Percutaneous Endoscopic Thoracic Discectomy in the Upper and Midthoracic Spine: A Technical Note
Article information
Abstract
Despite the successful application of percutaneous endoscopic thoracic discectomy (PETD), its technical feasibility and outcomes for symptomatic upper and midthoracic disc herniation have not been reported yet. The purpose of this article was to evaluate the feasibility of the percutaneous transforaminal endoscopic approach to remove disc herniations in the upper and midthoracic spine. Fourteen consecutive patients (mean age, 42.4 years; 12 males, 2 females) who underwent PETD were included in the analysis. The procedure was performed under local anesthesia and intravenous sedation using the standard endoscopy instrument set. The transforaminal approach combined with foraminoplasty was used to access the herniated areas. Treatment outcomes were evaluated using visual analogue scale (VAS) scores, Oswestry Disability Index (ODI) scores, and the modified MacNab criteria. Four discectomies were performed at T2–3, 5 at T3–4, and 5 at T5–6. The mean follow-up period was 43.4 months, and all patients showed statistically significant postoperative improvement (VAS: 7.3 to 2.3, ODI: 53.5 to 16.9, p<0.05 for all). No serious complications were reported during follow-up. PETD for upper and midthoracic disc herniation is a feasible and effective minimally invasive treatment option with favorable clinical results.
INTRODUCTION
Thoracic disc herniation (THD) is relatively uncommon [1-4]. The incidence has been reported to be 0.25%–0.5% of spinal disc disease [1-4]. However, the diagnosis of TDH is increasing with the development of magnetic resonance image (MRI) [2-4].
Considering the complexity of neural and vascular structures, surgical treatment of upper and mid thoracic disc herniation (UMTDH) is technically challenging [3,4]. Open surgical approach for THD include laminectomy, transpedicular approach, costotransversectomy, and transthoracic approach [5-7]. For upper thoracic levels, axillary approach or transsternal approach is possible trajectory for transthoracic approach [3,4]. Although percutaneous endoscopic thoracic discectomy (PETD) has been introduced, technical feasibility and outcomes for UMTDH have not been reported. The purpose of this report is to describe percutaneous endoscopic approach to remove disc herniation on upper and mid thoracic spine via transforaminal approach.
MATERIALS AND METHODS
1. Patient Population
After approval of the Institutional Review Board by the Wooridul Hospital (WRDIRB-018-002) and receiving informed consent from patients, patients with symptomatic UMTDH who underwent PETD, were retrospectively analyzed. Cases of calcified disc herniations, concomitant ossification of the posterior longitudinal ligament or ossification of the ligamentum flavum, history of trauma and worker’s compensation claim were excluded (Table 1). Total of fourteen consecutive patients (mean age, 42.4 years; 12 males, 2 females), who underwent PETD from 2001 to 2017, were included in the analysis. Four, 5, and 5 discectomies were performed at T2–3, T3–4, and T5–6 levels, respectively. The presenting symptoms varied from dorsal back pain, chest wall pain to visceral pain such as chest tightness. Symptomatic relief after epidural block was used to confirm diagnosis of symptomatic UMTDH. Patients with visceral symptoms underwent mandatory lung, heart and stomach evaluation to exclude nonspinal etiologies. Axial back pain localized to inter- or subscapular region was the most common presenting complaint. Diagnosis was delayed in some cases due to confusing clinical symptoms like radicular chest pain, chest discomfort or heart burn. Three patients had myelopathic clinical presentation with paraparesis and gait disturbance. All the cases were given a trial of conservative treatment before consideration of surgical intervention.
2. Data Analysis
Clinical chart review and telephone survey was performed. Clinical outcomes were assessed using the visual analogue scale (VAS; 0–10, with 0=no pain), and functional outcomes were scored according to the Oswestry Disability Index (ODI; 0%–100%). Patient’s satisfaction was measured with modified MacNab criteria. SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Wilcoxon signed ranks test and matched t-test were employed. A p-value of <0.05 was considered statistically significant.
