 |
 |
- Search
| Neurospine > Volume 17(1); 2020 > Article |
|
|
Abstract
Objective
To assess the relationship of preoperative physical function, as measured by Patient-Reported Outcome Measurement Information System Physical Function (PROMIS PF), to improvement in mental health, as evaluated by Short Form-12 Mental Component Summary (SF-12 MCS) following anterior cervical discectomy and fusion (ACDF).
Methods
Patients undergoing primary ACDF were retrospectively reviewed and stratified based on preoperative PROMIS PF scores. PROMIS PF cohorts were tested for an association with demographic characteristics and perioperative variables using chi-square analysis and multivariate linear regression. Multivariate linear regression was utilized to determine the association between PROMIS PF cohorts and improvement in SF-12 MCS.
Results
A total of 129 one- to 3-level ACDF patients were included: 73 had PROMIS PF < 40 (ŌĆ£low PROMISŌĆØ) and 56 had PROMIS PF Ōēź 40 (ŌĆ£high PROMISŌĆØ). The low PROMIS cohort reported worse mental health preoperatively and at all postoperative timepoints except for 1 year. Both cohorts had similar changes in mental health from baseline through the 6-month follow-up. However, at 1 year. postoperatively, the low PROMIS cohort had a statistically greater change in mental health score.
Conclusion
Patients with worse preoperative physical function reported significantly worse preoperative and postoperative mental health. However, patients with worse preoperative physical function made significantly greater improvements in mental health from baseline. This suggests that patients with worse preoperative physical function can still expect significant improvements in mental health following surgery.
Patient-Reported Outcome Measurement Information System (PROMIS) has recently gained widespread attention as an efficient method of evaluating patient health before and after a variety of orthopedic and spinal procedures. The surveyŌĆÖs unique algorithm has allowed for a timely collection of clinical data compared to legacy outcome measures [1-3]. Since the introduction of PROMIS, multiple domains have been created to assess physical, mental, or social health. In relation to spine surgery, the PROMIS Physical Function (PF) domain has been particularly valuable due to its ability to accurately evaluate strength, mobility, and coordination. However, different utilities of the questionnaire are still being explored.
Aside from assessment of physical health, attention towards mental health has also become a major focus in the clinical spine setting. Although the literature contains evidence suggesting poor mental health leads to unfavorable recovery in physical function, there is a scarcity of studies focusing on the implications of poor preoperative physical function on improvement in mental health following surgery. Knowledge of the association between physical function and mental health improvements may allow physicians to better manage patient expectations and appropriately refer them for psychiatric evaluation when necessary.
Few investigations have evaluated the relationship between preoperative physical health and improvement in mental health following common spinal procedures such as anterior cervical discectomy and fusion (ACDF). In this context, the purpose of this investigation is to assess the relationship of preoperative physical function, as measured by PROMIS PF, to improvement in mental health, as evaluated by Short Form-12 Mental Component Summary (SF-12 MCS) following ACDF.
This study was approved by the Institutional Review Board of Rush University (ORA# 14051301). A prospectively-maintained database of patients undergoing primary, 1- to 3-level ACDF for degenerative pathology between 2015 and 2018 was retrospectively reviewed. All patients were treated by a single surgeon at a single academic institution. Patients with incomplete preoperative PROMIS PF scores or those that underwent an ACDF for nondegenerative pathology were excluded from the analysis.
