A Review of a New Clinical Entity of ‘Central Atlantoaxial Instability’: Expanding Horizons of Craniovertebral Junction Surgery
Article information
Abstract
The author discusses the novel form of central or axial atlantoaxial instability and analyses its clinical significance. High degree of clinical and radiological understanding of the region is mandatory to diagnose and then treat such atlantoaxial instability. Evaluation of alignment of facets of atlas and axis and observations on direct manipulation of facets of atlas and axis forms the basis of diagnosis. The treatment of clinical entities like basilar invagination, Chiari formation, syringomyelia and myelopathy related to cervical spinal degeneration, spinal deformities, ossified posterior longitudinal ligament, and Hirayama disease can be influenced by the understanding of central or axial atlantoaxial instability.
INTRODUCTION
For several decades’ abnormal alteration of atlantodental interval was considered to be the sole parameter to diagnose atlantoaxial instability. Apart from clinical evidences, neural indentation and deformation and alteration in cord signals in the region of the tip of odontoid process have been other parameters that establish the presence of abnormal craniovertebral dynamics and indicate the need for surgical intervention. In the year 2014, we proposed a novel concept that atlantoaxial instability can be present even when there is no bone deformity or malalignment on dynamic imaging and the conventional and validated parameters that determine the presence of atlantoaxial instability are within the range of normal [1]. Such instability was identified as ‘central’ or ‘axial’ atlantoaxial instability (CAAD) [2,3]. Our further experience in the subject identifies that understanding of presence of CAAD can have wide implications in the treatment of a number of commonly encountered clinical entities involving the craniovertebral junction and rest of the spine. We review our published reports on the subject in this article. Other authors are yet to validate these observations.
ATLANTOAXIAL INSTABILITY
Atlantoaxial joint is the most mobile joint of the body. Its round and flat articular surfaces that facilitate circumferential movements at this joint also predispose it to development of instability. Our analysis of the subject, over several years, concludes that amongst all spinal segments, atlantoaxial instability is the most common. The concept is that more is the mobility; more is the possibility of instability. It seems that atlantoaxial instability is an ill-understood and undertreated clinical entity.
CLASSIFICATION OF CAAD
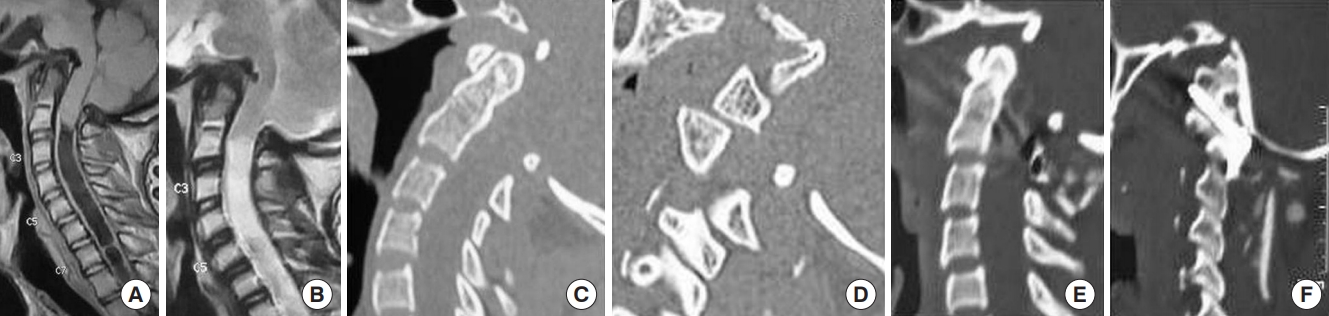
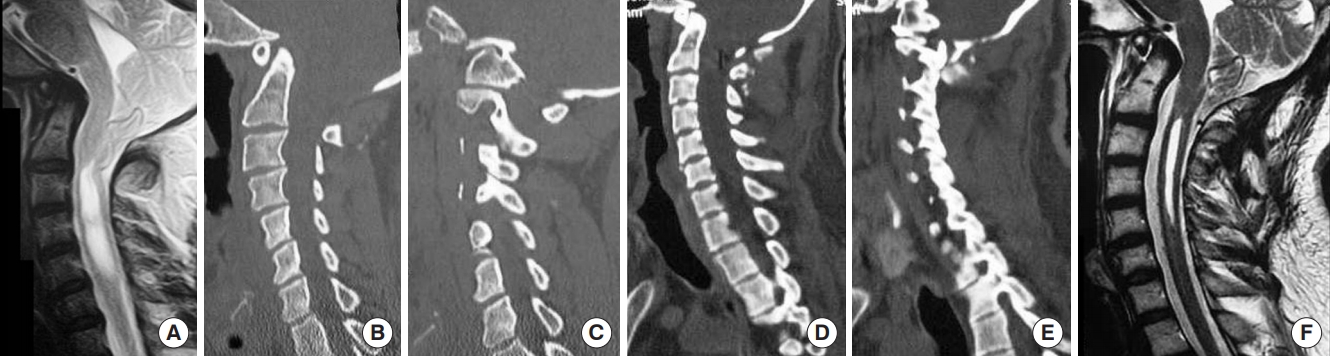
Atlantoaxial instability was diagnosed on the basis of evaluation of alignment of facets on lateral profile imaging with the head in neutral position and by manual manipulation and visual inspection of the atlantoaxial facetal articulation during surgery [1]. Type 1 atlantoaxial facetal instability indicates when the facet of atlas was dislocated anterior to the facet of axis (Fig. 1). Type 2 atlantoaxial facetal instability indicates when the facet of atlas was dislocated posterior to the facet of axis (Fig. 2). In type 3 atlantoaxial facetal instability, the facets were in alignment and instability was diagnosed on the basis of telltale clinical and radiological evidences and confirmed by manual manipulation of bones during the surgical procedure (Fig. 3). In types 2 and 3 atlantoaxial facetal instability, the atlantodental interval may not be abnormally altered and there may not be any neural or dural compression by the odontoid process. Due to these reasons, types 2 and 3 atlantoaxial facetal instability is labeled as CAAD. It is obvious that high degree of clinical suspicion and understanding of the subject is crucial to make such a diagnosis. Considering that there can be a wide spectrum of therapeutic implications of such an understanding, a comprehensive discussion on the subject is mandatory.