3. Surgical Procedure
Surgery was performed using local anesthesia and intravenous sedation with patient in prone position. Appropriate skin entry point was determined by drawing a line from posterior annulus at the midpedicular level to lateral margin of facet joint on axial computed tomography scan cuts (Fig. 1A). Skin entry point was commonly located at about 5–6 cm from the midline. Approach trajectory was planned on fluoroscopic lateral view by drawing oblique line from the posterior endplate of the lower vertebra passing the tip of superior articular process to avoid obstruction of thick transverse process and rib head at the costotransverse junction. After local anesthesia infiltration, a 6-inch long, 18-G spinal needle was inserted along planned trajectory under fluoroscopic guidance. The needle tip was placed at the midpedicular level (Fig. 1B). Epidurography was performed followed by epidural anesthetic infiltration. Then, the needle was advanced into the disc space and intraoperative discography was performed by injecting a mixture of radiopaque dye (Telebrix; Guerbet, France), indigo carmine (Carmine; Korea United Pharmaceutical, Yoenki, Korea), and normal saline in a 2:1:2 ratio. Indigo carmine stains the degenerated acidic nucleus blue and helps in identifying the herniated disc fragment. A guide wire was inserted through the needle. Serial dilation and sequential reaming of ventral and lateral aspect of superior facet was done over the guidewire, to enlarge neural foramen (Fig. 1C, D). Foraminoplasty was performed using round reamer or bone-drill. A beveled 7.5-mm outer diameter working cannula was then placed on the posterior disc space through annular window at the midpedicular level (Fig. 1E, F). Then, the 4.7-mm endoscope (TESSYS, Joimax GmbH, Karlsruhe, Germany) was introduced. Under endoscopic visualization, a blue-stained annular surface and part of the disc material could be observed. Initial decompression was performed from central and paramedian disc space. Then the working channel was retrieved posteriorly, close to the epidural space. Due to anatomical characteristic of thoracic vertebra, central disc space is located more ventrally than paramedian disc space. Posterior longitudinal ligament was resected at paramedian/foraminal area, and ventral/lateral surface of thecal sac was exposed. The blue stained herniated fragment of central hernia could be visualized and was removed using microforceps (Fig. 1G, H). After adequate decompression, skin was closed with a single subcuticular suture and sterile dressing was applied. Patients were allowed to ambulate on the same day. Postoperative MRI was performed immediately after operation or on the following day.

Surgical technique. (A) Skin entry point planning on axial computed tomography scan by drawing an imaginary line from posterior annulus at the midpedicular level to lateral margin of facet joint. (B) Placement of needle tip is placed at the midpedicular level. (C, D) Enlargement of foramen by serial dilation and sequential reaming of ventral and lateral aspect of superior facet over guidewire. (E) Placement of beveled 7.5-mm working cannula on the posterior disc space through annular window at the midpedicular level - anteroposterior view. (F) Placement of beveled 7.5-mm working cannula on the posterior disc space through annular window at the midpedicular level - lateral view. (G, H) Removal of herniated disc fragment using microforceps.
RESULTS
Mean follow-up period was 43.4 months (6–120 months). All patients showed statistically significant improvement of both VAS and ODI scores (7.2 to 2.2 for VAS and 44.6 vs. 14.8 for ODI, p<0.05 for all). According to the modified MacNab criteria, 7 (50%), 5 (35.7%) and 2 patients (14.3%) reported excellent, good and fair outcomes, respectively. No serious complication was reported during the follow-up.
1. Case 1
A 35-year-old female presented with severe interscapular pain and chest discomfort for 10-year duration. She underwent physical therapy and epidural steroid injection several time. MRI showed a foraminal TDH at the T2–3 level. PETD was performed under the local anesthesia. Postoperatively the patient showed significant improvement of pain. Using modified MacNab criteria, the clinical outcome was categorized as excellent (Fig. 2).
