Heterotopic Ossification after Cervical Arthroplasty with ProDisc-C: Time Course Radiographic Follow-up over 3 years
Article information
Abstract
Objective
Heterotopic ossification (HO) is a well-known complication after total hip replacement. But the occurrence rate by the time-course, clinical effect and risk factors of HO after total cervical disc replacement (TCDR) are not well described. The purpose of this study is to evaluate the occurrence rate by the time-course and risk factors for HO after TCDR with a ProDisc-C.
Methods
Thirty-two patients whom followed up more than one year after the TCDR are enrolled. Radiographic study was done at 12, 24 and 36 months after the TCDR and classified HO with McAfee classification. Segmental range of motion, preoperative existence of spondylosis, type of operation, disc space occupying ratio by artificial disc, surgical level are analyzed to identify the risk factors of HO. The visual analog scale and the neck disability index were evaluated preoperatively and at last follow-up time for clinical parameters.
Results
Eighteen patients (56%) showed HO at 12 months, 18 patients (86%) showed HO at 24 months and 6 patients (89%) showed HO at 36 months after the TCDR. Clinical significant HO(Grade 3 and 4) was shown in one patient (3%) at 12 months, 3 patients (14%) at 24 months and 5 patients (56%) at 36 months. Only post-operative follow-up period increases the risk of development clinical significant HO. All patients showed improvement of clinical parameters (p<0.005).
Conclusion
Incidence of HO is getting higher as time course progress. However, there are no relation between clinical outcome and radiologic change of ROM and the grade of HO.
INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) is golden standard for treatment of cervical degenerative disc disorders with a long term clinical success7,19). Although ACDF shows the excellent clinical and radiologic outcomes, it may leads to symptomatic adjacent segment degeneration. According to Hillbrand et al.10) symptomatic new disease occurred at an adjacent level at the relatively constant incidence of 2.9 percent per year in the ten years after the operation. In addition, within 10 years, up to 25% of all patients treated with ACDF may have symptomatic adjacent segment disc degeneration. Increased longitudinal or shear strain after ACDF contribute adjacent segment disc degeneration16). Recent study suggested that total cervical disc replacement (TCDR) can be alternative treatment option20). TCDR preserve disc joint mobility and restore disc height, which is considered to prevent adjacent level degeneration. However, in terms of incidence of adjacent level degeneration, it is unclear that TCDR have clinical advantage.
Heterotopic ossification (HO) is well known complication after total hip arthroplasty4,13,23). HO and spontaneous fusion in patient treated with TCDR have been reported. According to Mehren et al.18), Grade III HO was observed in 10.4%, and Grade IV HO was observed in 9.1% of the implanted cases in a 1 year follow up. But the occurrence rate by the time-course, clinical effect and risk factors of HO after total cervical disc replacement (TCDR) are not well described.
We designed this study to analyze the occurrence rate by the time-course and possible risk factors for HO after the TCDR with a ProDisc-C.
MATERIALS AND METHODS
From September, 2005 to October, 2008, 48 patients underwent TCDR with a ProDisc-C(Synthes, Inc., West Chester, PA) by one surgeon and 32 patients whom followed up more than one year after the operation are enrolled in this study. Clinical and radiologic data of these 32 patients were retrospectively reviewed.
TCDR was performed by standard anterior cervical approach and microdiscectomy was done, but the posterior longitudinal ligament was retained as much as possible. Meticulous hemostasis of soft-tissue bleeding was done and bone bleeding was controlled with a bone wax before insertion of artificial disc. Patients with degenerative disc herniation with no or minor spondylosis between C3/4 and C6/7 were included. Exclusion criteria were segmental instability, severe spondylosis, ossification of posterior longitudinal ligament and severe disc height loss.
Radiographic and clinical evaluation was done at 12 months, 24 months and 36 months after the TCDR. Routine cervical anteroposterior (AP), lateral, dynamic views were taken to identify HO. Classification of HO was done according to modified McAfee classification that are proposed by Mehren et al18). The classification has 5-points grade: grade 0=no HO present; grade 1=presence of HO but not in the interdiscal space; grade 2=presence of HO in the interdiscal space; grade 3=bridging of ossification with segment movement; grade 4=complete fusion without movement in flexion/extension. We also defined HO grade above 2 (HO grade 3 and 4) as a clinical significant HO.