Images of a 50-year-old female patient. (A) Computed tomography (CT) scan with the head in neutral position showing abnormal increase in the atlantodental interval. There is assimilation of atlas and C2–3 fusion. Posterior foramen magnum decompression has been done. (B) CT scan with sagittal cut passing through the facets showing facet of atlas dislocated anterior to facet of axis – type 1 atlantoaxial facetal dislocation. (C) T2-weighted magnetic resonance imaging showing neural indentation by the odontoid process. (D) Postoperative CT scan showing reduction in atlantoaxial dislocation and craniovertebral junction realignment. (E) Postoperative CT scan showing the implant. The facets are now in alignment.
Images of a 19-year-old male patient. (A) T1-weighted magnetic resonance imaging (MRI) showing severe basilar invagination. (B) T2-weighted MRI. (C) Computed tomography (CT) scan showing no atlantodental interval abnormality. (D) CT scan showing type 2 atlantoaxial facetal instability. The facet of atlas is dislocated posterior to the facet of axis. (E) Postoperative CT scan. (F) Postoperative CT scan showing the implant.

Images of a 33-year-old male patient. (A) T2-weighted magnetic resonance imaging (MRI) showing basilar invagination and Chiari formation. (B) Computed tomography (CT) scan showing basilar invagination. There is no abnormality in atlantodental interval. (C) The facets of atlas and axis are in alignment. Clinical and radiological features suggest type 3 atlantoaxial facetal instability. (D) Postoperative CT scan. (E) Postoperative CT scan showing the implant.
CLINICAL SYMPTOMS
In type 1 atlantoaxial facetal instability the atlantodental interval is usually abnormally altered and odontoid process is angled acutely posteriorly. The odontoid process compresses on the dural tube and neural structures and the abnormally reduced cord dimensions and cord signal are obvious on imaging. In CAAD, there may not be any direct dural or neural compression or deformation by the odontoid process. The clinical symptoms in patients having type 1 atlantoaxial instability are usually relatively acute and pronounced when compared to patients having CAAD where the symptoms are chronic, longstanding and subtle but progressively disabling in nature [3]. The clinical hallmark in patients with CAAD is the presence of a range of musculoskeletal and neural alterations [3-8]. Musculoskeletal alterations include basilar invagination and its various known accompaniments like short neck, short head, short spine, torticollis, kyphoscoliosis, platybasia, Klippel-Feil abnormality, assimilation of atlas, C2–3 fusion and bifid posterior arch of atlas [3-9]. Neural alterations include Chiari formation, syringomyelia, syringobulbia, external syringomyelia and external syringobulbia [3-9]. It was observed that each of these alterations when present singly or in association with other alterations can indicate the presence of CAAD. Our publications on the subject have identified that the entire range of musculoskeletal and neural alterations are not embryological disorders but are secondary natural processes that aim to protect the neural structures and life and delay or stall the neurological symptoms and deficits in the event of potential, subtle or manifest atlantoaxial instability, more often of central or axial variety [10,11]. Considering this fact, we prefer to label them as ‘alterations’ instead of ‘anomalies’ and ‘formations’ instead of ‘malformations’ [11]. The musculoskeletal and neural alterations attempt to make the spinal cord traverse a smaller and stretch free course and the fluid excess in the region float the cord away from the odontoid process and avoid compression [11]. The more important clinical issue is that all these musculoskeletal and neural alterations are potentially reversible following atlantoaxial stabilization as early as in the immediate postoperative phase.
