Monostotic Paget Disease of the Lumbar Vertebrae: A Pathological Mimicker
Article information
Abstract
Paget disease is a metabolic disorder involving abnormal bone turnover that consists of 3 phases: the initial lytic phase, the intermediate mixed phase, and the chronic sclerotic phase. Paget disease mostly presents as polyostotic or monostotic lesions of the spine, and is rare on the Indian subcontinent. We present a case of isolated Paget disease of the lumbar third vertebra, which was confirmed only at biopsy. The patient presented with chronic low backache with a developing neurological deficit. We managed the patient with posterior spinal stabilisation, using pedicular screws and vertebroplasty of the collapsed vertebrae to regain the height. Upon the diagnosis of Paget disease, the patient was treated with calcitonin and bisphosphonates for 3 months, along with regular monitoring of alkaline phosphatase levels. Through this case, we hope to emphasize that Paget disease should be considered in the differential diagnosis of lytic lesions. Additionally, the alkaline phosphatase level in this patient was high-normal, which was an aspect of the role of Paget disease as a mimicker. Confirmatory biopsy is mandatory in all lesions.
INTRODUCTION
Low back pain is a common problem causing economic and social morbidity. Back Pain is multifactorial and Paget disease is an uncommon cause for low back pain in Indian subcontinent [1]. Paget disease is a metabolic disorder characterised with focal areas of excessive osteoclastic bone resorption accompanied with secondary increase in osteoblastic bone formation involving the skeletal system [2]. We report a case of solitary vertebral involvement with central compression of body and lysis of lumbar spine which turned into Paget disease on biopsy. Importance of this article is to consider Paget disease as an important differential diagnosis in management of patients presenting with chronic low backache and isolated lumbar collapse with lysis. Very few reports are being quoted in literature from Indian subcontinent.
CASE REPORT
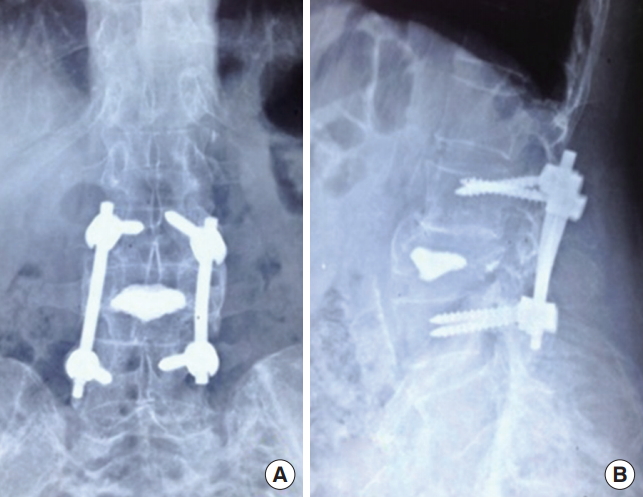
Seventy-nine-year old man presented with low backache which was dull aching for 6 months duration. He was a farmer by occupation and was on conservative management. His low backache did not subside and radiculopathy started on his left side. Tenderness was present at L3 vertebrae. Radiological examination revealed a near complete compression L3 vertebrae with end plate sclerosis (Fig. 1). Radiological differentials were osteoporotic compression fracture, metastasis and infective spondylitis. Blood investigations were clinically in normal range with erythrocyte sedimentation rate, 21 mm/hr, neutrophils, 69%, and lymphocyte, 20%. Alkaline phosphatase level was in upper limit of normal range – 240 U/L (range, 100–260 U/L). Serum electrophoresis and prostate specific antigen were normal and done to rule out myeloma and sclerotic metastasis from prostate. Mantoux test was positive. Computed tomography scan revealed a lysis in the marrow region with peripheral sclerosis. Magnetic resonance imaging (MRI) images revealed destruction of L3 vertebrae with disc dehydration of L2–3 and L3–4 and evidence of mild cord compression (Fig. 2).
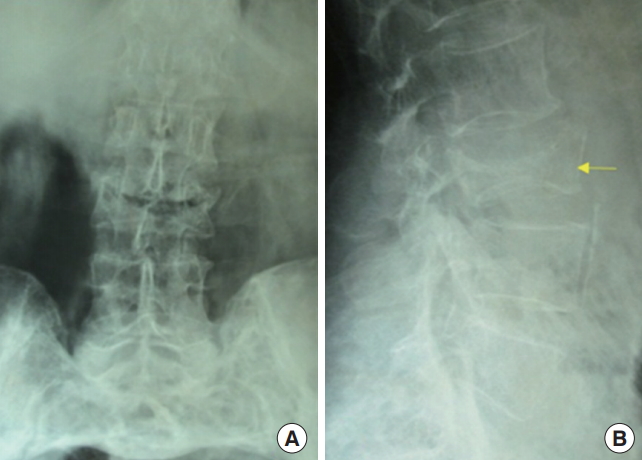
Plain radiograph of the lumbar spine anterior-posterior view (A) and lateral view (B) showing near complete compression of the body of L3 vertebra with sclerosis of end plates (shown with the arrow).

