Towards Guideline-Based Management of Tethered Cord Syndrome in Spina Bifida: A Global Health Paradigm Shift in the Era of Prenatal Surgery
Article information
Abstract
An estimated 60% of the world’s population lives in Asia, where the incidence of neural tube defects is high. Aware that tethered cord syndrome (TCS) is an important comorbidity, the purpose of this systematic review was to explore the treatment of TCS among individuals living with spina bifida (SB) in Asia. MEDLINE and Embase databases were searched for relevant studies published from January 2000 to June 2018. Search terms such as ‘spinal dysraphism,’ ‘spinabifida,’ ‘diastematomyelia,’ ‘lipomeningocele,’ ‘lypomyelomeningocele,’ ‘meningomyelocele,’ and ‘tethered cord syndrome’ were used in diverse combinations. Of the 1,290 articles that were identified in accordance with PRISMA (Preferred Items for Systematic Reviews and Meta-Analyses) guidelines, 15 Asia-based studies met the inclusion criteria. Significant differences in the diagnostic criteria and management of TCS were documented. As the surgical techniques for prenatal closure of the spinal defect continue to evolve, their adoption internationally is likely to continue. In this setting, a clear and evidence-based approach to the definition and management of TCS is essential. The recent publication by the Spina Bifida Association of America of their updated care guidelines may serve as a tool used to promote a systematized approach to diagnosing and treating TCS among individuals with SB in the region, as well as globally.
INTRODUCTION
An estimated 60% of the world’s population lives in Asia [1]. As with many other parts of the globe, disparities in medical care exist among countries in this region. The Lancet Commission on Global Surgery reports that more than 70% of the world’s population does not have access to timely, safe, or affordable surgical care. Access to proper surgical care is even less prevalent in South Asia, where up to 97% of the population lives without access to surgical care; this is in sharp contrast to the reality lived among higher-income regions, where only 3.6% of the population has a similar experience [2]. Additionally, although mandatory folic acid fortification has resulted in a lower prevalence of neural tube defects (NTDs) worldwide, rates of new folic acid preventable NTD cases remain calcitrant to reduction, and divergent prevalence rates exist within nations [3]. In Asia specifically, mandatory legislation enforcing fortification has lagged behind the evidence supporting it [4]. Given the size of the population across Asia and the presence of this surgical disparity, attention as to how to best allocate resources and provide greater access to avant-garde surgical techniques is mounting within the global health field.
Worldwide NTDs, comprising anencephaly and spinal dysraphism, are estimated to occur in 15–23 per 10,000 live births, with a higher prevalence reported in Southern Asia, at an estimated 22–43 per 10,000 live births [5]. The most common form of spinal dysraphism occurs along the dorsal spine, referred to as open spina bifida (SB). Myelomeningocele (MMC), the most common form of open SB, has long been associated with several comorbidities such as hydrocephalus, Chiari II malformation, tethered cord, scoliotic and kyphotic spinal deformities, skin injuries, as well as, neurogenic bowel and bladder [6,7]. Additionally, correction of a complex spinal deformities can produce severe pressure wound complications during treatment, after spinal instrumentation, or ambulation [8]. Differences in the related health outcomes vary widely contingent upon access to medical care, financial resources, and cultural/educational barriers that are specific to each region. Given the significant phenotypic variation in NTDs, the critical need for research-driven approach to this condition, as well as the multidisciplinary perspectives in its management, have long been recognized [9,10]. In response, the Spina Bifida Association of America (SBA) has developed evidence-based guidelines for the provision of care to individuals living with SB. Concurrently, global prevention efforts to reduce congenital disability have focused on the nutritional fortification of grains with folic acid and its prophylactic use by women in the childbearing years [11-13]. However, care is still needed to address the many related comorbidities and improve the quality of life among those living with NTDs. This is centered on the provision of appropriate medical and surgical services. Historically, surgical interventions have primarily focused on comorbidity mitigation. However, in the recent past, closure of the spinal defect prenatally has given rise to the possibility of preventing further damage secondary to ongoing exposure of the neural elements to amniotic fluid. These prenatal interventions have evolved over time from an open access hysterotomy approach to endoscopic coverage of the spinal defect [14-16]. Moreover, during the 2nd Asia Pacific Conference on Fetal Therapy in Singapore, a round table discussion was held to create a candidate model which can be applied in Asia to offer fetal surgery for MMC [17].