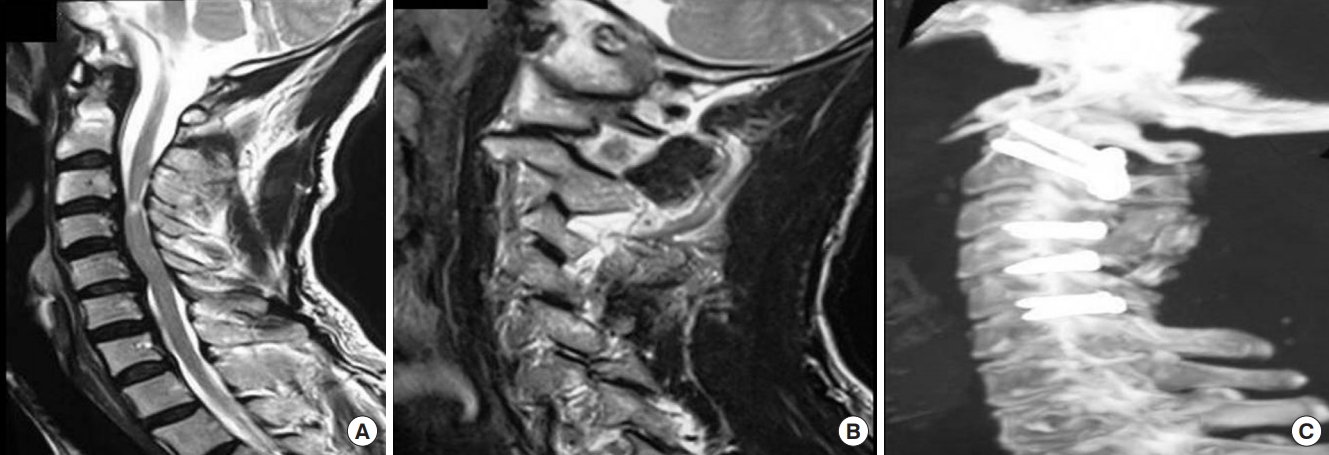
CHIARI FORMATION AND SYRINGOMYELIA
Embryological abnormality has been traditionally recognized to be the cause of Chiari formation and syringomyelia. The term ‘tonsillar herniation’ has been equated with the term ‘uncal herniation’ and consequently a sense of urgency in the management has prevailed. Morphometric assessments of the posterior cranial fossa have identified its reduced volume [12]. Foramen magnum decompression has been the gold-standard treatment for several decades. Many authors advocate the need for lysis of arachnoid bands and resection of the herniated tonsils. In 1998, we recommended that in cases with Chiari formation dural opening is not necessary during foramen magnum decompression [12]. In 2013, we reported that atlantoaxial instability is the nodal point of pathogenesis of Chiari formation and a host of other associated manifestations like basilar invagination and syringomyelia [4,5]. Clinical symptom of pain in the nape of neck seem to be more related to atlantoaxial instability than to alterations in the intracranial pressures as has been previously speculated [13]. Symptoms of sleep apnea, breathing disturbances, voice alterations and breathlessness on exertion were identified to be related to atlantoaxial instability [14]. On the basis of our analysis we advocated the efficacy of atlantoaxial fixation in resolution of the symptoms and reversal of tonsillar herniation and reduction in the size of syringomyelia [4]. We observed that majority of patients with Chiari formation and syringomyelia had CAAD (Figs. 3, 4). In cases having Chiari formation and syringomyelia atlantoaxial joint is difficult to expose due to presence of relatively higher volume of venous sinuses in the extradural spaces due to small volume of neural tissue in larger volume spinal canal [8]. Significant instability can be identified on manual manipulation of the bones of the region [15]. Successful and strong atlantoaxial fixation can result in intraoperative improvement in motor evoked potentials and immediate postoperative recovery in clinical symptoms [16]. The rapidity of improvement in symptoms is a clear testimony of presence of an unstable atlantoaxial joint. Understanding of the fact that CAAD is present in cases with Chiari formation has the potential of revolutionizing the treatment.
