Inside-Out Approach of Lumbar Endoscopic Unilateral Laminotomy for Bilateral Decompression: A Detailed Technical Description, Rationale and Outcomes
Article information
Abstract
Although lumbar stenosis was recognized as a contraindication for endoscopic spine surgery in the past, the advancement in endoscopic system design and development of approach techniques and strategies now enabled the endoscopic spine surgeons to manage all types of lumbar stenosis safely and more effectively. A full-endoscopic lumbar technique for surgical management of spinal canal stenosis is now used today in many advanced spine centers around the world as one of their standard procedures which can be done under general, regional, local anesthesia with sedation. In this technical report, we described in detail the inside-out approach of performing lumbar endoscopic unilateral laminotomy with bilateral decompression (LE-ULBD) and retrospectively reviewed hospital records of 127 patients who underwent the approach from December 2018 to March 2019 to address 1 level lumbar spinal stenosis and determined its outcome after 12-month follow-up period. Perioperative outcomes, operation time, length of hospital stay, and surgical complications were recorded and analyzed. The cross-sectional area of the thecal sac at the operated level was measured. The visual analogue scale (VAS) was assessed preoperatively, 1 month, and 12 months as well as the Oswestry Disability Index (ODI). The data were statistically analyzed (using SPSS ver. 17.0). The inside-out approach LE-ULBD was shown to effect statistically significant improvement in the VAS of leg and back pain as well as the ODI. It is a familiar, safe, and effective way of performing spinal stenosis decompression with good reproducible outcomes.
INTRODUCTION
Population ageing is a global phenomenon. Virtually every country in the world is experiencing growth in both the size and the proportion of older persons in the population [1]. The incidence of degenerative spine disease, specifically lumbar spinal stenosis is also expected to increase with the ageing population. Degenerative changes of spine structures including facet joints, intervertebral discs, ligamentum flavum can lead to spinal narrowing (stenosis) that can compress neural structures producing pain in the legs and back as well as impaired ambulation and other disabilities and is the most common indications of spinal surgery in old age [2-6]. Surgical intervention may be necessary to decompress the stenosis depending on its severity after conservative management has failed.
Surgical decompression had shown statistically significant improvements in postoperative functional outcome and quality of life, compared with conservative medical treatment in the management of symptomatic lumbar stenosis, even in the long term [7]. The gold standard [8] surgical treatment for symptomatic lumbar stenosis is facet sparing laminectomy decompression requiring removal of the spinous process and lamina, detaching the posterior musculo-ligamentous complex. The damage to the posterior supporting structures is unavoidable in this procedure leading to long-term consequences. Muscle detachment and dissection may cause muscle weakness and denervation during the procedure, finally followed by atrophy, this is linked to an increase in the prevalence of post-spine surgery syndrome and chronic low back pain [9]. Also, wide removal of facet joints results in segmental instability, a long recovery time, and rehabilitation [10-12] for which some may even require fusion surgery [13]. To lessen iatrogenic injury to normal anatomic structures not directly involved in compression syndromes and to avoid the long term consequences of such, more minimal invasive techniques were introduced. Getty et al. [14] in 1981 introduced the partial undercutting facetectomy technique. Young et al. [15] in 1988 presented multilevel subarticular fenestration technique as an alternative to wide laminectomy and Poletti [16] i n 1995 reported on successful outcome of 2 cases where he performed unilateral laminotomy for bilateral ligamentectomy. It was however Spetzger et al. [17] in 1997 who made the cadaveric study of the anatomic and surgical considerations of unilateral laminotomy for bilateral decompression of lumbar spinal stenosis and published their clinical experience (n = 27) for which they reported a 93% favorable outcome. Oertel et al. [18] in 2006 reported that 92.2% of their patients remained improved on their long-term postoperative results 5.6 years (4–10 years) of ULBD experience. The clinical outcomes of these procedures were comparable with open facet sparing laminectomy decompression [19]. While using the parent technique of ULBD, procedures involving tubular retractors coupled with microscope or endoscope (microendoscopic decompression) were reported in literature that showed the same benefits of open laminectomy. There were high patient satisfaction and favorable functional outcomes while preserving the normal support structures of the lumbar spine resulting low incidence of spinal instability and reoperation rates. Furthermore, functional improvement was similar even in patients with preoperative spondylolisthesis [20,21].
