The History, Present, and Future of Spine Surgery in Switzerland
Article information

INTRODUCTION
Despite being a rather small country (area, 41.285 km2; population, 8.5 million), embedded in the center of surrounding Europe, Switzerland looks back on a long tradition of care for patients with diseases of the spine. It has always been a hub for innovation. The alpine landscape and the originally strong focus on physically demanding agricultural work in Switzerland inevitably led to early expertise with traumatic and degenerative spinal diseases. Several Swiss protagonists have therefore pioneered the diagnosis and treatment of traumatic, degenerative, but also infectious and oncological spinal conditions [1].
From a global perspective, the history of spine surgery is relatively much influenced by contributions of surgeons from the United Kingdom and North America. This is probably inevitable, taking into consideration that most articles on the history of neuro- and spine surgery stem from English-speaking authors who cannot take into account early works of authors published in German, French, or other languages [2]. The quality of Swiss spine care continuously improved, owing to the achievements of several eminent leaders and the early foundation of a neurosurgical department in Zurich in 1937 by Hugo Krayenbühl (1902–1985) [3].
Today, there is a trend towards the foundation of interdisciplinary spine units at academic and larger nonuniversity hospitals. Several strong national spine societies, industry partners, and globally active organizations such as AOSpine and Eurospine are based in Switzerland and promote excellence in Swiss spine care. Spine surgery is an essential part of the training curriculum for neurosurgeons; however, less so for orthopedic spine surgeons. Endeavors are ongoing to harmonize operative spine care across those 2 specialties. An interdisciplinary subtitle for spine surgery was recently created and accepted by the Swiss Medical Council. This title expresses a special competence in spine surgery and can be achieved by board-certified neurosurgeons or orthopedic surgeons.
This article aims to provide an overview of some of the past achievements, present issues, and a possible future outlook of Swiss spine surgery.
PIONEERS IN SWISS SPINE CARE
Several leading surgeons at the end of the 19th century—among them Ernst von Bergmann (1836–1907), Emil Theodor Kocher (1841–1917), Rudolf Ulrich Krönlein (1847–1910)—were protagonists of and built a triumvirate for modern, scientifically-oriented medicine [4]. Inspired by the physiological experiments as promoted by Victor Horsley (1857–1916) and Francois Magendie (1783–1855), they terminated the previous era of speculative nature philosophy in the field of surgery. With the introduction of antisepsis as a standard operating procedure in surgery after 1867, following the ground-breaking works of Ignaz Philipp Semmelweis (1818–1865) and Joseph Lister (1882–1912), infections as feared complications after surgery occurred less frequently and paved the way for an increase in the total number of surgeries, including spine surgeries [1]. The pioneering momentum of early academic spine care in Switzerland was desperately lost with the beginning of World War I, as in the rest of Europe [4].
1. Spine Trauma
Being a mountainous region, Switzerland traditionally deals with a considerable number of accidents involving the spine. Some of the earliest descriptions of modern surgical treatment for spine trauma in Switzerland originate from Kocher, who was appointed professor and director of the Surgical University Hospital in Berne. He had seen and learned innovative surgical techniques during many educational trips throughout Germany, England, France, and Austria [5]. In his 1892 publication “Chirurgische Operationslehre” (= Surgical Textbook) he describes the technique of laminectomy and refers to the successes observed at Victor Horsley’s (1857–1916) institution when applying laminectomy for the decompression of the spinal canal in the context of spine trauma and tumors (Fig. 1) [6]. Four years later, he dedicated a further 245-page monography to the diagnosis and treatment of spine trauma, which summarizes his observations in 78 patients (treated between 1872–1896) and provided evidence that he undertook manual repositioning maneuvers (e.g., using the Glisson-sling for unilateral facet joint dislocation) and decompressive laminectomies. He categorized spine trauma into partial (contusion and distortion of the vertebral body, isolated fractures of the vertebral arch and the spinous process, isolated dislocation of the facet joints, isolated fractures of the vertebral body) or total (dislocation and compression fractures with the affection of one or both vertebral joints, total dislocation trauma with the affection of the intervertebral disc, and total dislocation trauma with the affection of both facet joints and distraction of the fracture surface of the vertebral body). In extensive discussions and profound detail, the clinical courses, pathological findings, therapies, and postmortem findings were reported. From his observations in individual case-vignettes, he published a dermatome chart as appendix “Tafel IV,” which is among the earliest illustrations of this kind in the medical literature (Fig. 2) [5]. This paved the way to a more precise lesion localization, which should be essential for future neuro- and spine surgery to develop. With the introduction of X-ray by Conrad Röntgen (1845–1923) in 1895, imaging of spinal fractures was made possible and helped improve their management.