Images of a 35-year-old male patient. (A) T2-weighted magnetic resonance imaging (MRI) showing basilar invagination, Chiari formation and syringomyelia. (B) Computed tomography (CT) scan showing basilar invagination. (C) CT scan with the cut passing through the facets. The facets of atlas and axis are in alignment. (D) Postoperative CT scan. (E) Postoperative CT scan showing the implant in the lateral masses of atlas and axis. (F) Postoperative MRI showing reduction in the size of syrinx.
Treatment of idiopathic syringomyelia is not clearly identified in the literature. We observed that identification and treatment of CAAD could be a gratifying surgical exercise and provide an opportunity of functional and symptomatic neurological recovery for the patient [17]. This is particularly when all other forms of surgical treatment have been identified to have only ‘doubtful’ or ‘inconsistent’ clinical impact.
BASILAR INVAGINATION
In 1998, we divided basilar invagination into 2 types on the basis of absence (basilar invagination group (1) or presence (basilar invagination group (2) of Chiari formation [12]. The concept was that basilar invagination was associated with ‘fixed’ atlantoaxial instability. As the anomaly was considered to be ‘fixed’ the surgical treatment was identified to be decompression; anterior transoral route for group 1 and posterior foramen magnum decompression for group 2 basilar invagination [12]. In 2004, we identified that a group of patients having basilar invagination (group A) can be surgically reduced by distraction of the facets of atlas and axis and introduced the term craniovertebral junction realignment as a form of surgical treatment for such cases (Fig. 1) [18]. Group B basilar invagination cases were identified to be having ‘fixed’ atlantoaxial instability and posterior decompression was identified to be the treatment [18]. Our current understanding is that all patients with basilar invagination are unstable and need atlantoaxial stabilization as treatment [7,8,19]. CAAD is present in cases where the conventional and validated parameters of identification of atlantoaxial instability are absent [2]. Understanding of the fact that CAAD is present in such cases and atlantoaxial stabilization is the treatment can provide an opportunity to successfully treat these patients (Figs. 2, 3). We have identified that foramen decompression is of no clinical relevance in such cases [20].
MULTISEGMENTAL CERVICAL SPONDYLOTIC DISEASE
In 2010, we proposed that it was not age related reduction in the water content of the intervertebral disc that initiates the process of spinal degeneration, but it is facetal retrolisthesis related to weakness of the muscles that are responsible for lifelong standing human position related to their disuse, abuse or injury [21,22]. Instability of the spinal segment/segments is the primary event and all the other spinal alterations like osteophyte formation, ligamentum flavum buckling, disc space reduction and ultimate reduction of spinal canal and/or neural foraminal dimensions are secondary alterations [21,22]. We introduced the concept of facetal distraction using Goel facet spacer for the treatment of single or multiple level radiculopathy and myelopathy (both cervical and lumbar) without resorting to any kind of bone, soft tissue, osteophyte or disc resection. The technique resulted in ‘indirect’ neural decompression and ultimately led to spinal arthrodesis [23,24]. A single act of facetal distraction was identified to reverse all the known pathological features identified in cases with degenerative spine that includes unbuckling of the ligamentum flavum and other intervertebral ligaments, reduction in the size of osteophyte and disc bulge and increase in the size of disc space and spinal and neural canals [23,24]. The surgical results following such treatment that ultimately aims at arthrodesis of affected spinal segments have been identified to be remarkably gratifying.
As our understanding matured, we realized that instability of the spinal segment/s formed the primary issue and ‘only-stabilization’ or fixation of the affected segments as treatment. It was identified that no direct or indirect techniques of spinal decompression is necessary in such cases [25-27].