To evaluate risk factors of HO, patient's age, sex, follow up period, segmental range of motion (ROM), preoperative existence of spondylosis, type of operation (TCDR vs hybrid operation), disc space occupying ratio by artificial disc, operation level, number of surgical level (single level vs multi-level) and pre-operative disc grade were analyzed. Pfirrmann's lumbar disc degeneration grade was used to evaluate pre-operative disc grade22). On the pre-operative flexion/extension view, segmental ROM was checked. Segmental ROM was calculated by ratio of summation of Cobb's angles of implanted disc space per summation of Cobb's angles between C2 and C7 on flexion and extension view(Fig. 1). Cobb's angle of implanted disc space was measured between upper parallel end plate line of upper vertebral body and lower parallel end plate line of lower vertebral body of implanted disc. Lordosis angle was expressed as positive, whereas kyphosis angle was expressed as negative. Disc space occupying ratio by artificial disc was evaluated as a ratio to anteroposterior diameter of the vertebral body and length of ProDisc-C in disc space (Fig. 2). Pre-operative existence of spondylosis was identified on both simple X-ray and cervical computed tomography (CT).
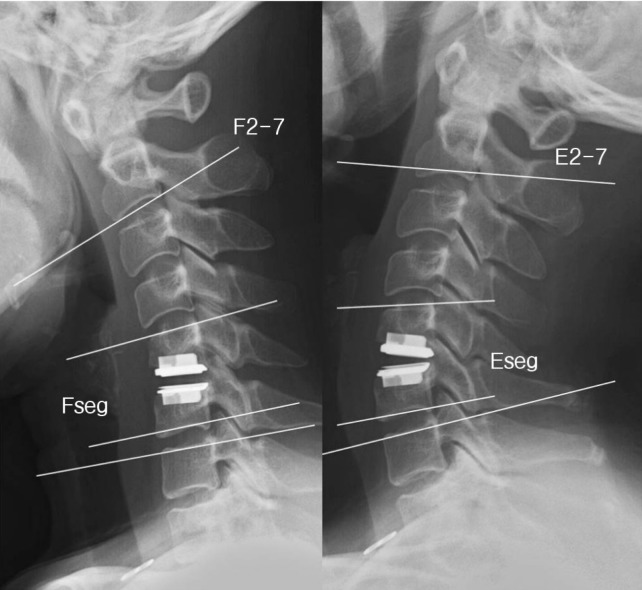
Illustration of segmental range of motion (SROM) measurement. SROM was measured using dynamic flexion and extension image. Fseg=segmental cobb's angle of implanted disc space in flexion view, Eseg=segmental cobb's angle of implanted disc space in extension view, F2-7 and E2-7=cobb's angle between lower margin of C2 body and upper margin of C7 body. SROM=(Fseg+Eseg/F2-7+E2-7)*100
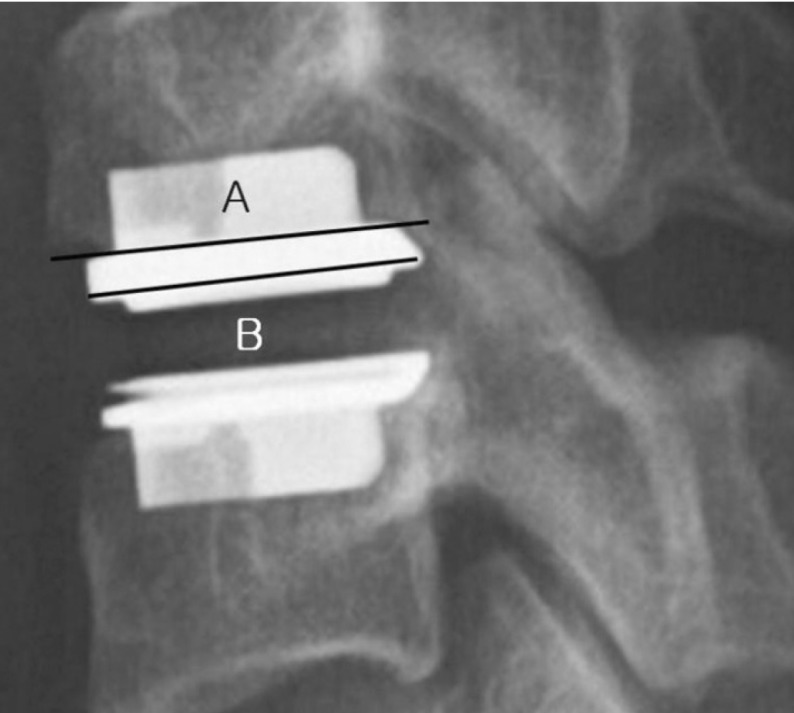
Disc space occupying ratio by artificial disc was measured using simple X-ray lateral image. Occupying ratio=B/A*100; A: anteroposterior diameter of vertebral body; B: anteroposterior diameter of artificial disc.