Presenting with 2 etiologies, tethered cord syndrome (TCS) is a common SB comorbidity, present as part of the congenital syndrome (primary) or as secondary to the open MMC closure, which has an incidence of 14%–32% [18-21]. When individuals with NTDs begin to display early symptoms of neurological deterioration such as impaired motor function, lumbosciatica, scoliotic and kyphotic spinal deformities, bowel/bladder incontinence, or foot deformities, then surgical untethering is paramount. The untethering procedure leads to an improvement of neurological function in an estimated 42%–75% of individuals with TCS [19,22,23]. However, it should be noted that the benefit of surgical intervention is most optimal among symptomatic individuals, versus those who have asymptomatic tethering [24]. In an era of expanding global surgical care [25], a common understanding of the clinical indications, time of intervention, and surgical technique in the management of TCS is fundamental. However, as with the surgical technique for endoscopic closure of the spinal defect, the definition of TCS as a condition that merits surgical intervention has also evolved over time. Another literature review defined TCS as “a diverse clinical entity characterized by symptoms and signs which are caused by excessive tension on the spinal cord” [26]. For this review, the same definition was used. We hypothesized that there would be variation in the approach to TCS throughout Asia. Therefore, the purpose of this systematic review was to explore the treatment of TCS among individuals living with SB in Asia.
METHODS
This review was conducted and reported in line with the Preferred Items for Systematic Reviews and Meta-Analyses (PRISMA) [27]. The MEDLINE, PubMed, and Embase databases were searched for English language studies published from January 2000 to July 2018. A maximally expanded search was applied using the following terms ‘spinal dysraphism,’ ‘spina bifida,’ ‘diastematomyelia,’ ‘lipomeningocele,’ ‘lypomyelomeningocele,’ ‘meningomyelocele,’ and ‘tethered cord syndrome’ in diverse combination following search strategy described by McKibbon et al. [28] The inclusion criteria were: (1) children and adolescents (0–18 years old) with NTDs and TCS, (2) quantitative studies, and (3) Asian region-based studies as defined by the United Nations [29]. Reviews, animal studies, case reports, conference abstracts, editorials, and comments were excluded. Studies that included less than 6 individuals with NTDs as a subset of a population were also excluded. Also we included a search of the gray literature (Google Scholar), personal communications, as well as a hand search of high-impact journals in the field using the reference lists of identified articles. Title and abstracts were screened before analyzing the full texts to determine their eligibility. Two reviewers independently assessed relevant studies to be included based on eligibility criteria. Any disagreements were resolved by discussion with a third reviewer. Methods of the analysis and inclusion criteria were specified in advance and documented in a protocol; the review protocol is available upon request.
Tethered cord and NTD-related information were extracted by one trained researcher using a standardized extraction form and checked by a second trained researcher. Data were obtained for the following study variables: authors, publication date, geographic location, experimental design, level of evidence, sample size, patients’ diagnoses, patients’ age, time of surgical intervention, duration of follow-up, and health outcomes related to the surgical intervention.
RESULTS
The systematic review was conducted on June 11, 2018. One thousand two hundred eighty-eight articles were identified in accordance with PRISMA guidelines, of which 15 Asia-based studies met the inclusion criteria for the systematic review (Fig. 1). Study characteristics and results of individual studies are presented in Table 1.

PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram of the search strategy and selection criteria. Adapted from Moher et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. https://doi.org/10.1371/journal.pmed1000097 [27].