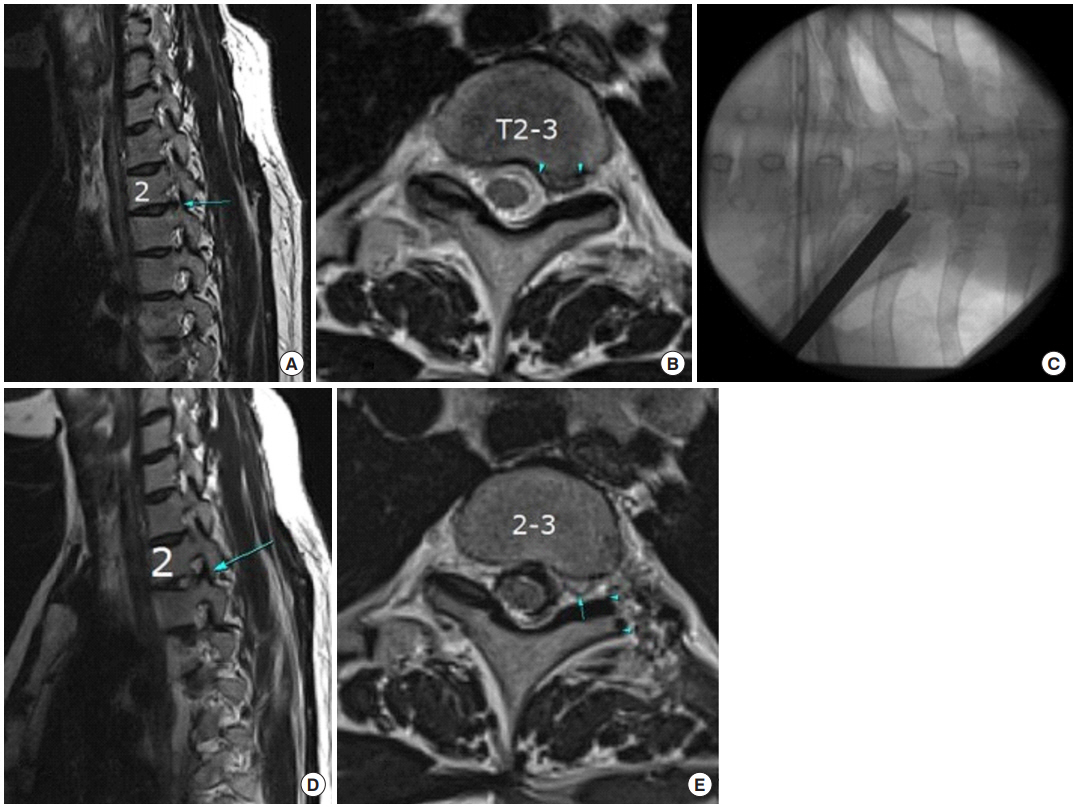
A 35-year-old female patient: (A) Preoperative sagittal view showing foraminal thoracic disc herniation (TDH) at the T2–3 level. (B) Preoperative axial view showing left foraminal TDH at the T3–4 level. (C) Intraoperative fluoroscopic view showing working channel is place at the foraminal area after foraminoplasty. (D) Postoperative sagittal view showing successful removal of disc herniation. (E) Postoperative axial view showing successful removal of disc herniation. Note that T2 nerve root is visible after decompression (arrow) and amount of foraminoplasty (arrowheads).
2. Case 2
A 52-year-old male, presented with upper thoracic back pain and paresthesia on upper chest for 2-year duration, Initial conservative treatment including physical therapy and epidural steroid injection failed to improve his pain. MRI showed central TDH at the C3–4 level. He underwent PETD under the local anesthesia. Postoperatively patient showed significant improvement of pain and discomfort. Using modified MacNab criteria, the clinical outcome was categorized as good and it was maintained during 10 years of postoperative follow-up (Fig. 3).
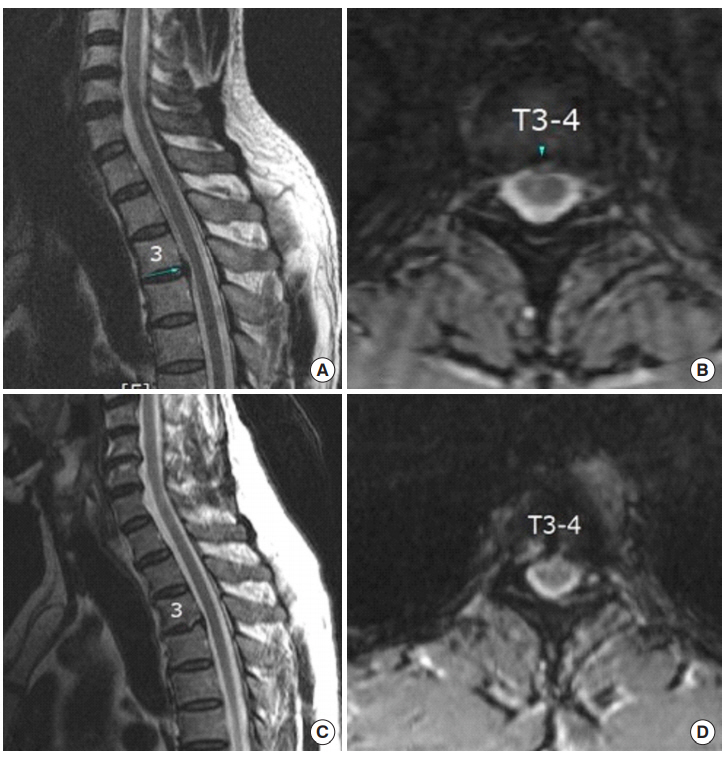
A 52-year-old male patient: (A) Preoperative sagittal view showing central thoracic disc herniation (TDH) at the T3–4 level. (B) Preoperative axial view showing central TDH at the T3–4 level. (C) Postoperative sagittal view showing successful removal of disc herniation. Note that the amount of foraminoplasty to access central part of disc. (D) Postoperative axial view showing successful removal of herniated disc.