(A) Computed tomography image of the L3 vertebra axial section showing lysis of the vertebral body. (B) Magnetic resonance imaging image of the lumbar spine, axial section of T2 weighted turbo spin sequence showing central hyper-intense lysis surrounded by hypo-intense bone. (C) Coronal section of lumbar spine T2 weighted sequence showing destruction of the central body with intact posterior border. The arrows in the panel C depicts the marking of L1 and L5 vertebra.
Since there was mild compression of the nerve roots with neurological deficit leading to mild weakness (grade 4/5) of ankle dorsiflexion. Patient underwent posterior spinal stabilisation with pedicle screws. Vertebroplasty was done to regain the vertebral height since the anterior and posterior borders were intact. Postoperative period was uneventful with no new neurological deficit. Biopsy was reported as Paget disease. Microscopic examination showed a benign fibro-osseous pattern with osteoclastic giant cells and fine strands of fibrosis (Fig. 3). Now patient is at 2-year follow-up with intact neurological status (Fig. 4).
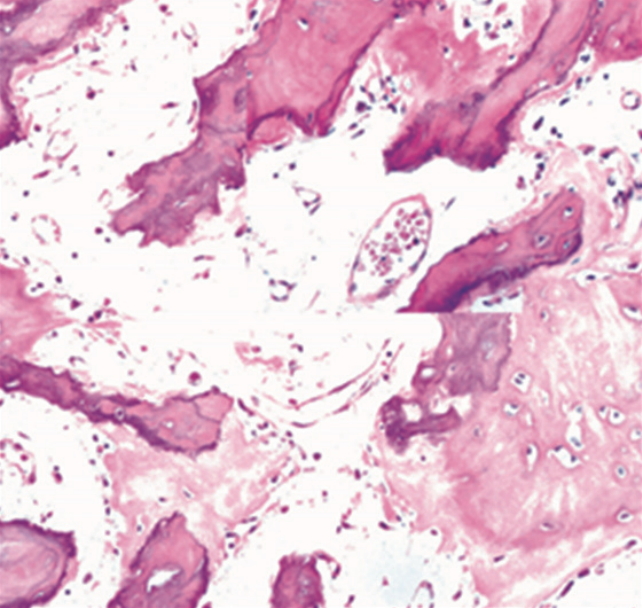
Histopathological image in low power (×10) stained with eosin and haematoxylin showing primarily woven bone with focal mosaic pattern of lamellar bone resembling jigsaw puzzle with irregular cement lines with osteoclasts and fine fibrous strands present in marrow.
DISCUSSION
Paget disease (osteitis deformans) was first coined by James Paget in 1877. It is defined as a chronic disorder with disturbance in the rate of bone turnover involving focal areas of excessive osteoclastic bone resorption by giant osteoclasts followed by secondary osteoblastic activity. This disease has a male predilection of 1.8:1 with mean age involvement of 55 years. It is second most common disorder after osteoporosis [2,3].
Pelvis is most commonly involved in 70% of cases and spine in 53% of cases. It is common in UK, Australia, New Zealand, and people of Anglo-saxon origin but uncommon in Asians, Scandinavians, and black Africans [4].
It has a strong genetic component with mutations in the chromosome 1/p62. Mutations in SQSTM1/p62 are also found in Paget disease which play an important role in osteoclastic differentiation and activation in response to the cytokines like interleukin-1. Environmental factors and viral etiology like paramyxovirus also play a causative factor [5].
Most commonly the disease involves pelvis, lumbosacral spine, skull, femur or tibia but literally any bone may be affected clinically by the disease [6,7]. Pelvis is commonly involved followed by spine. Lumbar spine is often involved which leads to chronic low backache and spinal canal stenosis. Back pain in Paget disease is also contributed to blood engorgement in vertebral body due to disorganised, hyperactive vascular remodelling process and also due to periosteal stretching [1]. Sometimes the disease is inactive and is diagnosed only with isolated increased serum alkaline phosphatase activity [8,9].
Clinically Paget disease may present with pain which may be constant, diffuse or localised which may arise due to microfracture or lysis. Paget disease may present with secondary osteoarthritis of joint. Deformity of local bone such as bowing of long bones like tibia or femur occur due to abnormal distribution of forces. Mechanical pain of the affected limb can arise due to cortical fissuring arising from abnormal mechanical forces on bone. The most common neurological complication is conductive or sensoneural deafness arising from compression of eight cranial bone in the petrous part of temporal bone. Other neurological problems include vertigo, spinal cord compression, local compression syndromes, cranial nerve palsies, hydrocephalus, brain stem compression from basilar invagination [10].
Paget disease commonly presents as polyostotic lesion (35%–50%) and less than 20% present as monostotic lesions which are rare in India. Polyostotic lesion presents with bone pain due to increased turn over. Lesions in the lumbar spine commonly present with chronic low back-ache. Vertebral monostotic lesion of lumbar spine in Indian subcontinent are rare with only few cases reported [11-16].