Traditionally, in spinal degeneration, cervical multisegmental affection or multisegmental spinal instability has seldom been associated with atlantoaxial joint instability. The surgical procedures that involve treatment of multisegmental spinal degeneration are limited to subaxial spine. Understanding of the fact that CAAD is a ‘frequent’ accompaniment of multisegmental spinal spondylotic disease can be crucial in initiating rational surgical treatment (Fig. 5) [28]. CAAD is more frequently present in cases with ‘high’ cervical spinal degeneration, ‘old’ age patients and patients presenting with significant neurological deficits [29]. Presence of retro-odontoid ‘pseudotumor’ that we have identified to be similar to subaxial osteophyte is an additional indicator of presence of CAAD [30]. Osteophytes in the vicinity of the atlantoaxial facets, along the odontoid tip and unusually or abnormally open atlantoaxial joints can be indicators of presence of an unstable atlantoaxial joint [29]. In such cases atlantoaxial stabilization should be included in the fixation construct along with the fixation of subaxial spinal segments.
Images of a 52-year-old male patient. (A) T2-weighted magnetic resonance imaging (MRI) showing multisegmental spinal degeneration with evidences of cord compression and cord signal alteration. There is no neural compression in the region of craniovertebral junction. (B) MRI cut through the facets of atlas and axis showing type 2 atlantoaxial facetal instability. (C) Postoperative X-ray showing multisegmental fixation that includes atlantoaxial joint fixation.
TORTICOLLIS, CERVICAL KYPHOSIS, AND DORSAL KYPHOSCOLIOSIS
Torticollis is a frequently encountered musculoskeletal alteration in cases with basilar invagination. Presence of short neck and torticollis are by themselves indicators of presence of atlantoaxial instability. More often instability in such cases is CAAD.
Presence of cervical kyphosis was frequently identified to be associated with CAAD. Multisegmental spinal stabilization that includes atlantoaxial stabilization can be a rational form of surgical treatment in such cases [31].
We recently identified that cases with dorsal kyphoscoliosis can be associated with CAAD. Presence of Chiari formation and syringomyelia in association with dorsal kyphoscoliosis is a definitive indicator of presence of CAAD and is suggestive of the need for atlantoaxial stabilization [9]. The patients usually present with symptoms related to difficulty in breathing and myelopathy. Both these symptoms have been related to compression of the lung and of the neural tissues by spinal cord deformation. We observed that atlantoaxial fixation in such cases is associated with recovery from all major symptoms that includes recovery from spinal deformity [9].
OSSIFICATION OF THE POSTERIOR LONGITUDINAL LIGAMENT
Ossification of the posterior longitudinal ligament (OPLL) related myelopathy is amongst the more difficult and potentially a dangerous surgical treatment. Essentially OPLL is considered to be associated with a ‘more than normally stable’ spine. The presence of extra intervertebral spinal bone is identified to be an additional or enhancing stabilizing factor. The surgical treatment has been focused on ‘decompressing’ the spinal cord either from anterior perspective by corpectomy or by posterior aspect by laminectomy or by laminoplasty. Apart from various other factors, the number of spinal segments involved determines the direction of surgical approach. The issue regarding instability of the spinal segments is usually considered as multisegmental spinal decompression has been identified to have destabilizing effects. In 2015 we identified that the pathogenesis of OPLL is similar to that of spinal degenerative spondylosis and instability is primary and nodal factor that initiates and propels the process of OPLL [32]. Accordingly, for the first time in the literature, we proposed that stabilization of the spinal segments is the treatment and decompression of spinal canal is not necessary [32]. We identified that CAAD is frequently associated with subaxial spinal instability in cases with OPLL [33]. Identification of CAAD and inclusion of the atlantoaxial joint in the multisegmental spinal fixation forms the basis of treatment in such cases [33]. We have achieved remarkable clinical improvement following such a form of surgical treatment in cases having ‘high’ or even ‘low’ cervical OPLL (Fig. 6) [32,33].

Images of a 53-year-old female patient. (A) T2-weighted magnetic resonance imaging (MRI) showing multilevel cervical cord compression by ossification of the posterior longitudinal ligament (OPLL). (B) Computed tomography (CT) scan showing OPLL. (C) CT scan image passing through the facets showing no facetal instability. (D) Plain X-ray showing multisegmental spinal fixation that includes atlantoaxial joint.
HIRAYAMA DISEASE
Treatment of patients with Hirayama’s disease continues to remain under discussion. Multiple forms of treatment protocols have been advocated that range from dural ‘tacking’ stitches, corpectomy and laminectomy. In 2017, we identified that Hirayama disease is related to multilevel cervical spinal instability that more often includes CAAD [34].