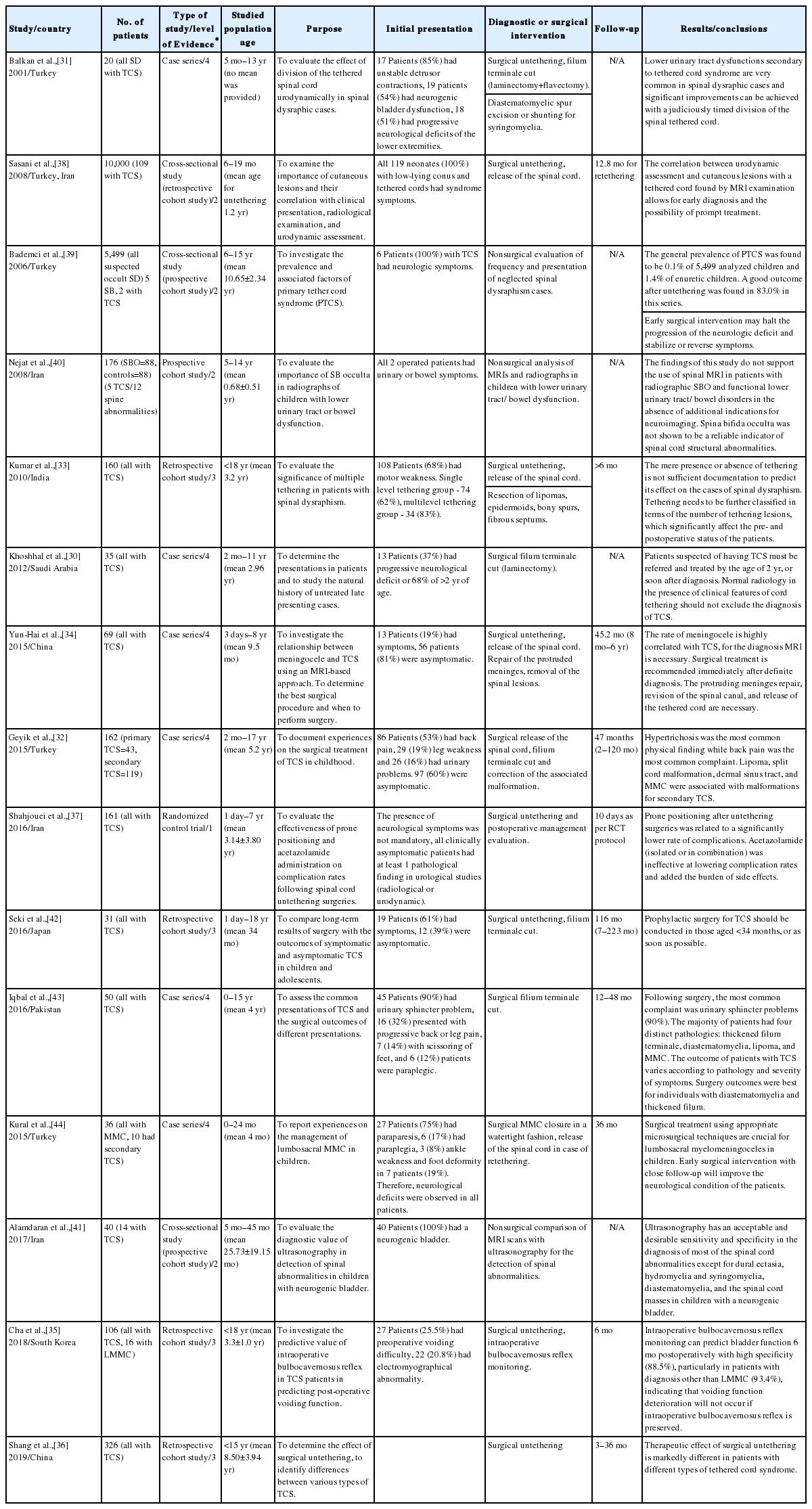
Literature review of the management of tethered cord syndrome (TCS) among individuals living with spina bifida in Asia
1. Study Characteristics
Studies meeting inclusion criteria were published from Turkey (4), Iran (3), China (2), South Korea (1), Japan (1), India (1), Pakistan (1), Saudi Arabia (1), as well as, Turkey and Iran (1) as a collaborative study. The most frequent study designs were case series (6 of 15 studies) and cross-sectional studies (3 of 15 studies). Seven of the 15 studies had less than 50 participants with TCS in their cohort. The spectrum of articles was representative of children of various ages: 3 studies had an average age for their participants above 1 year, and 8 studies had age ranges between 2 and 5 years.