Paget disease consist of an initial lytic phase, intermediate mixed phase and a late blastic phase. In bones with less trabecular/cortex ratio like skull, femur and humerus, Paget disease produce a leading edge in lytic phase [17].
Biochemistry investigations reveal an increase in bone turnover with a marked increase of alkaline Phosphatase in active lesions but in monostotic lesion alkaline Phosphatase level is usually in high normal range. Alkaline phosphatase iso-enzyme assessment increases the specificity. Vitamin D deficiency can also mimic with raised alkaline phosphatase level and bone pain hence correction is needed before starting bisphosphonate therapy in Paget disease. In urine examination, during osteoclastic phase there is increased urinary hydroxyproline and pyridinoline. In osteoblastic phase there is increase in bone alkaline phosphatase and osteocalcin [18].
Radiologically in lytic phase, they present as focal lytic lesions or flame shaped advancing edge in long bones. In mixed and blastic stage, there is thickening of trabecular bone, cortical thickening and deformity. Classically they form a picture frame vertebrae in spine which is due to a combination of trabecular bone hypertrophy, thickening of end plate with apposition and adsorption of new bone on the periosteal and endosteal surface of the anterior and posterior vertebral borders with central translucency. Clinico-radiologically they mimic spinal metastasis. Bone scan may be needed and in bone scan they appear like a clover image when the vertebral pedicles and spinous process are affected and like a heart when vertebral body and spinous process are involved [19,20]. Final confirmative diagnosis is only by biopsy.
Treatment of Paget disease consists a combination of bisphosphonates and calcitonin for three month duration. Indication for treatment includes pain in Pagetic bone, neurological complication, osteolytic lesion with increased fracture risk, involvement of long bones, vertebrae, base of skull, asymptomatic joint involvement and patients undergoing surgery on Pagetic bones. Calcitonin is used in milder forms of disease. Calcitonin acts through a specific receptor to alter cell function by a cyclic adenosine monophosphate mediated system. The common drug dosage include pamidronate 60 mg intravenously, alendrnate 40 mg/day, and risedronate 30 mg/day given orally for 3 months. Alkaline phosphatase level should be monitored during treatment initially once in a month, then every 3 months for the first year following treatment. During the next 5 years alkaline phosphatase levels should be monitored every 6 months. Other deformities should not be neglected and prompt management is needed.
In our case, diagnosis of Paget disease was difficult because in initial radiological x-ray it appeared to be a osteoporotic compression, metastatic or myeloma lesion. In MRI sequences it appeared to be of infective pathology owing to the partial destruction of the vertebrae. In view of the ambiguous pathology, we proceeded with the decompression, biopsy, Histo-Pathological examination and stabilisation of spinal segment using pedicle screws in L2 and L4 vertebrae. Since there was only central collapse with intact posterior borders, vertebroplasty of L3 vertebrae was performed. The diagnosis was confirmed as Paget disease only by biopsy. Since there was no other symptomatic lesion in the rest of the skeletal system, diagnosis of monostotic Paget disease was made. Further investigation of bone scan or positron emission tomography scan was not done, in view of cost issues. At 24-month follow-up, patient was asymptomatic with no new neurological deficit. Stabilisation was done in our case to prevent further collapse of vertebrae and prevent neurological recovery. Vertebroplasty was done to regain the height of vertebrae to relieve the osseous pressure and pain. Paget disease should be considered as one of the last diagnosis of a mono-vertebral lesion. Biopsy is only confirmative and treatment depends upon the bone involved and the stage of the disease.
Paget disease is a diagnosis of exclusion. Knowledge of the pathophysiology and the radiological manifestations of the Paget disease, which can present in a lytic or sclerotic phase is helpful in diagnosing Paget disease.
Paget disease can cause various systemic manifestations and metabolic alterations by creating marrow suppression leading to anaemia and hypervascular focus by creating arterio-venous channels. If preoperative knowledge of Paget disease as one of the differential diagnosis of lytic or a sclerotic lesion, can reduce the intraoperative complications like vascular bleeding from the arterio-venous anastomotic vessels. In our case, we used bone cement in vertebroplasty, which acts both like a mechanical spacer and chemical cauterisation of the hypervascular channels. Biopsy and histopathology are must for definitive diagnosis, which are helpful in prompt management of the lesion. Surgical management of stabilisation and fixation did not change in our case, irrespective of the diagnosis of Paget disease.
CONCLUSION
Monostotic Paget disease of the lumbar vertebrae is involved less frequently in the skeletal system and can mimic various pathological conditions like myeloma, metastasis, vertebral osteomyelitis, or osteoporotic compression in an old age man. Complete clinical, biochemical, and radiological work up is needed to rule out various differentials. Importance of Paget disease as a differential diagnosis in the preoperative and intraoperative period will help to plan our management. Definitive diagnosis is only by histopathological examination and prompt management of the vertebral lesion to prevent neurological deterioration. Awareness of Paget disease as a differential for mono-vertebral lesion is needed among clinicians of Indian subcontinent.
Notes
The authors have nothing to disclose.