Suture Repair in Endoscopic Surgery for Craniovertebral Junction
Article information
Abstract
Objective
Endoscopic approaches to the craniovertebral junction (CVJ) have been established as viable and effective surgical treatments in the past decade. One of the major complications is leakage of the cerebrospinal fluid (CSF). This study aimed to investigate the efficacy and feasibility of suture closure at the nasopharyngeal mucosa upon durotomy.
Methods
A series of consecutive patients who underwent different endoscopic approaches to the CVJ were retrospectively reviewed. The pathologies, surgical corridors, neurological and functional outcomes, radiological evaluations, and complications were analyzed. Different strategies of repair for the intraoperative CSF leakage were described and compared.
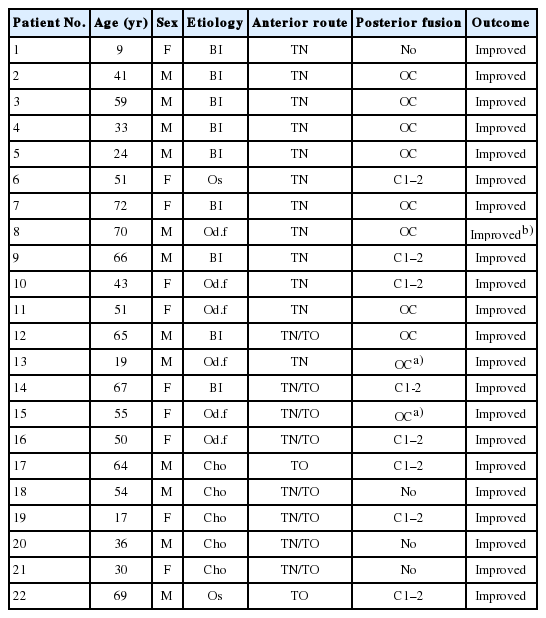
Results
A total of 22 patients covering 13 years were analyzed. There were 12, 2, and 8 patients who underwent transnasal, transoral, and combined approaches, respectively. There were 8 patients (36.4%) who experienced intraoperative CSF leakage, and were grouped into 2: 4 in the nonsuture (NS) group and 4 in the suture-repaired (SR) group. The NS group had 3 (75%) persistent CSF leakages postoperation that caused 1 mortality, whereas patients of the SR group had only 1 minor CSF rhinorrhea that healed spontaneously within days.
Conclusion
In this series of 22 patients who required anterior endoscopic resection of pathologies at the CVJ, there was 1 (4.5%) serious complication related to CSF leakage. For patients who had no durotomy, the mucosal incision at the nasopharynx usually healed rapidly and there were few procedure-related complications. For patients with intraoperative CSF leakage, suture closure was technically challenging but could significantly lower the risks of postoperative complications.
INTRODUCTION
Anterior surgical decompression at the craniovertebral junction (CVJ) is occasionally necessary for patients with pathologies of oncological, congenital, inflammatory or traumatic disorders. The most standard surgical corridor for the CVJ has long been the transoral approach [1-4]. In the last decade, there has been an emerging adaptation of endoscopic transnasal surgery for odontoidectomy or resection of tumors at the CVJ [5-8]. Although there have been no randomized control trials for comparison of the conventional microscopic approach to the innovative endoscopic approaches, the introduction of endoscopic approaches has been considered to mitigate the approach-related comorbidities [7-9].
For anomalies at the CVJ, there has been a trend toward less anterior decompression and more posterior reduction due to recent advances in technology and knowledge of the critical anatomical region [10-13]. Successful atlantoaxial (AA) fixation and realignment of the clivus and AA complex could substantially reduce the need for anterior decompression [14-17]. However, for selected patients, direct anterior decompression, including resection of a neoplasm, pannus, or bony deformity, is still a straightforward solution. To achieve adequate resection of the pathology at the CVJ, endoscopic transnasal or transoral surgery appears to provide a minimally invasive option. Although neurological complications associated with the endoscopic transnasal or transoral surgery are rare, the endoscopic approach is not free of risks. One of the most drastic complications of these endoscopic surgeries is cerebrospinal fluid (CSF) leakage, which could cause subsequent meningitis and mortality [6,18-20]. The CSF leakage after durotomy, no matter incidental or planned, could be more difficult to repair with endoscopes than that under microscopes. To date, there have been only a few reports that have addressed the repair of durotomy. Moreover, most of the repair techniques described were for the expanded endonasal approach and involved the use of a nasal-septal flap [21-23]. For endoscopic surgery at the CVJ, the suture repair technique was seldom addressed [5].