For clinical parameters, the visual analog scale (VAS) and the neck disability index (NDI) were evaluated preoperatively and at the time of the last follow-up.
Statistical analysis was done using chi square test and multiple logistic regression tests. All p values less than 0.05 were considered statistically significant.
RESULTS
The group consisted of 25 men and 7 women and their average age of all patients was 41.7 years (range 27-67 years). Total of thirty two patients were followed at least 1 year, 21 patients for 2 years and 12 patients for 3 years. Five patients (15.6%) underwent hybrid operation (combined TCDR and ACDF). A single level surgery was performed in 27 patients (84.4%), two levels (hybrid operation) in 3 (9.3%) and three levels (hybrid operation) in 2 patients (6.3%). Total 34 ProDisc-C prostheses were implanted, the C3/4 intervertebral disc was replaced in 1 (2.9%), C4/5 in 5 (14.7%), C5/6 in 38 (59%) and C6/7 in 6(17.7%). Fifteen patients (47%) showed pre-operation disc grade 3 and the others in 4 (Table 1).
At 12 month follow-up, eighteen patients (56%) showed HO and one patient (3%) showed clinical significant HO. At 24 months follow up, 18 patients (86%) showed HO and significant HO was shown in 3 patients (14%). At 36 months follow up, 11 patients (91.7%) showed HO and 5 patients (41.7%) presented clinical significant HO(Fig. 3 and 4). As far as 36 months followed up, there was no grade IV HO.

Occurrence rate of HO by postoperative period (%). Total 56% of patients showed HO at 12 months while 86% at 24 months and 91.7% at 36 months showed HO after TCDR.
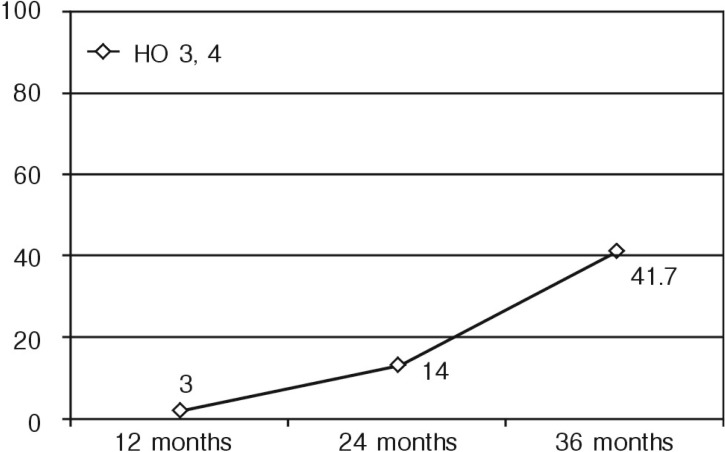
Clinical significant HO by postoperative period (%). Three percent of patients showed clinical significant HO at 12 months, 14% at 24 months and 41.7% at 36 months after TCDR. Longer period after operation increase risk of clinical significant HO (p=0.043).
No association was found between the development of HO and assessed risk factors. Patient's age (p=0.624), sex (p=0.193), existence of spondylosis (p=0.229), pre- and post-operative ROM(p=0.540), number of surgical level (p=0.691), disc space occupying ratio by artificial disc (p=0.643), type of operation (p=0.131), disc grade (p=0.445) and operation level (p=0.691) were not related to the risk factors for formation of HO(Table 2). However, post-operative follow-up period was the only statistically significant factor that showed formation of HO after TCDR(p=0.043) (Fig. 4). Preoperative NDI was improved from 41.71 to 13.41 at last follow up, mean VAS in neck pain decreased from 4.71 preoperatively to 1.29 at last follow-up time, and VAS in arm pain decreased from 7.71 to 0.86 at last follow-up time (Fig. 5).