Patients were stratified based on predetermined preoperative PROMIS PF cutoff scores: < 40 points (low PROMIS) and Ōēź 40 points (high PROMIS). A PROMIS PF score of 50 is the mean score of the general United States population with higher scores representing better physical function, and each 10-point interval equals one standard deviation above or below the mean score.
Demographic and baseline characteristics included age, sex, body mass index, smoking status, diabetes status, and comorbidity burden. Comorbidity burden was calculated using the Charlson Comorbidity Index with the age component removed. Perioperative variables included number of fusion levels, operative time, estimated intraoperative blood loss, length of hospital stay, and day of discharge.
The SF-12 MCS questionnaire was administered at the preoperative time point as well as at 6-weeks, 3-month, 6-month, and 1-year postoperative follow-up. The SF-12 MCS, which evaluates mental health, is a subcomponent derived from the original SF-12 survey. It has a mean score of 50 with higher scores representing better mental health.
Statistical analysis was performed using Stata/MP 13.0 for macOS Mojave (StataCorp LP, College Station, TX, USA). PROMIS PF cohorts were tested for an association with demographic characteristics and perioperative variables using Chi-squared analysis and multivariate linear regression. Additionally, multivariate linear regression was utilized to determine the association between PROMIS PF cohorts and improvement in SF-12 MCS following ACDF. Statistical significance was set at p < 0.05.
A total of 129 one- to 3-level ACDF patients were included in this analysis. Seventy-three (56.6%) had preoperative PROMIS PF < 40 (ŌĆ£Low PROMISŌĆØ) and 56 (43.4%) had preoperative PROMIS PF Ōēź 40 (ŌĆ£High PROMISŌĆØ). Baseline characteristics of the patient population are described in Table 1. There were no significant differences in age, sex, smoking status, body mass index, or comorbidity burden between the 2 cohorts (p > 0.05 for each). The low PROMIS cohort was more likely to be diabetic (20.6% vs. 7.1%, p = 0.033). There were no differences between cohorts in regard to operative levels, operative time, estimated blood loss, hospital length of stay, and day of discharge (p > 0.05 for each) (Table 2).
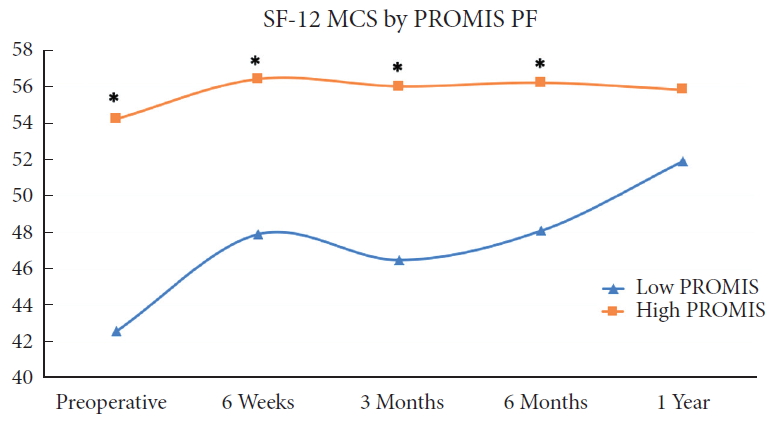
Table 3 provides a comparison of the SF-12 MCS scores between cohorts at the preoperative and postoperative timepoints (6 weeks, 3 months, 6 months, 1 year). The postoperative changes in SF-12 MCS from the preoperative baseline are also compared between the cohorts in Table 3. As demonstrated by Fig. 1, the low PROMIS cohort reported worse mental health than the high PROMIS cohort at the preoperative period and at all postoperative timepoints except for 1 year. Furthermore, both cohorts had similar changes in mental health from baseline through the 6-month follow-up (p > 0.05 for each). However, at the 1-year postoperative timepoint, the low PROMIS cohort had a statistically greater change in mental health score compared to the high PROMIS cohort (9.3 vs. 1.6, p = 0.003).
PROMIS PF is a computer adaptive assessment tool first developed by the National Institutes of Health that measures patient-reported health function. It can be used to quickly and efficiently assess patient disability in the preoperative period. In various orthopedic subspecialties, preoperative PROMIS PF scores have been valuable in predicting postoperative clinical outcomes [4,5]. In recent years, mental health has been a topic of interest in the field of spine surgery, as conditions such as depression have been determined to negatively impact recovery and pain relief after surgery [6,7]. However, few studies have investigated the utility of PROMIS PF to evaluate the course of mental health during the convalescent period after surgery [7-11]. Furthermore, while there is prior literature regarding effects of depression on outcomes of lumbar spinal surgery, there is a lack of studies examining the effects of depression on recovery following cervical spine surgery [12,13]. Therefore, the purpose of our study is to determine whether the PROMIS PF survey can be useful in predicting the preoperative and postoperative course of the mental health status of patients undergoing ACDF.