This paper summarizes the authors’ serial experiences of endoscopic (e.g., transnasal, transoral, or combined) surgery at the CVJ, with emphasis on the technical aspect of repair for CSF leakage. The study aimed to shed light on the advantages of suture closure.
MATERIALS AND METHODS
From July 2004 to November 2017, consecutive patients who underwent endoscopic transnasal, transoral, or combined approaches for resection of pathologies at the CVJ at the authors’ institute were included for analysis. In this retrospective study, we reviewed all the clinical and radiological data of every patient. The underlying pathologies of the CVJ included basilar invagination, Os odontoideum, nonunion of old odontoid fracture, chronic inflammation with pannus formation associated with rheumatic disorders, severe deformity with AA dislocation, and neoplasms, such as clival chordoma. All patients received the standard endoscopic transnasal, transoral, or combined approaches for anterior odontoidectomies (Table 1), according to the senior authors’ (Yen or Wu) decision. The surgical indication was progressive quadriparesis or myelopathy caused by ventral neural compression at the CVJ.
1. Perioperative Management and Operative Techniques
All patients were subject to halo-vest immobilization after traction in the intensive care unit before surgery to achieve better alignment of the CVJ. Intraoperative fluoroscopy and the neuronavigation system (VectorVision Cranial; BrainLab, Munich, Germany; Stealth 7, Medtronic, Minneapolis, MN, United States) were used for confirmation of anatomical landmarks during surgery. The surgery of endoscopic transnasal odontoidectomy was performed on the first 2 patients with a singlenostril approach. The other patients received modified endoscopic transnasal or transoral odontoidectomy via 2 nostrils without entering the sphenoid sinus, which was described in the authors’ previous reports [6].
A linear vertical incision at the nasopharyngeal mucosa wall was made to perform the surgery in every patient. The surgical field of the transnasal approach was very small and limited, so that suture closure was attempted in only 3 patients, but was not achievable. Later in the series the authors shifted the suture procedure to the transoral corridor, which allowed a wider working space, even though sometimes the main part of the surgery (i.e., decompression or resection of the tumor) was performed via the transnasal corridor. Also, an autologous fat graft, harvested from the abdominal wall subcutaneously was subsequently placed into the linear mucosal defect to mitigate the chances of postoperative CSF leakage. In those patients of the SR group, long needle forceps were used for suture with 3-0 polysorbs or 4-0 chromic catgut. The knots were tightened with a pusher used in endoscopic surgery (Fig. 1; Supplementary video clips 1, 2). After the anterior operation, the patient was sent to the intensive care unit for observation. Subsequently, lateral radiographs and computed tomography (CT) scans were always obtained for confirmation of the degree of decompression and stability. Most of the patients in the series later (usually within days) underwent posterior fixation surgery for assurance of stability and improvement of reduction [17]. Immediately after posterior fixation surgery, the halo-vest was removed in the operation room and switched to a Miami-J neck collar for postoperative support, unless it was otherwise contraindicated.

Illustration of the sequential steps involved in mucosal suture repair. (A) After retracting the oral cavity, a needle was placed using the holder with 3-0 Polysorb to suture the mucosal insicion. (B) A pusher was used for tightening the tie after stitch. (C) The knot on the tie was pushed down. (D) Transoral mucosal suture was done after the stitches were made.
Due to the retrospective nature of the analysis, the study was exempted for approval by the institutional review board. There were only review of the medical charts and radiological evaluations, without any additional examinations or interventions of the patients throughout the study period. Therefore, there was no need for informed consents from the patients included.