The operative treatment of spine trauma beyond laminectomies was uncommon for a long time. Fritz De Quervain (1868–1940) from Berne published an early report of a fusion operation of the cervical spine in December 1911 [7]. He operated on a patient with dislocation of the fifth over the sixth cervical vertebra and performed fusion with the use of a portion of the scapula as a bone graft.
In the following decades, advances in spinal traumatology were made in Switzerland and elsewhere. We would like to point out the manifold and meaningful contributions of the Austrianborn orthopedic surgeon Friedrich Paul Magerl (*1931), who worked at the Kantonsspital St. Gallen (north-eastern part of Switzerland – close to the borders of Germany and Austria) from 1970 onwards and became department head in 1987. In the 1970s, based on the contributions of Jörg Böhler (1917–2005), he helped developed the compressive anterior screw osteosynthesis for dens fractures [8,9]. In 1976, he proposed a “fixateur externe” for the treatment of unstable spinal fractures, which had favorable biomechanic properties compared to other available therapeutic options at that time [10,11]. In 1987, he published an alternative C1–2 fixation by passing threaded screws across the atlantoaxial facet joints from posterior, ending in the lateral mass of C1, which is still used as “transarticular screw fixation” today [12]. Furthermore, he proposed a modern classification system of thoracolumbar spinal fractures which relied on computed tomography (CT)-findings and was based on both the 3-column concept by Denis and the McAfee classification [13].
Similarly, Walter Theodor Dick (*1943) should be mentioned, who was a professor and became director of Orthopedic Surgery in Basel in 1995. He contributed significantly to the stateof-the-art treatment of spinal trauma, among other conditions, by proposing the “fixateur interne” using long Schanz screws, inserted from a posterior approach through the pedicles [14]. The long leverarms of the Schanz screws facilitated reduction maneuvers—even when using short constructs—and have been further developed and refined manifold.
2. Degenerative Disc Disease
One of the oldest publications dealing with acute or chronic diseases by Caelius Aurelianus (5th century A.D.) was edited by Johann Conrad Ammann (1669–1730) from Schaffhausen (city in the North of Switzerland, bordering to Germany). The first chapter of the fifth book was dedicated to “De Isciadicis & Psaeadicis” (= sciatica and lumbar back pain) and contained one of the most detailed descriptions of sciatic pain. Here, Caelius places particular emphasis on the topography and chronology of sciatica pain, as the following quotation proves: “...pain in the vertebrae is followed by pain in the buttocks, sometimes on both sides (bilateral sciatica), heaviness of the limbs, unusual gait problems, sometimes with slight numbness and paresthesia, occasionally with severe, stabbing and burning pain, which makes the patient move and winde like a snake; the sick cannot even find a bearable position in bed and sometimes fever occurs...” (cited after [15]) In the more chronic stages, weakness, paralysis, atrophy, and contracture-related shortening of the leg are mentioned. However, Caelius did not discriminate between arthritic joint- and radicular nerve pain and sciatic pain, in general, was in the antiquity, middle ages until the modern time a heterogeneous group of etiologically different disease entities [15]. With humoral pathology as predominant doctrine from the Hippocratic writings, theories of the 4 humors were used to explain sciatic pain until the middle of the 19th century.
In 1841 and 1864, the French physicians Francois Louis Isidore Valleix (1807–1855) and Ernest-Charles Lasègue (1816–1883) described clinical maneuvers that exacerbate radicular leg pain, which provided evidence that sciatica was related to stretching of the sciatic nerve [16,17]. In Switzerland it was again Kocher, who pointed out the possibility of intervertebral disc (IVDs) rupture in 1896 already [5,18,19]. He may have been aware of the findings of Hubert von Luschka (1820–1875) from Tübingen, Germany who described subligamentous disc herniations, originating from the Nucleus pulposus [20]. At that time, however, IVD rupture was not considered a degenerative but a traumatic or neoplastic disorder by many famous physicians of this time including Luschka, Heinrich O. Oppenheim (1858–1919), Fedor Krause (1857–1937), Goldthwait, George S. Middleton (1853–1928), and John H. Teacher (1869–1930) [21]. Also in his report, Kocher described the case of a 26-year-old male who fell from a 30-m height and suffered from traumatic IVD rupture at the L1/2 level [5,18,19].