We retrospectively identified patients undergoing primary, 1- to 3-level ACDF and stratified them by preoperative disability as measured by PROMIS PF scores: worse physical function (scores < 40) and better physical function (scores Ōēź 40). Our results demonstrated that patients with worse preoperative physical ability were more likely to have diabetes. However, there were no significant differences in other demographic characteristics or perioperative outcomes. In regard to patient mental health status as assessed by the SF-12 MCS, the results of our study suggest that patients with worse preoperative physical function as indicated by their PROMIS PF scores are also more likely to have worse overall mental health. This is in agreement with a prospective cohort study conducted by Purvis et al. [14] that evaluated 148 adult patients prior to undergoing cervical spine surgery. The investigators concluded that the PROMIS PF domain strongly correlated with self-reported mental health outcomes assessed by surveys such as the GAD-7 (Generalized Anxiety Disorder-7) and PHQ-8 (Patient Health Questionnaire-8).
Our study establishes that patients with worse physical function before undergoing surgery are more likely to have worse mental health following surgery in comparison to patients with better preoperative physical function as denoted by the PROMIS PF. We observed this trend at every postoperative timepoint, although this difference was not statistically significant at 1 year. This may be explained by the fact that because patients with worse preoperative PROMIS scores had worse baseline SF-12 MCS scores, their SF-12 scores continued to be comparatively worse at every postoperative follow-up. However, while the high PROMIS cohort experienced minimal improvement in SF-12 from baseline postoperatively, the low PROMIS cohort demonstrated much larger improvements. As such, by the 1-year timepoint, the low PROMIS cohort reported a SF-12 score that had risen to the level close to that of the high PROMIS cohort, resulting in the lack of significant difference. This is in agreement with our finding of significant difference at 1 year when comparing the preoperative to postoperative change in SF-12 MCS scores between the 2 cohorts.
Prior studies have investigated the impact of baseline preoperative mental health symptomatology such as depression on postoperative outcomes following cervical spine surgery [15-20]. For instance, Adogwa et al. [21] demonstrated in their prospective study of patients with a known diagnosis of depression or anxiety undergoing ACDF that pretreatment of their mental condition resulted in significantly better postoperative outcomes in terms of pain and disability. Contrastingly, Asher et al. [22] found no relationship between preoperative general mental health as measured by the SF-36 MCS and postoperative patient-reported outcomes following minimally invasive lumbar spine surgery. Sundseth et al. [23] demonstrated a correlation between physical function assessed by the legacy outcome measure Neck Disability Index and the SF-36 MCS in patients scheduled to undergo surgery for cervical radiculopathy. It is important to note that none of these past investigations tracked the changes in the mental health of patients over time in either the short-term or long-term recovery period after undergoing surgery.
Additionally, our literature review resulted in several studies that investigated the utility of PROMIS PF in regard to the assessment of mental health. For example, Beleckas et al. [24] performed a cross-sectional study of 14,962 adult patients in an orthopedic practice and assessed the correlation of the various subdomains of the PROMIS survey, such as between the physical function component in relation to anxiety or depression scores. The authors concluded that there was a strong association between the physical function and anxiety assessments and recommended the anxiety component for clinical use to evaluate mental health in