2. Follow-up Evaluations
Standard anteroposterior, lateral radiographs were obtained before the anterior surgery, after the anterior surgery, after the posterior fixation surgery, and at approximately 3-, 6-, 12-, and 24-month follow-up. Thin-section axial and sagittal reformatted CT scans of the CVJ were obtained before and after the anterior surgery, after the posterior fixation surgery to check screw positions, and approximately 12 months after surgery. Also, magnetic resonances images (MRIs) were obtained before and approximately 6 months after the operations. Preoperative, perioperative, and postoperative assessment and findings were recorded by the treating neurosurgeons of the patients, with the assistance of specialized nurse practitioners.
The outcomes of each surgical approach (i.e., transnasal, transoral, or combined both transnasal and transoral) were compared. Those patients who had mucosal suture closure were also compared to those had not (i.e., repaired mainly with grafting and glue). All the morbidities and mortalities were compared during the follow-up period. All continuous and categorical parameters in each follow-up point were analyzed by the method of t-test and chi-square test. The significance of statistic results was defined by p-valve less than 0.05.
RESULTS
A total of 22 patients were included in this retrospective analysis. There were 16 patients who received 2-phase surgical management, which included an anterior odontoidectomy and a staged posterior fixation within days after the first-stage surgery. There were 2 patients who had odontoid fractures and had already received posterior fixation surgery and presented with progressive deformity in addition to severe ventral spinal cord compression. Thus, these 2 received only anterior odontoidectomy. There was 1 patient who received only anterior surgery due to their young age and there was no obvious instability according to postoperative radiography and CT scans. There were 3 patients in whom surgery was indicated due to clival chordoma, and they all received only anterior tumor decompression but no posterior fixation (Table 1).
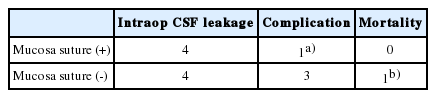
The patients were categorized for comparison of clinical outcomes, based on whether or not the transoral suture repair of the mucosa after anterior decompression operation was performed. Thus, the 22 patients were divided by the surgical corridor used, including the transnasal, transoral, and combined (Table 2). One of the 12 patients who underwent surgery via transnasal approach received mucosa suture and all of the 2 patients with transoral approach received transoral mucosal suture for repair the vertical incision. In the group of combined transnasal and transoral approach, 7 out of 8 patients received mucosa suture for repair. Furthermore, there were 8 patients (36.4%) who experienced intraoperative CSF leakage, and were grouped into two: 4 in the nonsuture (NS) and 4 in the suture-repaired (SR) groups. The NS group had 3 (75%) persistent CSF leakages postoperation, that caused one mortality, whereas patients of the SR group had only 1 minor CSF rhinorrhea that healed spontaneously within days (Table 3). However, after analyzing by t-test and chi-square test, there is no statistical significance between these 2 groups. Uncomplicated patients of the series required no prolonged intubation nor feeding tubes, and all had neurological improvement.
The transnasal approach group consisted of 12 patients, 4 of whom had intraoperative CSF leakage. Postoperative meningitis was noted in 3 patients and all of them were found to have intraoperative CSF leakage without transoral suture. In this group, all patients showed neurological improvement after the surgery, but 1 patient died 10 days after the surgery due to severe sepsis and multiple organ failure. There were 2 patients of the transoral approach group, and both received transoral mucosal sutures without postoperative complications. The combined approach (both transnasal and transoral) group consisted of 8 patients, 3 of whom recorded intraoperative CSF leakage. However, there was only 1 patient for whom CSF rhinorrhea was noted without culture data for confirmation. For those patients in whom we found intraoperative CSF leakage, we compared the complication rates between SR patients and NS patients. But there was also no statistical significance due to small sample size. All patients unanimously had fat grafts for obliteration of the empty space and used tissue glue for temporary fixation and strengthening.
In this retrospective study, there were no patients in this series who required reoperation for postoperative hematoma or wound infection. No permanent feeding tube nor newly required mechanical ventilator were needed after the surgery, except 1 patient with a pre-existing mechanical ventilator dependence.