2. Initial Clinical Presentation and Research Focus
The primary focus for the included studies was an analysis of surgical results and complications (n= 7), description of epidemiology, and initial clinical TCS presentation (n= 3), as well as development and comparison of diagnostics (n= 3). There was wide variability in the description of neurological status and also a divergence in the reasoning for conducting untethering surgery in asymptomatic cases. For example, Khoshhal et al. [30] reported progressive neurologic deficit in only 13/35 (37%) of cases, while Balkan et al. [31] reported that 18 of 20 of individuals (90%) had progressive neurologic deficit before surgery. Geyik et al. [32] reported that 97 of 161 of the cases (60%) were asymptomatic, and Kumar et al. [33] reported that 108/160 (68%) of individuals did not have motor weakness. Moreover, 56 of 69 (81%) were asymptomatic in the study by Yun-Hai et al. [34] Cha et al. [35] used intraoperative neurophysiological monitoring to predict bladder function after surgical untethering. However only 27 individuals (25.5%) had preoperative voiding difficulties, and 22 (20.8%) had electromyographical abnormalities. Shang et al. [36] had at least 38 individuals (11.6%) with no neurological deficit. The presence of neurologic symptoms was not a prerequisite for untethering in the study by Shahjouei et al. [37] Lastly, only 3 studies used urodynamic testing as part of their patients’ examination [31,35,38].
3. Description of Evaluation, Results, and Follow-up
Three studies did not include surgical treatment but focused on nonsurgical evaluation and analysis of individuals with TCS [39-41]. Among surgical studies (n= 12), there was no clear or standardized description in the untethering technique utilized [30-34,37,38,42-44]. Among these surgical studies, only 6 described their complications in the results section of the respective article. Additionally, 5 out of the 13 studies did not provide information on the length of follow-up after surgical intervention. Concerning the potential source of bias, the most frequent risk for bias was the lack of clear diagnostic criteria, variability in study design, as well as the lack of homogeneity in sample sizes, indications for interventions, and outcome measures.
DISCUSSION
1. Global Surgery and Variance in Surgical Approach to TCS
This literature review is the first to summarize published studies from Asia relating to surgical management of TCS among individuals with NTDs. In our systematic review, we observed differences in the diagnostic criteria of TCS and widely variable health outcomes following surgery in Asian countries [31,38-40]. Our findings suggest that among studies conducted in this region, the management of TCS was aggressive in the surgical approach leading to untethering and often did not rely on the presence of progressive neurologic deficits as a criterion for initial surgical treatment of spinal cord tethering [30,33,34,42].
To address the observable variation in the diagnostic criteria for TCS, Lew and Kothbauer [26] defined TCS as “a diverse clinical entity which presents with symptoms and signs resulting from abnormal spinal cord tension.” They advocated that surgical untethering was only necessary in cases with progressive or new-onset symptomatology attributable to TCS and raised questions regarding the benefits of surgical untethering among asymptomatic individuals. Furthermore, Yamada and Won [45] proposed that the terms “tethered cord syndrome” and “tethered spinal cord” be used exclusively to describe the presence of a functional disorder. Based on these parameters, individuals described as having TCS should exhibit symptoms attributable to a tethered cord.
To detect symptoms related to spinal cord tethering, noninvasive imaging techniques have been employed. Dias [46] has demonstrated that magnetic resonance images (MRIs) of the spine exhibit signs of tethering in most individuals with MMC. However, clinically significant symptoms are only present in about 30% of these cases. Additionally, Bowman et al. [21] reported that all children born with MMC have a low-lying cord when examined on MRI, even after initial repair and untethering. These findings are consistent with tethering and scarring resulting from prior MMC closure. However, less than one-third of these children will ever display signs of neurological, orthopedic, or urological impairment, despite the probability of being anatomically tethered.
2. Potential Increase Risk of TCS Following Prenatal Repair of the Spinal Defect
As the surgical technique of prenatal MMC closure continues to evolve, its adoption in different regions of the world will continue to increase [17]. However, a trend towards an increased rate of secondary tethering following the use of this new prenatal approach has been documented [47,48]. Danzer et al. [49] reported that 14 out of 42 children (33%) developed spinal cord tethering, despite the prenatal surgical repair. This issue requires particular attention as children undergoing prenatal closure of the spinal defect may not receive longitudinal follow-up if the fragmentation of care is not explicitly addressed after fetal surgery, or as they transition from pediatric-centered to adult-centered healthcare. Chiefly as The Singapore Consensus demonstrates [17], centers across Asia are adopting emerging fetal surgical management techniques; therefore the potential risk for observing an increase in the incidence of TCS is ongoing. Therefore, a clear and evidence-based approach to the definition and management of TCS is crucial to provide the best quality of care possible across the globe.