orthopedic patients. Another study by Merrill et al. [25] determined that depressed patients reported a greater magnitude of improvement in PROMIS PF than nondepressed patients, although depressed patients experienced worse postoperative outcomes in regards to depression, pain, and disability. It is worth nothing that while the aforementioned investigations are vital in informing the clinician about the relationship between patient mental health and PROMIS, none of the studies utilized PROMIS PF in order to predict postoperative changes in the mental status of patients following surgery. Therefore, to our knowledge, the present study is the first to follow the course of postoperative mental health outcomes longitudinally after stratifying patients into different cohorts based on preoperative PROMIS scores.
The results of our study clearly demonstrate that patients who report poorer physical function before undergoing ACDF are more likely to experience worse mental health both preoperatively and postoperatively compared to patients who started with better physical function. However, patients who have more physical disability also experience greater improvement from baseline and end up reporting similar mental health status by the 1-year postoperative timepoint. Therefore, patients who report worse physical and mental capacities before undergoing ACDF can expect to benefit from significant improvement in mental health after surgery that results in comparable mental health outcomes in the long-term relative to their counterparts with better preoperative function. This is supported by our finding that patients in the low PROMIS cohort demonstrated statistically significant postoperative improvement of SF-12 MCS scores from their preoperative baseline at the 1-year timepoint. Furthermore, patients in the low PROMIS cohort and high PROMIS cohort demonstrated comparable SF-12 MCS scores at the 1-year timepoint. Both of these results suggest that patients who start with worse preoperative physical function may still experience significant improvements in mental health following the ACDF procedure. It is our hope that the present study is helpful to the practicing spine surgeon in terms of the risk stratification of patients who are considering spinal surgery, as well as an aid in counseling of patients regarding expectations for the recovery period following surgery.
PROMIS PF can be regarded as an indispensable clinical tool that allows surgeons to predict the mental health outcomes of patients after spine surgery. However, the present study has several limitations. First, the retrospective nature of this study means there is an inherent element of selection bias. Second, all patients were treated by a single surgeon at a single teaching center, which may limit the generalizability of our results to a larger, more diverse population. Third, we did not take into account other factors which may influence the postoperative convalescence period, including adherence to prescribed medication regimen and physical therapy attendance, formal psychiatric treatment, and patient expectations about recovery. Fourth, previous psychosocial history, formal psychiatric diagnoses, or treatments prescribed for the patients in our study were not included as part of our assessment of mental health. Lastly, survey data was limited to 1 year due to incomplete survey completion in the longer-term. Moving forward, a higher-powered, prospective study using preoperative PROMIS PF scores is necessary in order to form predictive models for postoperative recovery in mental health for patients undergoing ACDF for degenerative pathology.