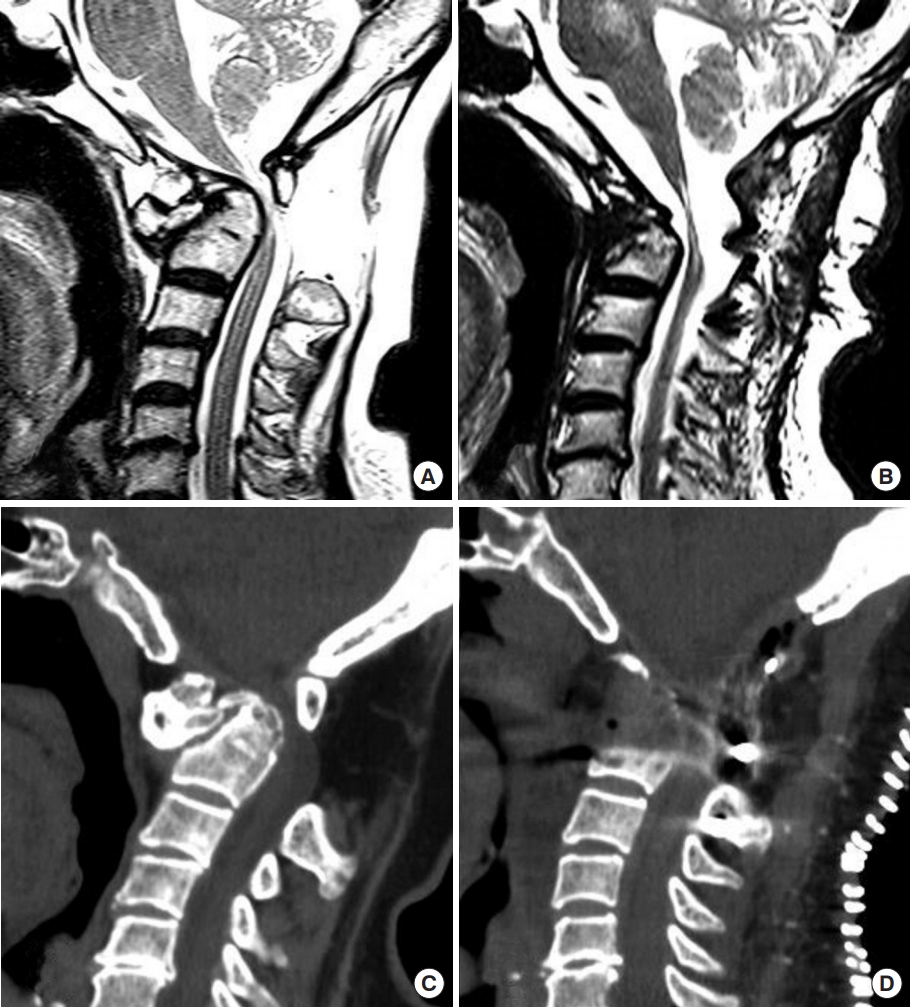
1. Case 1
A 66-year-old woman who suffered from nuchal pain and tightness for years and which gradually progressed to the lower limbs with weakness and claudication. The patient received cervical spine MRI and CT scans which reported an old fracture of the odontoid process with AA subluxation resulting in severe central canal spinal stenosis (Fig. 2A, C). The transnasal approach for odontoidectomy was performed and an intraoperative dura tear with CSF leakage was noted. Due to the small and limited surgical field, a transnasal suture was too difficult to perform. Thus, autologous fat graft harvested from the abdominal wall was subsequently placed into the linear mucosal defect to prevent postoperative CSF leakage. A posterior approach for C1–2 fusion with transarticular screws was performed 1 week after the initial surgery. Suboccipital craniectomy and C1 laminectomy were also done for better decompression. However, fever and leukocytosis with an elevated C-reactive protein level were noted and antibiotics were then prescribed. Postoperative dysphagia was also noted and gradually improved after rehabilitation. Cervical MRI and CT scans also followed postoperatively and revealed good decompression of cord compression (Fig. 2B, D). The patient was then discharged and regularly followed- up at the out-patient department.