DISCUSSION
Both traditional ACDF and TCDR show good clinical outcome. And a few randomized controlled studies demonstrated a better clinical outcome in the group of TCDR than the groups of ACDF5,24). Potential benefit of TCDR is maintaining of segmental motion to preserve physiological ROM. And moreover theoretically TCDR reduce the adjacent segment disease. Some studies showed that fusion increase the motion and intradiscal pressure at the adjacent segment while arthroplasty did not8,9,26). However, a few studies have been reported the HO as complication of the TCDR and even more fusion has been reported after the TCDR1,21).
Various range of occurrence rate of HO after TCDR have been reported. Occurrence rate of HO at 12 months after surgery ranged from 17.8 to 72.3% while clinical significant HO showed range of 4.2 to 23.1%. At 24 months after the surgery showed 28.8% to 78.5% of occurrence rate of HO and 8.5% to 32.3% range of clinical significant occurrence rate of HO14,15,18,25,28). Pooled prevalence of HO was 44.6% at 12 months and 58.2% at 24 months after TCDR, while clinical significant HO was 11.1% and 16.7% respectively6). Our series showed higher occurrence rate of HO at 12 and 24 months after TCDR than previously reported article, but similar occurrence rate of clinical significant HO is shown. However, HO was evaluated only on the simple plain X-ray in our study. If the existence of HO was evaluated on cervical CT, a higher incidence of HO might be reported3). However, there were no grade 4 HO at the 36 months after TCDR so far, but grade 4 could be seen if the longer post-operative period is followed.
Many studies about relationship between HO and TCDR have been reported. Various clinical factors have been suggested as risk factors for HO. According to Leung et al.15) male sex and older age were associated with development of HO. In our series neither sex nor old age did not increase occurrence rate of HO. Other studies demonstrate a higher rate of HO formation in patient with spondylosis or degenerative change than in those with a soft-disc herniation3,27). Our study also tried to see the relationship between HO formation and degree of pre-operative degeneration. Therefore we evaluated pre-operative disc grade using Pfirmann's grade22) and pre-operative existence of spondylosis using cervical CT. However, we exclude severe spondylosis and disc height loss patients, and it may make difference in result. Removal of posterior osteophyte is mandatory for patients with cervical spondylosis. Remained bone dust after removal of osteophyte may promote formation of HO. We minimized drilling of posterior osteophyte and retained posterior longitudinal ligament as much as possible.
Yi et al.28) suggested different types of prosthesis shows different occurrence rate of HO may be due to different biomechanical mechanism of prosthesis types. To avoid the effect of biomechanics and biomaterial of prosthesis device to formation of HO, we restricted to one type of artificial disc. They proposed that well fitting prosthesis device in AP diameter could prevent formation of HO. We measured disc space occupying ratio by artificial disc on immediate post-operative simple X-ray. Either increased or decreased pre-operative segmental ROM may act as a risk factor for formation of HO. However, our series showed that there were no relations between HO occurrence rate and both clinical factors. Mehren et al.18) reported higher rate of HO in multi-level case than mono-level case. However, our series shows no differences but very limited number of cases of multi-level TCDR was enrolled. There were no clinical parameters that are related to occurrence of HO. So far, only the longer post-operative period increase the risk of HO in this study. That may be due to as normal physiologic compensation to iatrogenic instability which was induced by removing of both anterior and posterior longitudinal ligament and some part of uncinate process.
There were no correlation between formation of HO and clinical outcome. In this study, there was good clinical improvement in the VAS, NDI. Some studies have reported that HO is less important in the absence of clinical deterioration2,12). Until now, there is no evidence that whether all HO finally progressed spontaneous fusion. And also recent study demonstrated that TCDR does not prevent development of adjacent segment disease11). However, decreased motion on TCDR segment from HO is the complication of TCDR and against the fundamental goal of TCDR.
There were some limitations in our study. The more cases are needed, and all patients should be followed same period and longer follow-up study should be followed. We analyzed risk factors could affect HO formation. Although no clinical association was founded, we expect this result could help decision making of performing TCDR.
CONCLUSION
Relatively high incidence of HO was shown and about 42% of clinical significant HO was shown at 36 months after the TCDR. However, there was no complete fusion in this study. In terms of clinical improvement, TCDR is comparable to ACDF. Clinical improvement was not correlated with grade of HO and radiologic change of ROM. HO formation risk was not correlated with clinical parameters. Only longer post-operative period increase the risk of HO formation.