In this retrospective investigation, we identified patients with varying physical function using PROMIS PF and compared mental health outcomes as assessed by the SF-12 MCS survey following ACDF. Patients with worse preoperative physical function reported significantly worse preoperative and postoperative mental health. However, both cohorts demonstrated similar clinical recovery at the 1-year follow-up. Therefore, the SF-12 MCS of patients with worse preoperative physical function might be improved in the long-term postoperative time period. In addition, patients with worse preoperative physical function made significantly greater improvements in mental health from baseline. These findings suggest that patients with worse preoperative physical function can still expect significant improvements in mental health following surgery and should be counseled to expect a similar long-term postoperative outcome compared to patients with better preoperative physical function. Moving forward, further research will be essential in elucidating the extent to which physical function influences mental health in procedure-specific spine populations such as ACDF.
Fig.┬Ā1.
Comparison of SF-12 MCS outcomes between PROMIS PF cohorts at each timepoint following anterior cervical discectomy and fusion. SF-12 MCS, Short Form-12 Mental Component Summary; PROMIS PF, Patient-Reported Outcome Measurement Information System Physical Function. *Statistical significance when comparing SF-12 MCS values between cohorts at each timepoint.
Table┬Ā1.
Baseline characteristics by preoperative PROMIS PF scores
| Characteristic | Low PROMIS (n = 73) | High PROMIS (n = 56) | p-valueŌĆĀ |
|---|---|---|---|
| Age (yr) | 49.6 ┬▒ 9.4 | 50.6 ┬▒ 10.4 | 0.603 |
| Sex | 0.499 | ||
| ŌĆāFemale | 27 (37.0) | 24 (42.9) | |
| ŌĆāMale | 46 (63.0) | 32 (57.1) | |
| Smoking status | 0.745 | ||
| ŌĆāNonsmoker | 64 (87.7) | 48 (85.7) | |
| ŌĆāSmoker | 9 (12.3) | 8 (14.3) | |
| Diabetes status | 0.033* | ||
| ŌĆāNondiabetic | 58 (79.5) | 52 (92.9) | |
| ŌĆāDiabetic | 15 (20.6) | 4 (7.1) | |
| BMI category | 0.130 | ||
| ŌĆāNonobese (< 30 kg/m2) | 38 (52.8) | 37 (66.7) | |
| ŌĆāObese (Ōēź 30 kg/m2) | 34 (47.2) | 19 (33.9) | |
| Modified CCI | 0.8 ┬▒ 0.9 | 0.6 ┬▒ 1.0 | 0.260 |
Values are presented as mean┬▒standard deviation or number (%).
Low PROMIS cohort defined as preoperative PROMIS score <40.
High PROMIS cohort defined as preoperative PROMIS score Ōēź40.
PROMIS PF, Patient-Reported Outcome Measurement Information System Physical Function; CCI, Charlson Comorbidity Index; BMI, body mass index.
Table┬Ā2.
Perioperative outcomes by preoperative PROMIS PF scores
| Characteristic | Low PROMIS (n = 73) | High PROMIS (n = 56) | p-valueŌĆĀ |
|---|---|---|---|
| No. of fusion levels | 0.635 | ||
| ŌĆā1-Level | 40 (54.8) | 35 (62.5) | |
| ŌĆā2-Level | 28 (38.4) | 17 (30.4) | |
| ŌĆā3-Level | 5 (6.9) | 4 (7.1) | |
| Operative time (min) | 52.0 ┬▒ 15.4 | 51.6 ┬▒ 14.6 | 0.892 |
| Estimated blood loss (mL) | 29.9 ┬▒ 12.3 | 29.8 ┬▒ 13.8 | 0.986 |
| Length of stay (hr) | 14.1 ┬▒ 14.0 | 10.3 ┬▒ 7.4 | 0.092 |
| Discharge date | 0.411 | ||
| ŌĆāPOD 0 | 37 (57.8) | 35 (70.0) | |
| ŌĆāPOD 1 | 15 (23.4) | 9 (18.0) | |
| ŌĆāPOD 2 | 2 (3.1) | 0 (0) | |
| ŌĆāPOD 3+ | 10 (15.6) | 6 (12.0) |
Table┬Ā3.
SF-12 MCS by preoperative PROMIS PF scores
| SF-12 MCS | Low PROMIS (n = 73) | High PROMIS (n = 56) | p-valueŌĆĀ |
|---|---|---|---|
| SF-12 MCS | |||
| ŌĆāPreoperative | 42.6 ┬▒ 14.1 | 54.2 ┬▒ 8.7 | < 0.001* |
| ŌĆā6-Week | 47.9 ┬▒ 13.3 | 56.4 ┬▒ 6.7 | < 0.001* |
| ŌĆā3-Month | 46.5 ┬▒ 14.2 | 56.0 ┬▒ 7.7 | < 0.001* |
| ŌĆā6-Month | 48.1 ┬▒ 13.7 | 56.2 ┬▒ 7.0 | 0.001* |
| ŌĆā1-Year | 51.9 ┬▒ 13.2 | 55.8 ┬▒ 8.6 | 0.440 |
| Postoperative change (postop ŌĆō preop) | |||
| ŌĆā6-Week ╬ö | 5.3 ┬▒ 10.9 | 2.2 ┬▒ 7.7 | 0.589 |
| ŌĆā3-Month ╬ö | 3.9 ┬▒ 11.5 | 1.8 ┬▒ 8.2 | 0.115 |
| ŌĆā6-Month ╬ö | 5.5 ┬▒ 13.1 | 2.0 ┬▒ 9.6 | 0.775 |
| ŌĆā1-Year ╬ö | 9.3 ┬▒ 12.1 | 1.6 ┬▒ 8.8 | 0.003* |
Values are presented as mean┬▒standard deviation.
Low PROMIS cohort defined as preoperative PROMIS score <40.
High PROMIS cohort defined as preoperative PROMIS score Ōēź40.
SF-12 MCS, Short Form-12 Mental Component Summary; PROMIS PF, Patient-Reported Outcome Measurement Information System Physical Function; ╬ö, postoperative SF-12 MCS ŌĆō preoperative SF-12 MCS.
REFERENCES
1. Koltsov JCB, Greenfield ST, Soukup D, et al. Validation of Patient-Reported Outcomes Measurement Information System computerized adaptive tests against the foot and ankle outcome score for 6 common foot and ankle pathologies. Foot Ankle Int 2017 38:870-8.