Over the last 3 decades, with the surgical trend favoring more minimal invasive procedures, a full uniportal endoscopic spine surgery has evolved. It was initially utilized to manage soft disc herniation through a standardized transforaminal, interlaminar, anterior cervical transdiscal, and posterior cervical approaches [22,23]. The favorable clinical outcomes of full-endoscopic spine surgery were validated by many studies [23-26] showing comparable outcomes with open and microscopic surgical techniques to the spine with lower complication rates, less blood loss, and shorter hospital stay. Although lumbar stenosis was recognized as a contraindication for endoscopic spine surgery in the past, the advancement in endoscopic system design and development of approach techniques and strategies now enabled the endoscopic spine surgeons to manage all types of lumbar stenosis safely and more effectively [25]. The full-endoscopic lumbar technique for operating spinal canal stenosis is used today as a largely standard procedure and allows sufficient decompression [26].
In this study, we described in detail the inside-out approach of performing lumbar endoscopic unilateral laminotomy with bilateral decompression (LE-ULBD), one of the ways of performing percutaneous stenoscopic lumbar decompression (PSLD) [27], to address 1 level lumbar spinal stenosis and determined its outcome after 12-month follow-up period.
MATERIALS AND METHODS
1. Patient Population
The study retrospectively analyzed data of 127 patients with lumbar stenosis who underwent bilateral decompression, LE-ULBD using inside-out approach, performed by a single surgeon, at Good Doctor Teun Teun Hospital, Anyang, Korea, between December 2018 to March 2019.
The study protocol followed the research guidelines of the Good Doctor Teun Teun Spine Hospital ethics committee and was approved by the Institutional Review Board (IRB No. 2019-W04). All patients involved in the study have provided written informed consent and their patients’ and data privacy rights were protected.
The demographics, mean age, sex, operation time, length of hospital stay, and complications were recorded through review of medical records. Magnetic resonance imaging was done preoperatively as well as within 24 hours postoperative for all patients to demonstrate any immediate complications were also reviewed. The cross-sectional area of the thecal sac at the operated level was measured preoperative and postoperatively and recorded. Perioperative outcomes such as operation time, length of hospital stay, and incidence of surgical complications were recorded and analyzed.
2. Outcome Measures and Statistical Analysis
The visual analogue scale (VAS) was assessed by questionnaire preoperatively, 1 month, and 12 months after surgery as was the Oswestry Disability Index (ODI) and these were recorded and analyzed. Simple mean and standard deviation were used to describe the changes between preoperative and postoperative status. SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) was utilized for statistical analysis.
INDICATION
LE-ULBD is indicated for decompression of symptomatic lumbar central and lateral recess stenosis which is mostly due to degenerative changes in older individuals. Central canal and lateral recess stenosis may result from a decrease in the anteroposterior, transverse or combined diameter secondary to loss of disc height with or without bulging of the intervertebral disc or development of discal cyst, hypertrophy of the facet joints, development of facet cyst, hypertrophy of the ligamentum flavum, vertebral endplate osteophytosis, presence of grade 1 spondylolisthesis, or any combination of these. Careful investigation and clinicoradiologic correlation are required since even severe anatomical/radiologic spinal stenosis may be present in asymptomatic patients. In this study, patients with symptoms of back pain, neurogenic claudication with or without radiculopathy referable to the lumbar stenosis for at least 6 weeks who failed conservative treatment and with an magnetic resonance imaging (MRI) evidence of 1 level central with or without lateral recess stenosis who were treated by LE-ULBD using inside-out approach and completed a 12-month follow-up visit were included in the study. Patients with foraminal stenosis, multiple level stenosis, significant instability, those with a history of previous lumbar spine surgery, and those with degenerative spondylolisthesis grade 2 and above were excluded.