3. Diagnostic and Surgical Interventions for TCS
In the United States (US), Yamada and Won [45] has defined TCS as a “stretch-induced functional disorder of the spinal cord” and has recommended close observation for asymptomatic individuals instead of surgical intervention as a primary approach. In our review, 3 out of the 15 included studies focused on diagnostic interventions for TCS [39-41]. For instance, Alamdaran et al. [41] compared the efficacy of MRI scans to ultrasonography for the detection of spinal abnormalities. Although ultrasound has a much lower resolution quality than MRI, it was described as a useful screening tool for TCS with best results under a 2 months of age window [50,51]. However, it is important to note that the average age in the study by Alamdaran et al. [41] was more than 2 years of age, which may have influenced their published results.
There were 12 studies that focused on surgical management, of which only 4 described their complications [32,37,38,44]. Overall, the mortality rate after spinal cord untethering was relatively low and usually resulted from infectious complications such as meningitis [52]. Given the morbidities (e.g., infectious complications, pseudomeningocele) affecting 10%–35% of cases [53-57], it should be noted that individuals with MMC are at an even higher risk than those with occult spinal dysraphism due to increased incidence of multiple recurrences, scarring, and poorly vascularized covering tissues. In light of our findings and the growing body of evidence in other regions of the globe, prophylactic surgical intervention among asymptomatic cases in Asia is called into question [58].
4. Refinement of the TCS Evaluation and Management Process
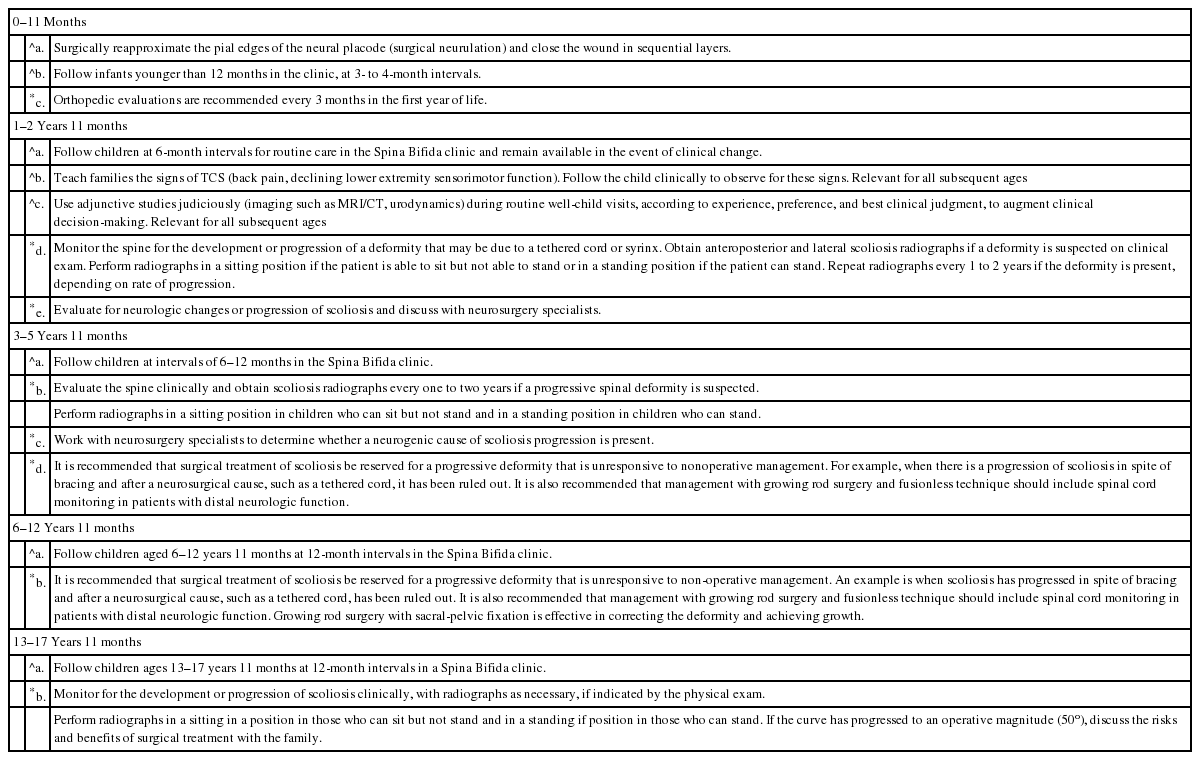
Currently, prophylactic untethering in asymptomatic individuals is not widely practiced in the US, as there are no controlled, prospective studies that have shown the benefits of the intervention in light of a high incidence of recurrent tethering [59]. In our review, we did not find a consistent evidence-based standard approach applied throughout the treatment centers. In most instances, the authors seemed to rely on anecdotal experience or previously established institutional practice. Concurrently, Buekens et al. [60] argue for a move to international collaboration to catalyze the use of tested interventions upfield. Buekens and colleagues argue that evidence-based global health necessitates the implementation of scientifically sound methods as the basis to interventions as they are adopted internationally. On October 25th 2018, the SBA released its updated “Guidelines for the Care of People with Spina Bifida” (available from: https://www.spinabifidaassociation.org/resource/guidelines/). The guidelines provide expert consensus and evidence-based guidance to the management of individuals living with SB; a summary of the TCS recommended approach is outlined in Table 2. Centers desiring to utilize an evidence-based approach to TCS management can implement these published recommendations ushering in the international opportunity for a cohesive approach to the diagnosis and management of TCS.