2. Case 2
A 64-year-old male diagnosed as having cervical chordoma presented with progressive numbness and weakness of the upper limbs to the lower limbs, and an unsteady gait had also been noted for 3 months. Cervical MRI and CT scans were performed and revealed a lobulated soft tissue mass lesion at the prevertebral space with C2 vertebral body involvement and epidural extension with mild extradural compression of the spinal cord (Fig. 3A, C). Thus, a transoral approach for tumor removal was performed with tumor forceps and bipolar cauterization. After tumor removal, a transoral suture was done with 3-0 polysorbs and 4-0 chromic catgut. There was no intraoperative nor postoperative CSF leakage. The patient received posterior cervical surgery with C1–4 fusion for stability and C1–2 laminectomy for decompression almost 1 month after the initial surgery. After the surgery, the patient recovered well and was discharged 1 week later. There were significant improvements in quadriparesis, numbness and unsteadiness postoperation. The postoperative follow-up MRI and CT scans demonstrated the anterosuperior part of the tumor at the retropharyngeal prevertebral space was removed (Fig. 3B, D). Subsequently the patient received proton beam radiation for unresectable part of the tumor and remained stable at 2-year follow-ups.
DISCUSSION
In this study, we focused on the clinical complications of those patients with endoscopic resection at the CVJ who received transoral suture or not. Transoral or transnasal odontoid resection is a direct surgical technique for ventral compression of the spinal cord in cases of nonreducible subluxation following odontoid fractures, and odontoid pathologies such as odontoid neoplasm and infections. The most commonly reported complications following the endoscopic transnasal approach were intraoperative and postoperative CSF leaks. Higher rates of CSF leaks following a transnasal approach were reported than for the transoral approach. It was reported that four patients had an intraoperative CSF leak, but none of them were found to have a postoperative CSF leak [24]. Autologous fat graft and tissue glue to repair and resolve the problems of intraoperative CSF leak were used [25]. In our study, 8 out of 21 patients (38.1%) were found to have intraoperative CSF leaks; 1 patient (4%) developed postoperative CSF rhinorrhea, and 3 patients (14%) were found to have postoperative meningitis and were treated with antibiotics. We also used autologous fat graft and fibrin glue for repair. Among the 9 patients for whom the transoral approach was used, a simple mucosa suture was performed with catgut stitches, which effectively decreased the postoperative CSF leakage rate to almost 50%. Damage to the dura causing following CSF leakage emphasized the importance of intraoperative repair with simple suture to avoid infection. Compared to the transnasal group, medical complications were much higher in the transoral group. Choi et al. [26] reported 17 patients (4%) who developed cardiovascular complications and 53 patients (12%) who suffered from respiratory complications among 428 patients. Marda et al. [27] described 28 of 178 patients (15.7%) who developed medical complications. Other studies showed a lower rate of medical complications compared to the above 2 studies. In our study, 1 patient (4%) showed neurological improvement, but died 10 days after the surgery due to severe sepsis and multiple organ failure. No patients in this study required reoperation for postoperative hematoma or wound infection. No permanent feeding tube nor mechanical ventilator were needed after the surgery, except 1 patient with a pre-existing mechanical ventilator dependence.
The clinical outcome of neurological improvement was 100% in our study. All patients improved after endoscopic anterior decompression at the CVJ. The rate of improved outcomes differed slightly between the transnasal and transoral groups. One patient underwent the transnasal approach without suture, causing meningitis and severe sepsis. There was no report of a worsening postoperative neurological condition among the transoral approach with the suture group. However, the outcomes and complications of the transoral approach mainly depend on the surgical skills of the neurosurgeon. Postoperative neurological deterioration was described in only 2 cases. Laborde et al. [28] reported 2 patients who underwent transoral decompression and who suffered from immediate neurological deterioration postoperatively due to no stabilization right after the decompression surgery. These patients’ neurological status improved after the application of a halo-vest and subsequent posterior fusion surgery. These cases of neurological deterioration after anterior decompression highlight the need for adequate decompression and immediate stabilization.