In 1929, the Zurich-based neurologist Otto Veraguth (1870–1944) and his surgeon-friend Hans Brun (1874–1946) from Lucerne published a case, where they reported the clinical course, diagnostic workup and successful surgical treatment of a 36-year-old female with progressive signs of cauda equina syndrome. The historical value of this early report was recently summarized in detail [21]: following a thorough neurological examinations with evidence of worsening pain and neurological deficits, a suboccipital tap, and installation of oily contrast agent was conducted to help outline a blockage of cerebrospinal fluid at the L4/5 level in subsequent X-ray studies. As the patient progressed to develop complete incontinence, Brun performed an L4–5 laminectomy and felt the resistance of about the size of a cherry pit by manually palpating the dura. After a ventral durotomy, the lesion was resected and histologically examined. Even though the pathologist diagnosed an “extradural myxochondroma,” the figure provided along with Veraguth’s publication clearly shows IVD tissue [21,22]. Reports by Dandy on the successful resection of IVD fragments in patients with cauda syndrome were published in the same year [23]. The relationship between degeneration of the lumbar discs, as well as between lumbar disc herniation and sciatic leg pain, was finally established with the Landmark paper by Mixter and Barr [24] in 1934. Disc surgery began to be more established at the neurosurgical department in Zurich from 1938 onwards [3,25], with continuous further technical advances over time, in particular, due to the introduction of intubation for a prone position in the 1940s and the development of microsurgical techniques by Mahmut Gazi Yasargil (*1925) [3]. It is reported that in the Krayenbühl era in Zurich (1937–1973), about 250 lumbar disc surgeries were performed [3]. Yasargil reported his early experience on 105 patients that he treated in Zurich between 1967 and 1977. By use of the microscope, he could reduce the surgical trauma to skin, muscles, and lamina. Furthermore, “… identification of the dural sac, nerve root, radicular artery and epidural veins is facilitated by the operating microscope. Epidural veins may be controlled with bipolar coagulation and are discernable from radicular arteries…” [26].
The advent and introduction of CT (1971) and magnetic resonance imaging (1979) provided further support for the upsurge of disc surgery, which would be offered as therapeutic alternative earlier in the clinical course as the localization of the pathology became more accurate. It also provided the basis for imaging-based comprehensive classification systems of degenerative disc disease, such as the Modic classification for bone marrow edema [27] or the Pfirrmann classification (developed by Christian Pfirrmann and Norbert Boos in Zurich, Switzerland) to grade disc degeneration based on T2-weighted magnetic resonance images [28].
3. Spinal Deformity
One of the Swiss pioneers in the evaluation and conservative orthopedic treatment of spinal deformity is Wilhelm Schulthess (1855–1917). Born in Villnachern, he enrolled at the University of Zurich to study medicine and trained in internal medicine and pediatrics. In 1883 he opened a private orthopedic clinic in Zurich, together with his surgeon-friend August Lüning (1813–1896); in 1951 the clinic was renamed “Schulthess Klinik” in his honors. His scientific activity was almost exclusively dedicated to a profound study of spinal deformity, and he was appointed Professor at the University of Zurich in 1912 [29]. Among his many achievements, Schulthess developed a scoliosometer, which allowed for the accurate measurement of the spinal morphology in 3 dimensions – before the advent of X-ray. This masterpiece was an early predecessor of today’s whole spine X-ray analysis for the evaluation of spinal deformity.