SURGICAL PROCEDURE OF INSIDE-OUT APPROACH LE-ULBD
1. Preoperative Planning
All pertinent information about the surgical patient must be considered in order to achieve a favorable outcome. The existence of comorbid conditions is common in the older population and must be extracted during the history taking and medical evaluation and surgical clearance. Careful neurologic examination and clinic-radiologic correlation will identify the symptom causing pathologic level. This is particularly important since most spine imaging studies in this age group can reveal many degenerative conditions that identifying the cause of the patient’s symptoms can be problematic.
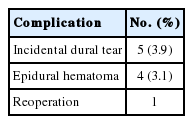
Aside from the MRI, all patients in the study were required to undergo a computed tomography (CT) scan before and after the procedure. CT scan investigation before operation can provide important information on the morphology of facet joints and spinous processes, lamina, and disc. Usually, the more symptomatic side determines the side of approach, however, it can be altered depending on the information from CT scan. An ipsilateral approach with 9.5-mm working sleeve would be chosen for wide lamina width (size> 10 mm) with normal facet joint (Fig. 1A, B). In case of hypertrophic, rotated spinous process (Fig. 1C), or more sagittal oriented (higher lumbar levels) and hypertrophic facet joints, and narrow lamina width, or hypertrophic, rotated spinous process (Fig. 1D), contralateral insideout approach is recommended to save facet joint (Fig. 1E).
(A) Preoperative computed tomography scan shows normal size of laminar. (B) Postoperative computed tomography scan shows decompression of ipsilateral approach without damage of facet joint. Contralateral approach is recommended in case of (C) vertebral rotation, (D) the width of laminar space is narrow. (E) Postoperative computed tomography scan shows decompression of spinal canal without damage of facet joint after contralateral approach procedures.
2. Use of Fluoroscopic Guidance
In the inside-out approach, there was no need to check anteroposterior fluoroscopic view because the palpation of the spinous process was enough to guide the surgeon orientation. Only the lateral C-arm view confirmation is required during the whole surgery to reduce the operative time and radiation exposure. The C-arm Machine was fixed on the lateral orientation and was included in the surgical sterile drapes.
3. Skin Entry Point and Landing Site
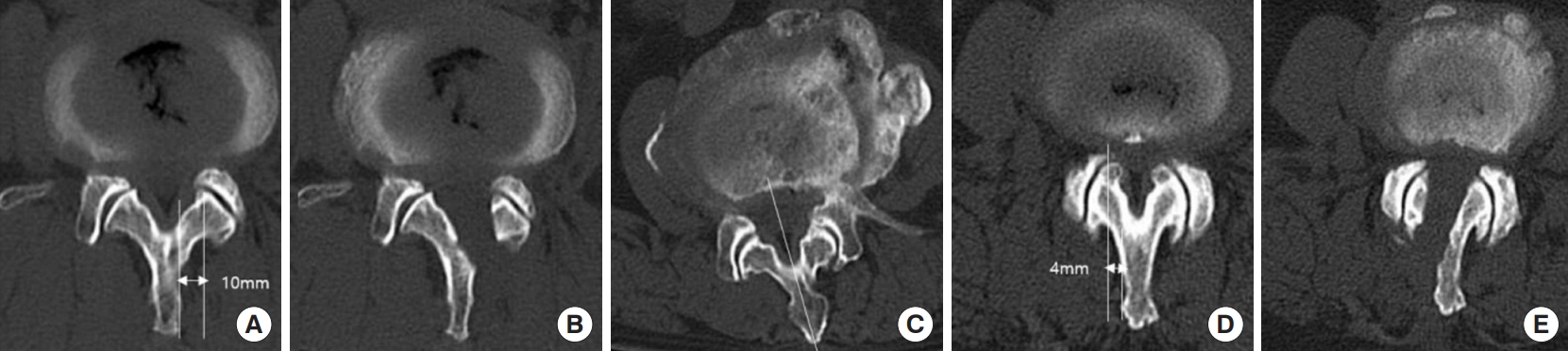
The surgery was performed in a standardized manner under epidural anesthesia with mask sedation in the prone-flexed position on a Wilson frame. The location of the skin incision was confirmed by the fluoroscopy and a 7-mm vertical skin incision was made over the fatty plane between the spinous process and multifidus muscle (Figs. 2-4) directly above the lamina of interest (Fig. 2A). Through this incision and fatty plane, an 8-mm dilator was applied to land on top of the cranial hemilamina at the spinolaminar junction.
