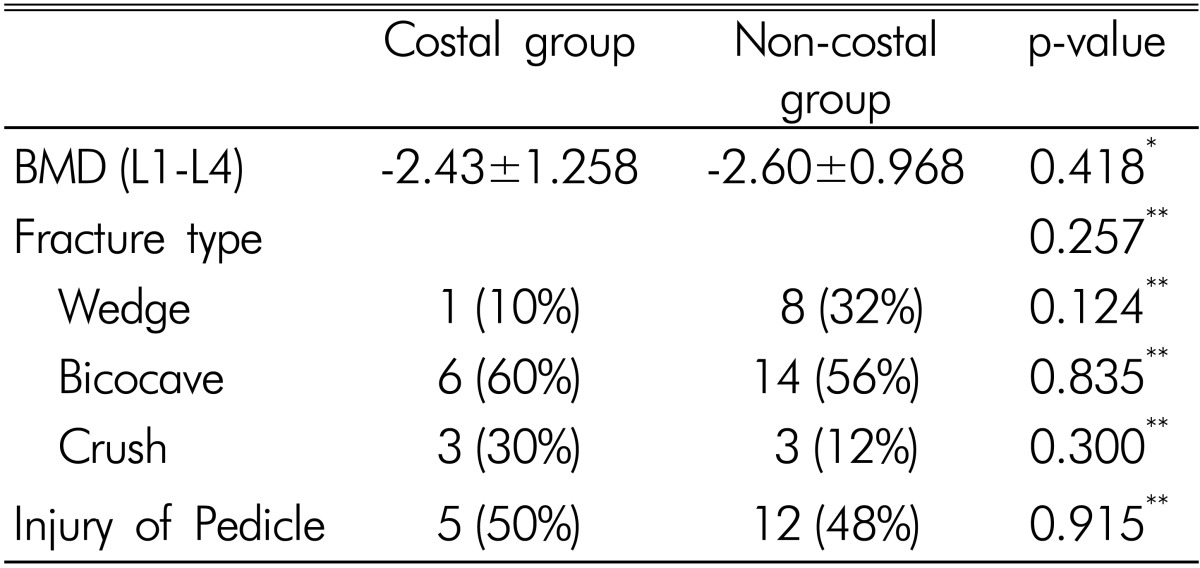
The mean BMD(T-score of L1-4) of costal and non-costal groups were -2.43┬▒1.258 and -2.60┬▒0.968 (p=0.418), respectively. In the classification of fracture type, the incidence of biconcave deformity was higher than other types in both groups. In the costal group, the incidence of the wedge type was 10% as compared to 32% in the non-costal group. Although there was no significant difference in the incidence of wedge deformity between the two groups (p=0.124), the incidence of a wedge fracture in the costal group was relatively low. Injuries of the pedicle in the costal and non-costal groups developed in half of the cases (5 cases, 50% vs. 12 cases, 48%, respectively) (Table 2).
The amount of bone cement and unilateral or bilateral approach were not significant factors related to the change of costal pain. And, the pedicle injury, BMD, the fracture level had no significant relation to the costal pain.
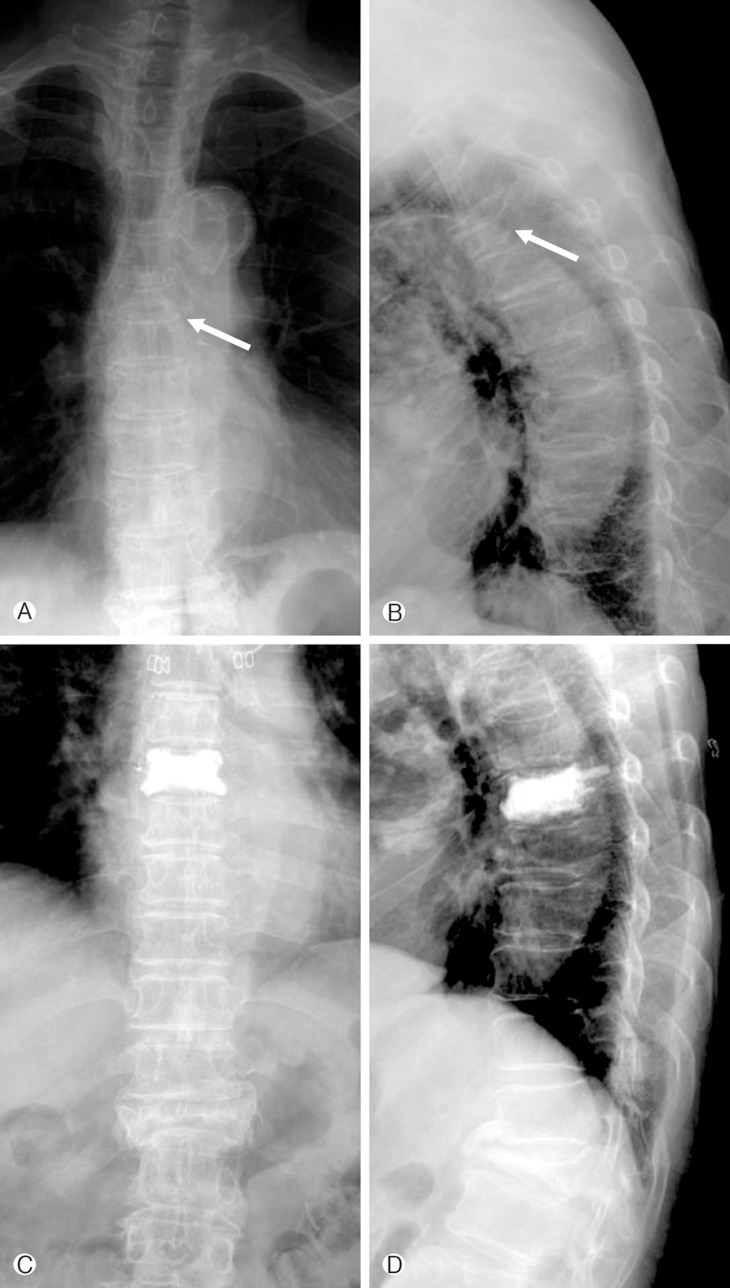
Five patients (50%) in the costal group had a reduction in costal pain after the VP (Fig. 1). Out of ten patients, the remaining five patients complained of consistent costal pain after VP. They were then treated with medications including: non-steroidal anti-inflammatory drugs and two patients underwent a costal block simultaneously. One year following treatment, there were no reported incidents of costal pain in any patients within the study.
The incidence of osteoporotic vertebral fractures in the elderly population has increased substantially. Following the occurrence of osteoporotic vertebral compression fractures, several sequelae including vertebral collapse, spinal deformity, back pain, increased disability, femur fracture, and increased mortality rates could develop4,20,21). Patients with these injuries present with both localized and non-localized back pain after osteoporotic vertebral compression fractures. Multiple symptomatic or non-symptomatic vertebral compression fractures induce a noticeable loss of height. Because localized tenderness does not necessarily indicate an injury of the posterior element during physical examination, the pain does not allow for a distinction between vertebral body fractures and posterior column fractures13). In the acute phase of compression fractures, augmentation of the vertebral body using VP results in the relief of back pain and the increase in height of the collapsed vertebral body11,16). Gray ramus communicans nerve block for a painful osteoporotic compression fracture in thoracic and lumbar spine was useful for the relief of vertebral pain5).