4. Intradural and -Medullary Tumors
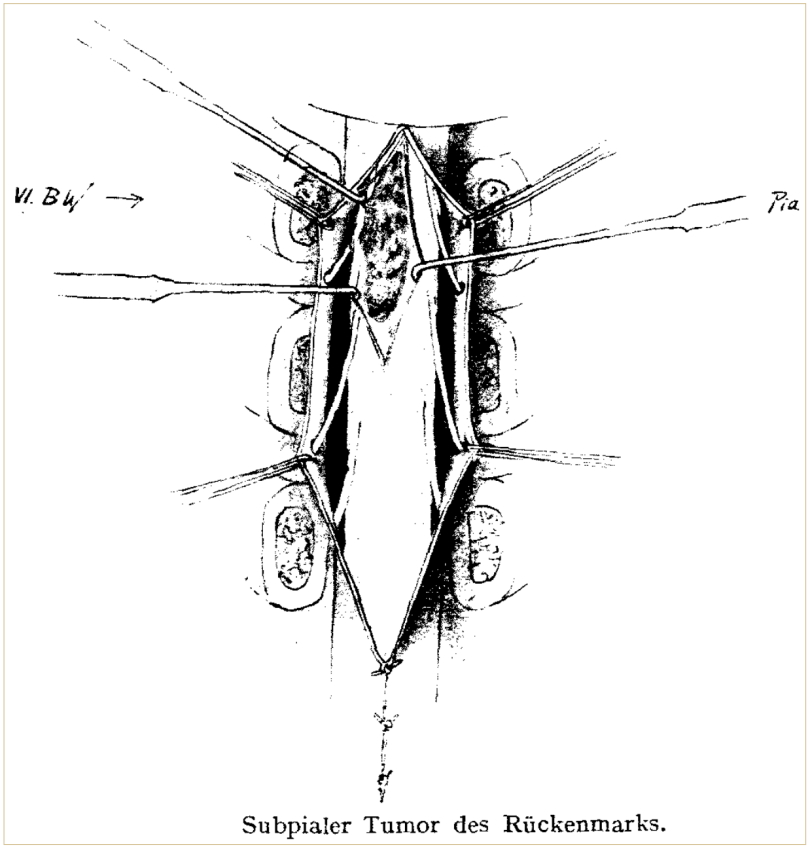
In Lucerne, the general surgeon Hans Brun was one of the first surgeons (together with Fedor Krause [1857–1937] in 1909 and Anton von Eiselsberg [1860–1939] in 1907) to remove a spinal intramedullary tumorous lesion in a 32-year-old railway employee with progressive signs of paraplegia [2,30]. On 15 February 1910, he chose a C3–4 laminectomy to explore and remove a 17-mm subpial lesion via median cordotomy that was later identified as tuberculoma. The lesion was localized by neurological examination (the preoperative workup was conducted together with the neurologist Otto Veraguth) and intraoperative palpation of the spinal cord. The patient experienced a significant recovery and returned to his preoperative occupation for about 3 years postoperative until dying of lung tuberculosis. Brun operated on 2 further patients with intramedullary spinal cord tumors; 1 with suspected diffuse glioma of T6–9 in September 1910 and 1 with multiple intramedullary tuberculomas of C6 in November 1913 and of C4 in December 1913 (Fig. 3) [31]. Details on these cases are provided in a recent historical review article [30]. Further reports of laminectomies for the removal of intradural tumors (e.g., meningioma) by Krayenbühl in Zurich date back to 1938 [3].
THE MODERN ERA
1. Academic Spine Care
With the progressive development of new instrumentation techniques, a wider range of therapeutic options became available to treat patients with various spinal diseases. Concepts of fusion originating from orthopedic surgery were combined with decompressive techniques of primarily neurosurgical background.
Arnaldo Benini (*1938) academically collaborated with Hugo Krayenbühl from Zurich, where he also was entitled as professor for Neurosurgery. He made a career as attending surgeon in the newly founded neurosurgical department of the Kantonsspital St. Gallen in 1970. His contributions to the anatomy and surgical treatment of lumbar spinal stenosis and spinal tumors are particularly known [32,33], but his expertise is known to be substantial for many other aspects of spine care, including the evaluation of syringomyelia and the infrequently applied technique of cordectomy.
In 1998, Jürgen Harms (*1944) and Dezsö J. Jeszenszky (*1954) described a unilateral, transforaminal approach to effectively decompress the nerves, and to conduct a lumbar interbody fusion without sacrifice of the contralateral joint complex (today known as transforaminal lumbar interbody fusion) [34]. One year after this publication, Dr. Jeszenszky moved to Switzerland and started to treat spine patients at the Kantonsspital St.Gallen (1999–2004) and at Schulthess Clinic (Zürich; since 2004) where he worked together with Dieter Grob (*1949). Both of their contributions to the biomechanics and treatment of the spine are manifold. During this time, quality control in spine surgery by the use of registries was promoted [35].
Norbert Boos (*1960) and Max Aebi (*1948) are 2 of the most academic and productive spine specialists in Switzerland. Norbert Boos studied in Germany and trained in orthopedic surgery in Berne, Switzerland. He then continued his educative journey to Iowa, Minnesota, Montréal, and Nottingham and worked as a spine surgeon at both the Balgrist and the University Hospital Zürich (USZ), Switzerland. In 2009 he went into private practice. The Swiss-Canadian Max Aebi from Berne underwent surgical and orthopedic training in Switzerland, England, Canada, the United States, and France. Among his achievements are the creation of academic orthopedic departments at the University of Berne & Montréal, the foundation of the European Spine Journal, of the AOSpine Foundation and of the Eurospine. Both, Norbert Boos and Max Aebi are coeditors of the textbook “Spinal Disorders – Fundamentals of Diagnosis and Treatment” that has become a standard reference in the field [36].