(A) Incision of skin should be made just beside spinous process to save facet joint. (B–D) Skin incision with #10 surgical blade. A 7-mm skin incision (dotted line) enables the passage of 8-mm dilator and 9.5-mm working sleeve due to skin elasticity (solid line = spinous process). Skin marking or incision is placed directly above the lamina based on anteroposterior C-Arm x-ray projection.
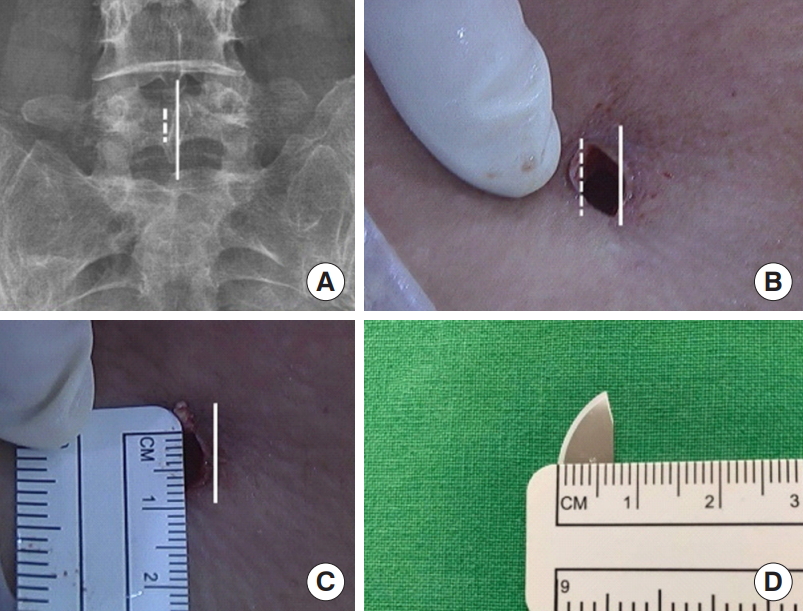
The entry point of approach is through the fatty plane, between spinous process and multifidus muscle. (A) Preoperative magnetic resonance imaging (MRI). (B) Postoperative MRI. The unique surgical approach may further limit muscle injury that could lead to less surgical site pain postoperatively.