To our knowledge, there are few reports regarding the incidence of costal pain following an osteoporotic vertebral compression fracture10,17). Also, some patients who exhibit osteoporotic compression fractures in the thoracic spine would complain of back pain and pain in non-midline areas such as the rib, chest, hip, groin, and buttock, simultaneously6,10,18,19). Among the non-midline pains, the ribs were the most common site and, the overall response of VP on non-midline pain was 83%10). In this study, a third of the patients (28.6%) with osteoporotic compression fractures in the thoracic spine had costal pain simultaneously. No tenderness of the rib cage was indicated and no rib fractures were identified.
The thoracic radiculopathy like as costal pain to the anterior thorax, chest, or abdomen may be explained as the referred pain of the ventral rami of the thoracic spine17). The costal pain developed more frequently in non-wedge deformities than wedge-type fracture in our study. Our results indicate that middle column injuries could be an important factor that leads to costal neuralgia following costal nerve injury. Arteries, veins and nerves pass the vertebral foramen and may be involved in the injury. Also, to protect the spinal nerve in the thoracic spine, the extraforaminal ligament attaches to the thoracic spinal nerve, which may serve in a protective function against traction and compression of the thoracic spinal nerves14). After traumatic injury near the extraforaminal area, the swelling or buckling of the ligament could have an effect on the compression of the nerve and then, costal pain could develop. Therefore, a middle column injury that contains the intervertebral foramen could affect the costal nerve and induce costal pain at the concordant vertebral fracture level. Other studies showed a favorable outcome of rib pain after VP10,17). The rate of costal pain relief after VP was 50% in this study. Because there was a difference of the response of VP for costal pain among studies, we could not put forward the effect of VP on pain relief of rib area.
This study has several limitations, including its small sample size, retrospective nature, the lack of significance identified in several factors between the two groups and the fact that vertebroplasty and kyphoplasty were considered simultaneously. Future studies should consider the aforementioned areas.
References
1. Alvarez L, Alcaraz M, Perez-Higueras A, Granizo JJ, de Miguel I, Rossi RE, et al. Percutaneous vertebroplasty: functional improvement in patients with osteoporotic compression fractures. Spine (Phila Pa 1976) 2006 31:1113-1118. PMID: 16648745.