There are several further, dedicated, academically oriented clinicians and researchers with a focus on spine health in Switzerland. Exemplarily, we would like to point out the numerous scientific contributions of Anne F. Mannion (Schulthess Klinik, Zurich, Switzerland). She was fundamental in developing the Core Outcome Measures Index, a brief questionnaire that was accepted by the Eurospine as recommended patient-reported outcome measure, translated into all European languages [37].
2. Political Developments, Societies, and Programs
Over the years, neurosurgeons as well as orthopedic surgeons have increased their surgical activities in the field of spine care. To reduce the natural friction of both groups and despite the fact of progressive pressure of the health authorities, the Swiss Spine Society (https://www.spinesociety.ch/) was founded with the turn of the millennium. Members of the board committee are equally elected out of 2 mother societies, the Swiss Neurosurgical Society (https://www.swissneurosurgery.ch/), and the SwissOrthopaedics (http://www.swissorthopaedics.ch/), whereas the chair rotates every second year.
Regarding the progressive implementation of new technologies in spine surgery, with an associated potential increase in subsequent health care costs, the Swiss Spine Society was forced to establish a spine registry in 2006. In consequence, all interventions using interspinous devices, dynamic transpedicular devices, total disc replacement (TDR), or kyphoplasty had to be registered. Interestingly, the register was paid by the involved health technology companies. Over the years, the interest of health authorities decreased, and the quality of the data dropped. However, it was possible to publish the long-term results of cervical and lumbar TDR [38,39].
Swiss spine surgeons are active in research, and they maintain a lively exchange. This year the Swiss Neurosurgical Society will hold the 10th NeuroSpine meeting (https://neurospine2020.congress-imk.ch/). This meeting is specially dedicated to spine topics in the neurosurgical field. However, it encourages a strong interdisciplinary approach with colleagues from Orthopedic Surgery, Neurology, Rheumatology, Sports Medicine, and Anesthesiologists specialized in pain treatment.
To increase the clinical and academic horizon of junior neurosurgical colleagues and to foster networking, the ‘Swiss-Korean Exchange program’ was established [40]. It allows a fruitful exchange of surgeons between the 2 countries, which are characterized by many similarities but at the same time have very different histories and backgrounds. Hopefully this popular program can be continued despite the current concerns with the COVID-19 pandemic [41].
THE FUTURE
Today, spine surgery is performed to nearly equal parts in public and private institutions. There is a trend towards specialization for highly specialized intradural, as well as for complex revision and deformity surgery in the larger public and university hospitals. Training conditions become increasingly important, as caseloads during residency decrease as a result of working hour restrictions [42]. Great opportunities to deepen technical know-how outside the operating room are offered at high-quality spine surgery training courses organized by the AOSpine Swiss Council, the European Association of Neurosurgical Societies and—more locally—by the Swiss Young Neurosurgeons (SYNS; https://www.syns.ch).
To guarantee high quality of spine care for Swiss patients and to harmonize the future education and training of both neurosurgeons and surgeons with an orthopedic background after board-certification, a common interdisciplinary title confirming the specialization on spine surgery was created. It consists of an additional 3 years of training—exclusively in spine surgery—after the specialist title in neurosurgery or orthopedic surgery has been obtained. To increase the interdisciplinary exchange, a rotation into the sister department is mandatory. Recently, this innovative and interdisciplinary specialization in spine surgery was accepted by the government and shall start in 2021.
The development is paralleled by the formation of interdisciplinary spine units in the larger Swiss public and university hospitals, e.g., in Basel, Lausanne, Zurich, and St.Gallen, which are composed of both neuro- and orthopedic surgeons. A joint ortho-neuro program for challenging spine conditions is beneficial to both patients and care providers [43].
CONCLUSION
In summary, there is a long history and tradition in Swiss spine surgery. To list the many important personalities in the development of spine surgery in all parts of Switzerland—especially within the last decades—goes beyond the scope of this work. Accordingly, only a small and selected overview could be created. Recent developments aim at increasing training conditions with the ultimate aim of improving the quality of care in spine surgery. To archive this goal, Swiss spine surgeons recently joined efforts to strengthen the collaboration between and training of neuro- and orthopedic surgeons.
Notes
The authors have nothing to disclose.