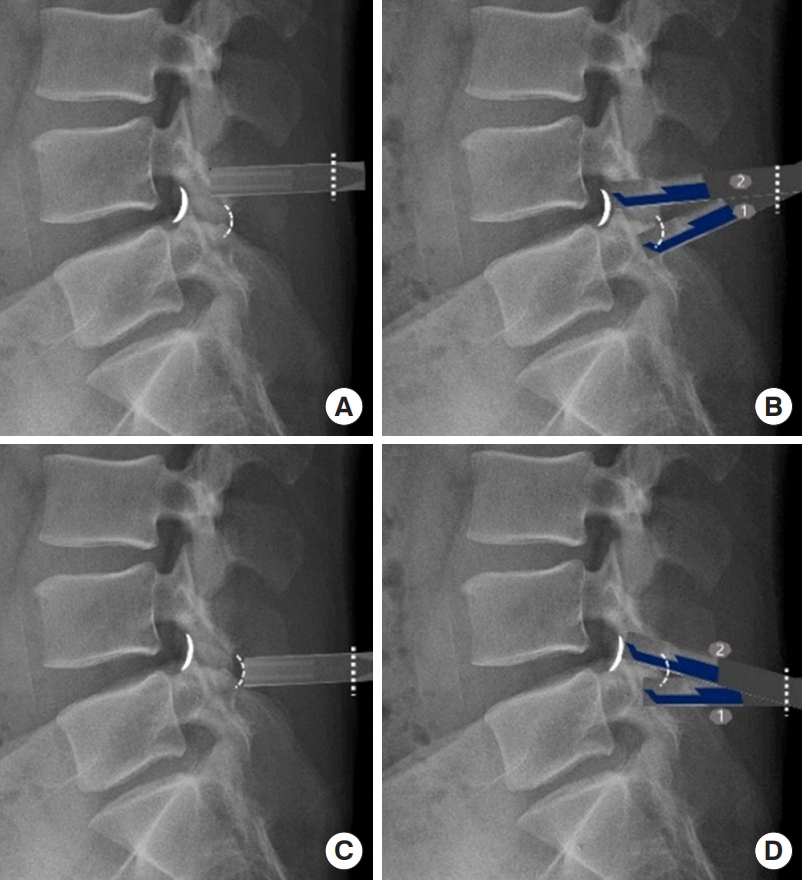
Lateral x-ray views comparing skin incision and landing on the lamina (A, B) and interlaminar space (C, D). (A, B) The inside-out approach landing point is on the L4 lamina. The lamina is represented by a solid curved line and ligament flavum (interlaminar space) by a curved dotted line. The straight dotted line denotes the skin incision. ① starting point of laminectomy, ② endpoint of laminectomy. The landing point of instruments on the lamina will facilitate laminotomy (of cranial lamina) and access directly to the spinal canal at the disc level of interest.
A 9.5-mm outer diameter working sleeve was applied over the dilator which was subsequently removed once the sleeve was docked on the inferior border of the cranial hemilamina, A STENOSCOPE [28] (Techord, Daejeon, Korea), with a 8.4-mm outer diameter, 5.7-mm working channel, 120-mm working length and 12° angle optical lens endoscope was introduced into the working sleeve to start the endoscopic stage while on continuous saline irrigation using pump irrigation at 30–60 mmHg pressure.
4. Bone Work and Decompression
Ipsilateral small laminectomy to expose the ligament flavum is the first step in the inside-out approach. The partial laminectomy using a combination of endoscopic Kerrison punch and drill starts at the inferior border of the cranial hemilamina at the spinolaminar junction going cranially until the ligamentum flavum is detached showing a small area of epidural space. Identification of the uppermost attachment of the ligamentum flavum provides an important landmark to confirm the cranial limit of the decompression. An epidural space is created among the laminotomy area, ligamentum flavum, and the spinal dura with the help of the saline irrigation pressure which can avert iatrogenic dural injury. Medial laminotomy and early piecemeal removal of the detached ligamentum flavum border should reveal the spinal canal and the spinal dura which can be followed laterally to guide the surgeon in preforming medial facetectomy keeping within the border of the attachment of the ligamentum flavum to visualize the lateral margin of the ipsilateral traversing nerve root (Fig. 5). Early exposure of the lateral margin of the traversing nerve root (inside-out approach) may reduce nerve damage and may prevent undue facetectomy. It allows surgeon to find and protect the neural structure early in the procedure and bony decompression can be done just enough to decompress the nerve root (Fig. 6A). The contralateral decompression was done after decompression of the ipsilateral traversing nerve root was satisfactory. This was done by undercutting the base of the spinous process and the contralateral lamina using a high-speed drill and Kerrison punches until the small detachment of the cranial contralateral ligamentum flavum. Once the water pressure created a window to make the epidural fat and neural structures visible, careful piecemeal flavectomy was resumed (Fig. 6B). The importance of visually protecting the neural structures was emphasized in this technique. Use of punches more than drills were employed also in the contralateral decompression. After clearing the thickened flavum, the contralateral superior articular process (SAP) was visualized. Blunt dissectors were used to carefully probe the SAP and detach adhesions between the dura and ligamentum flavum, only then was the resection/decompression of the contralateral SAP started, which was again, under direct visualization by manipulating the endoscope to maximize the angle of sight. Extra care was required with decompression/flavectomy especially in the midline and the resection of SAP of the contralateral side due to adhesion between dura and ligament flavum (Fig. 6C) which can cause dural tear. Disc decompression and annuloplasty were done as necessary.