Odontoidectomy has been a widely accepted surgical procedure to decompress the soft tissue and osseous mass lesions at the anterior CVJ. There have been a number of series published in the past two decades showing satisfactory clinical results of this transoral approach [29-32]. Detailed surgical techniques and nuances of transoral surgery have been described in detail in the literature by multiple authors [3,29-31,33,34]. In addition, other approaches to anterior or lateral CVJ with wider exposures, which often involve more aggressive osteotomies along the surgical corridor, have been reported. For example, such extensive surgical approaches include palate splitting, mandibulotomy, or trespassing the maxillary sinus, and even a zygomatic process or other extensive craniotomies. Under microscopes or loupe with head lights, these extensive approaches allow magnification and illumination of the deeply seated anterior CVJ and surgical maneuver of the neural tissue. However, since these microscopic approaches require wide exposures, they inevitably carry problems of reconstruction, including both cosmetic and functional.
Endoscopic approaches have emerged and prevailed in the past decade for many skull-based cases [5-7,9]. Using the endoscope, magnification and illumination can be achieved easily. Moreover, the endoscope provides a remarkably more panoramic view of the deeply seated CVJ than microscopes. Around the CVJ, which usually requires a working corridor of 8 to 10 centimeters long, the viewing angle and working space is inherently limited through the microscopes. In contrast, the endoscope can move the surgeons’ eyes closer to the target of pathology and thus gain a greater panoramic view of surrounding structures. Moreover, by introducing the endoscope at an angled-view (e.g., the 30°, 45°, and 70° angled endoscopes), significantly greater and wider visualization can be achieved. Surgical manipulation of the structures seen under the endoscope also often requires specialized instruments, which have bayonet-shaped long shafts, or mechanisms that could convert the direction of force. The endoscopic approaches to the anterior CVJ are less invasive than traditional microscopic surgery because they require less exposure and thus less compromise to the normal anatomical structures and physiological functions. For example, an endoscopic transnasal transclival odontoidectomy can achieve similar decompression at the anterior CVJ while allowing less velopharyngeal insufficiency and earlier oral intake than the traditional transoral odontoidectomy performed with microscopes [5-7].
There are still several limitations for transoral and transnasal approaches, such as the limited surgical field and space, the lesion should be as midline as possible, the surgical learning curve of the endoscopic approach is steep, and the difficulty of mucosa suture. Although complication rates showed to be higher in the group without mucosal suture, there was no statistically significance between the suture group and nonsuture groups of all kind of approaches (transnasal approach, transoral approach, combined approach). The small sample size could also influence the statistical significance of complication rates. Besides, there were different pathologies and diagnoses among the cases, and our study had no control group. We focused our study to investigate the influence between transoral suture or not and the surgical complications.
CONCLUSION
In this series of 22 patients who required anterior endoscopic resection of pathologies at the CVJ, there was 1 (4.5%) serious complication related to CSF leakage. For patients who had no durotomy, the mucosal incision at the nasopharynx usually healed rapidly and there were few procedure-related complications. For patients with intraoperative CSF leakage, suture closure was technically challenging but could significantly lower the risks of postoperative complications.
Notes
The authors have nothing to disclose.
SUPPLEMENTARY MATERIALS
Supplementary video clip 1 and 2 can be found via https://doi.org/10.14245/ns.1938174.087.v1, https://doi.org/10.14245/ns.1938174.087.v2.
Supplementary video clip 1: The video clip illustrates the surgical steps for the patient of C1–2 subluxation and received transnasal odontoidectomy and transoral mucosal suture. After impaction of a piece of gelfoam and fat graft, sutured with 3-0 polysorb were done via transoral approach. (https://youtu.be/Q20EMvc-sFk).
Supplementary video clip 2: The suture video of a case of clival chordoma with a large dura defect after removal of tumor. After impaction with a fat graft, 2 stitches of suture with 3-0 polysorb were performed from oral cavity to secure the fat graft. During suture procedure, 30° endoscope was used, and the soft palate and uvula were retracted upward for exposure of nasopharyngeal incision (https://youtu.be/lou_yNPxsQw).