2. Brodke DJ, Saltzman CL, Brodke DS. PROMIS for orthopaedic outcomes measurement. J Am Acad Orthop Surg 2016 24:744-9.


3. Boody BS, Bhatt S, Mazmudar AS, et al. Validation of Patient-Reported Outcomes Measurement Information System (PROMIS) computerized adaptive tests in cervical spine surgery. J Neurosurg Spine 2018 28:268-79.



4. Ho B, Houck JR, Flemister AS, et al. Preoperative PROMIS scores predict postoperative success in foot and ankle patients. Foot Ankle Int 2016 37:911-8.


5. Chen RE, Papuga MO, Voloshin I, et al. Preoperative PROMIS scores predict postoperative outcomes after primary ACL reconstruction. Orthop J Sports Med 2018 6:325967118771286.

6. Miller JA, Derakhshan A, Lubelski D, et al. The impact of preoperative depression on quality of life outcomes after lumbar surgery. Spine J 2015 15:58-64.


7. Tuck AN, Scribani MB, Grainger SD, et al. The 9-Item Patient Health Questionnaire (PHQ-9): an aid to assessment of patient-reported functional outcomes after spinal surgery. Spine J 2018 18:1398-405.


8. Cassin S, Sockalingam S, Hawa R, et al. Psychometric properties of the Patient Health Questionnaire (PHQ-9) as a depression screening tool for bariatric surgery candidates. Psychosomatics 2013 54:352-8.


9. Choi Y, Mayer TG, Williams MJ, et al. What is the best screening test for depression in chronic spinal pain patients? Spine J 2014 14:1175-82.


10. Adogwa O, Parker SL, Shau DN, et al. Preoperative Zung depression scale predicts patient satisfaction independent of the extent of improvement after revision lumbar surgery. Spine J 2013 13:501-6.


11. Phan K, Moran D, Kostowski T, et al. Relationship between depression and clinical outcome following anterior cervical discectomy and fusion. J Spine Surg 2017 3:133-40.



12. Skeppholm M, Fransson R, Hammar M, et al. The association between preoperative mental distress and patient-reported outcome measures in patients treated surgically for cervical radiculopathy. Spine J 2017 17:790-8.


13. Pakarinen M, Vanhanen S, Sinikallio S, et al. Depressive burden is associated with a poorer surgical outcome among lumbar spinal stenosis patients: a 5-year follow-up study. Spine J 2014 14:2392-6.


14. Purvis TE, Andreou E, Neuman BJ, et al. Concurrent validity and responsiveness of PROMIS health domains among patients presenting for anterior cervical spine surgery. Spine (Phila Pa 1976) 2017 42:E1357-65.


15. He J, Xiong W, Li F, et al. Depression influences pain and function after cervical disc arthroplasty. J Neurosurg Sci 2017 61:39-45.


16. Lubelski D, Alentado V, Nowacki AS, et al. Preoperative nomograms predict patient-specific cervical spine surgery clinical and quality of life outcomes. Neurosurgery 2018 83:104-13.



17. Alvin MD, Miller JA, Lubelski D, et al. The impact of preoperative depression and health state on quality-of-life outcomes after anterior cervical diskectomy and fusion. Global Spine J 2016 6:306-13.


18. Alvin MD, Miller JA, Sundar S, et al. The impact of preoperative depression on quality of life outcomes after posterior cervical fusion. Spine J 2015 15:79-85.


19. Diebo BG, Tishelman JC, Horn S, et al. The impact of mental health on patient-reported outcomes in cervical radiculopathy or myelopathy surgery. J Clin Neurosci 2018 54:102-8.


20. Elsamadicy AA, Adogwa O, Cheng J, et al. Pretreatment of depression before cervical spine surgery improves patientsŌĆÖ perception of postoperative health status: a retrospective, single institutional experience. World Neurosurg 2016 87:214-9.


21. Adogwa O, Elsamadicy AA, Cheng J, et al. Pretreatment of anxiety before cervical spine surgery improves clinical outcomes: a prospective, single-institution experience. World Neurosurg 2016 88:625-30.


22. Asher R, Mason AE, Weiner J, et al. The relationship between preoperative general mental health and postoperative quality of life in minimally invasive lumbar spine surgery. Neurosurgery 2015 76:672-9.



23. Sundseth J, Kolstad F, Johnsen LG, et al. The Neck Disability Index (NDI) and its correlation with quality of life and mental health measures among patients with single-level cervical disc disease scheduled for surgery. Acta Neurochir (Wien) 2015 157:1807-12.




- TOOLS
- Related articles in NS
-
Journal Impact Factor 3.2



