2. Berlemann U, Ferguson SJ, Nolte LP, Heini PF. Adjacent vertebral failure after vertebroplasty. A biomechanical investigation. J Bone Joint Surg Br 2002 84:748-752. PMID: 12188498.


3. Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med 2009 361:557-568. PMID: 19657121.


4. Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D. Risk of mortality following clinical fractures. Osteoporos Int 2000 11:556-561. PMID: 11069188.


5. Chandler G, Dalley G, Hemmer J, Seely T. Comparison of Thoracic versus Lumbar Gray Ramus Communicans Nerve Block in the treatment of painful osteoporotic vertebral compression fracture. Pain Physician 2000 3:240PMID: 16906202.


6. Chung SK, Lee SH, Kim DY, Lee HY. Treatment of lower lumbar radiculopathy caused by osteoporotic compression fracture: the role of vertebroplasty. J Spinal Disord Tech 2002 15:461-468. PMID: 12468971.


7. Diamond TH, Champion B, Clark WA. Management of acute osteoporotic vertebral fractures: a nonrandomized trial comparing percutaneous vertebroplasty with conservative therapy. Am J Med 2003 114:257-265. PMID: 12681451.


8. Galibert P, Deramond H, Rosat P, Le Gars D. [Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty]. Neurochirurgie 1987 33:166-168. PMID: 3600949.

9. Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993 8:1137-1148. PMID: 8237484.


10. Gibson JE, Pilgram TK, Gilula LA. Response of nonmidline pain to percutaneous vertebroplasty. AJR 2006 187:869-872. PMID: 16985127.


11. Hiwatashi A, Moritani T, Numaguchi Y, Westesson PL. Increase in vertebral body height after vertebroplasty. AJNR Am J Neuroradiol 2003 24:185-189. PMID: 12591631.


12. Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 2009 361:569-579. PMID: 19657122.



13. Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J 2006 6:479-487. PMID: 16934715.


14. Kraan GA, Hoogland PV, Wuisman PI. Extraforaminal ligament attachments of the thoracic spinal nerves in humans. Eur Spine J 2009 18:490-498. PMID: 19165508.



15. Melton LJ 3rd. Epidemiology of spinal osteoporosis. Spine (Phila Pa 1976) 1997 22:2S-11S. PMID: 9431638.


16. Nakano M, Hirano N, Ishihara H, Kawaguchi Y, Watanabe H, Matsuura K. Calcium phosphate cement-based vertebroplasty compared with conservative treatment for osteoporotic compression fractures: a matched case-control study. J Neurosurg Spine 2006 4:110-117. PMID: 16506477.


17. O'Connor RC, Andary MT, Russo RB, DeLano M. Thoracic radiculopathy. Phys Med Rehabil Clin N Am 2002 13:623-644. PMID: 12380552.


18. Patel U, Skingle S, Campbell GA, Crisp AJ, Boyle IT. Clinical profile of acute vertebral compression fractures in osteoporosis. Br J Rheumatol 1991 30:418-421. PMID: 1836154.


19. Peh WC, Gilula LA. Percutaneous vertebroplasty: indications, contraindications, and technique. Br J Radiol 2003 76:69-75. PMID: 12595329.


20. Ross PD, Davis JW, Epstein RS, Wasnich RD. Pre-existing fractures and bone mass predict vertebral fracture incidence in women. Ann Intern Med 1991 114:919-923. PMID: 2024857.


21. Schlaich C, Minne HW, Bruckner T, Wagner G, Gebest HJ, Grunze M, et al. Reduced pulmonaryfunction in patients with spinal osteoporotic fractures. Osteoporos Int 1998 8:261-267. PMID: 9797911.


22. Song JC, Bak KH, Cho DC, Hong HJ, Kim JM, KimCH . The effect of early percutaneous vertebropalsty in occult osteoporotic vertebral frcture. Korean J Spine 2008 5:173-177.
Fig.┬Ā1
Case of the resolved costal pain after vertebroplasty. This picture shows the x-ray radiographies of patient with improved costal pain after vertebroplasty. The simple x-ray antero-posterior (A) and lateral (B) views showed the T6 compression fracture (arrow). After vertebroplasty at the compression fracture, the simple X-ray antero-posterior (C) and lateral view (D) showed the increased vertebral height.

- TOOLS
-
METRICS

-
- 2 Crossref
- Scopus
- 12,763 View
- 78 Download
- Related articles in NS
-
Journal Impact Factor 3.2