DISCUSSION
The current study is unique in evaluating the usefulness of previously described oblique paraspinal endoscopic discectomy technique in surgical management of symptomatic upper and midthoracic disc herniations. A total of fourteen consecutive patients were surgically treated and followed-up over a span of ten years with encouraging results. Satisfactory surgical decompression and clinical improvement was achieved in all the cases without any significant surgical morbidity. Moreover, the use of local anesthesia avoided prolonged hospitalization and facilitated quick postoperative recovery.
PETD has been successfully described in the literature [8-13]. Cho et al. [9] reported successful removal of both soft and calcified compressive lesions in lower thoracic spine by combining paraspinal approach with endoscopic techniques. In 2013, Nie and Liu [10] reported successful outcomes in a case series of 13 endoscopic thoracic discectomies. Similar to Cho et al. [9], they mainly operated at levels below T6-T7 with only 1 case performed at T5–6 [10]. Paolini et al. [11] reported successful removal of calciefied THD at T9–10 level in a 38-year-old man with endoscope assistance [11]. Wagner et al. [12] also reported successful endoscopic removal of T8–9 disc herniation in a young female and suggested usefulness of endoscopic discectomy in thoracic spine. Recently, Xiaobing et al. [13] reported a novel technique to decompress thoracic spinal stenosis utilizing transforaminal endoscopy. Their case series had fourteen cases with majority being performed at lower thoracic levels, except 2 cases which involved T1–2 level [13]. They followed up patients for a mean of 31.2 months and reported successful clinical outcomes [13]. Similar to epidemiological trends of symptomatic upper THDs being extremely rare, the surgical case reports dealing with them are also sparse [4,5,8]. The current study is unique in the sense that it specifically deals with usefulness of PETD in management of upper and mid (T1–6) TDH. As per author group’s knowledge, despite having only 14 patients the current case series is the largest one dealing with upper/midthoracic disc herniations.
Minimally invasive surgical (MIS) techniques have significantly improved outcomes in cervical and lumbar regions. MIS techniques require acquisition of new surgical techniques (e.g., endoscopy), working through narrow anatomical corridors and have a steep learning curve. Nevertheless, the benefits arising out of using MIS techniques can be greatly rewarding both for the patient and treating surgeon. The most challenging aspect of endoscopic thoracic spine surgery is working through a narrow anatomical corridor around highly delicate structures (spinal cord) affording minimum scope of error. As compared to anterior thoracoscopic approaches, posterior thoracic endoscopic approach offers higher manual dexterity to the surgeon, anatomical familiarity, direct approach to ventral epidural space and little approach related morbidity while avoiding dissection around risky anatomical structures, general anesthesia, onelung ventilation, nerve root retraction. Furthermore, PETD does not require use of neuromonitoring as the whole procedure is done under local anesthesia combined with conscious sedation. However, extreme surgical caution is advised as any complication can have catastrophic implications. Although no neurovascular complications were observed in current series, the proximity of major vascular, visceral and neurological structures during PETD is a real concern. The authors advise thorough understanding of 3-dimensional anatomy, sufficient experience with spinal endoscopy techniques and expert patient selection to get optimum results.
CONCLUSION
The current study highlights the possible utilization of posterior spine endoscopy techniques in management of upper THDs. Despite the small number of cases evaluated (due to rarity of symptomatic upper TDH), the results from current series are clinically satisfactory and suggest possible large-scale role of minimally invasive endoscopic techniques in surgical management of symptomatic upper THDs.
Notes
The authors have nothing to disclose.