5. Advantage of Use of Evidence-Based Medicine in TCS
Evidence-based medicine refers to a set of practice standards that are based on scientific evidence, clinical expertise, and individual patient needs [61]. The development and later use of evidence-based medicine has improved clinical healthcare [62] and significantly influenced the comparative effectiveness of research [63], decreased over or under diagnoses and treatment [64], enhanced measures of quality of care [65], improved publishing standards [66], ensured that trials are registered [67], and curtailed the use of misguided interventions that have previously become part of established practice [68].
The research-based evidence and consensus of neurosurgeons who contributed to the aforementioned guidelines frame a standardized approach to individuals with NTDs and TCS. The focus according to these experts is to preserve function. Monitoring individuals, especially those who are still undergoing vertical growth is fundamental. It is suggested that preforming regular and ongoing assessments of neurological function is paramount, as well as teaching families the signs of TCS for which to monitor (e.g., back pain or declining lower extremity sensorimotor function). In addition to a careful physical examination, collaboration with urological colleagues and interpretation of urodynamic studies is crucial. If there has been a worsening of the neurogenic bladder function, according to the urodynamic study, then this is additional evidence that a surgery may be indicated for TCS. Only with sufficient evidence is TCS diagnosed and then timely release is performed with the goal of preserving spinal cord function and minimizing the recurrence of spinal cord tethering.
6. Future Implications in TCS Care and Research
The recent publication of the SBA’s updated guidelines may serve as a useful tool for the evaluation and management of TCS among individuals with SB internationally. As such, a standardized approach to the diagnosis and management of TCS could also be employed throughout Asia to allow for proper analysis and comparison of surgical outcomes among different treatment centers [17]. Moreover, we contend that the use of a standardized criteria will play a fundamental role in the global initiative to standardize the care and treatment of individuals with TCS across the globe.
7. Limitations
There are several limitations common to literature review studies. Our search was limited to studies published in English, peerreviewed, and indexed in PubMed (MEDLINE) or Embase databases. Therefore, it is possible that some eligible publications were excluded due to not having an English translation of the article. However, the use of broad search terms, additional examination of study reference lists, and the employment of a broad date range support confidence in our review. Factors that limited the synthesis of some of the findings included various sample sizes, study designs, indications, and outcomes measures. Another limitation of this study is the broad and often divergent definition of TCS used in the articles identified and included. It is acknowledged, however, that this is the nature of the current status of this body of literature throughout the region.
CONCLUSIONS
In summary, this study is the first to systematically review the literature from Asia relating to surgical management of TCS among individuals with NTDs. Significant differences in the diagnostic criteria and management of TCS were documented. As the surgical techniques for prenatal MMC closure continue to evolve, their adoption internationally is likely to continue. However, a documented potential increased rate of tethering following fetal surgery is reason for caution. In this setting, a clear and evidence-based approach to the definition and management of TCS is crucial. Therefore, the recent publication of the SBA’s updated care guidelines may serve as a useful tool for a systematized approach to TCS among individuals with SB in the region, as well as globally.
Notes
The authors have nothing to disclose.