CAAD AS A DISCRETE CLINICAL ENTITY
CAAD can be an independent clinical entity and a cause of cervical myelopathy [3]. High degree of suspicion that is based on clinical findings and radiological observations can guide towards the correct diagnosis. Presence of unusual cervical lordotic curvature, bone fusions, bifid arch of atlas and other telltale evidences can guide the surgeon towards the diagnosis of CAAD. Identification and treatment of CAAD can lead to relief from disabling symptoms [3].
CONCLUSIONS
Understanding of entity of CAAD can have significant implications in the surgical treatment of a number of commonly encountered clinical issues.
Notes
The authors have nothing to disclose.
References
Appendices
EDITOR’S NOTE Creativity, Network, and Collective Intelligence
I am delighted to present Dr. Goel’s invited article, entitled “A Review of a New Clinical Entity of ‘Central Atlantoaxial Instability’: Expanding Horizons of Craniovertebral Junction Surgery.” [1] In this article, Dr. Goel summarizes his lifelong journey and success stories in craniovertebral junction (CVJ) surgery, and provides an overview of a new concept related to atlantoaxial instability.
In 1998, Dr. Goel developed a groundbreaking new principle in Chari malformation’s treatment by recommending that dural opening is not necessary during foramen magnum decompression. Dr. Goel’s most famous achievement in his life as a surgeon is probably the C1–2 arthrodesis technique. Dr. Goel developed the surgical principle of C1 lateral mass-C2 pedicle screw fixation (known as Goel’s technique or Goel-Harm’s technique) [2], as well as atlantoaxial joint distraction as a treatment for basilar invagination [3].
Like a river flows, the glory of success stories always passes. However, Dr. Goel did not rest on his laurels; instead, he embarked on another challenge related to the CVJ. Recently, he has strongly argued for the concept of central atlantoaxial instability as a way to understand the pathogenesis of various cervical spine diseases, including basilar invagination, Chiari malformation, cervical spondylotic myelopathy, and even ossification of the cervical posterior longitudinal ligament. His new concept is a very challenging, novel paradigm that is not explainable based on present-day concepts developed from evidence-based medicine. Furthermore, most of the evidence he proposed has not yet been proven or validated by other investigators. Therefore, Neurospine’s editors and reviewers presented extreme end-to-end opinions on Dr. Goel’s review article and did not reach agreement regarding its publication. As editor-in-chief of Neurospine, I decided to publish this article with an exemption from the peer-review process. Although Dr. Goel’s new concept has not been fully confirmed through scientific assessments by other peer researchers, this article is worth reading because he provokes our instinct of curiosity as Homo sapiens, allowing us to sample and catch a glimpse of the beautiful paradoxes and ambiguities of CVJ pathology.
In order to provide knowledge about evidence-based medical approaches to CVJ diseases, I invited the CVJ surgeon Dr. Behari (editor-in-chief of Neurology India, the official Journal of the Neurosurgical Societies of India) to write a manuscript on the development of indications and treatment strategies that are thoroughly grounded in the accumulated intellectual expertise from the history of medicine and scientific research on the CVJ. From Dr. Behari’s review article, entitled “Is Cervical Stabilization for All Cases of Chiari-I Malformation an Overkill? Evidence Speaks Louder Than Words!,” [4] we are excited to learn strategies for refining our knowledge and logical approach to treatment design based on well-designed medical research.
As editor-in-chief of Neurospine, I sincerely express gratitude to both Dr. Goel and Dr. Behari for providing outstanding intellectual input to Neurospine. I am also very appreciative of our editors who were willing to write editorials, which will help our readers to understand issues related to the CVJ and to reach appropriately-informed conclusions. I hope that our Neurospine readers will enjoy both articles and will achieve a deeper understanding of CVJ pathologies (from Dr. Goel’s article) and of ways to help our patients using evidence-based practice (Dr. Behari’s article) until Dr. Goel’s concept is proven by peers.
June 12, 2019
Yoon Ha
Editor-in-Chief of Neurospine
REFERENCES
1. Goel A. A review of a new clinical entity of ‘central atlantoaxial instability’: expanding horizons of craniovertebral junction surgery. Neurospine 2019;16:186-94.
2. Goel A, Laheri VK. Plate and screw fixation for atlanto-axial dislocation. Acta Neurochir (Wien) 1994;129:47-53.
3. Goel A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine 2004;1:281-6.
4. Deora H, Behari S, Sardhara J, Singh S, Srivastava AK. Is cervical stabilization for all cases of Chiari-I malformation an overkill? Evidence speaks louder than words! Neurospine 2019;16:195-206.