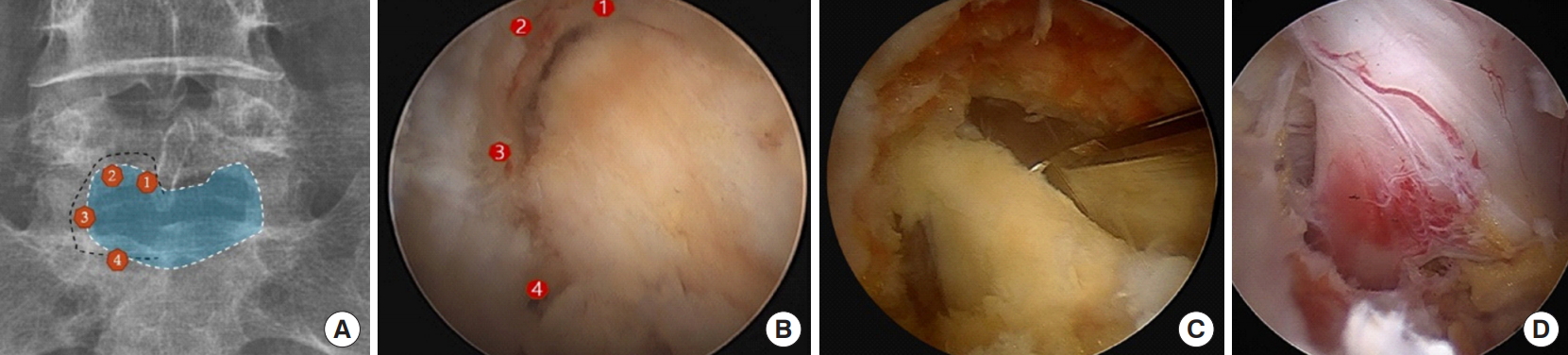
(A) The process of laminotomy: ① starting point of laminotomy at the spinolaminar junction, ④ caudal lamina= endpoint of laminotomy. (B) The procedure of piecemeal flavectomy (removal of the ligament flavum) follows the same pattern or sequence ① through ④, (C) Early splitting or removal of the ligamentum flavum for early direct access into the spinal canal, to visualize the lateral margin of spinal root. (D) Decompression of traversing root.
5. Procedural Endpoint
The endpoint of the procedure was reached when the dura and bilateral traversing spinal nerve root were free and pulsating. Careful hemostasis was performed by first turning off the irrigation pressure intermittently to identify bleeding points and these were controlled accordingly using endoscopic radiofrequency bipolar. A small closed suction drain was applied in all cases. All patients underwent a lumbosacral MRI, within 24 hours after surgery to identify immediate postoperative complications and to evaluate the change of cross-sectional area pre- and postoperatively. Pre- and postoperative cross-sectional area was measured by the PACS (picture archiving and communication system) software INFFINITE Healthcare Co. (Seoul, Korea) on axial view of MRI scan at the mid-disc level.
RESULTS
Table 1 summarizes the demographic data of patients included in the study including the percentage of each spinal level involved. The age distribution ranged from 49 to 83 years with a mean age of 69.2 years. We observed a male predominance, there were 72 male (56.7%) and 55 female consecutive patients (43.3%) who qualified for inclusion in this study. The operative levels ranged from L1–2 to L5–S1, where L4–5 level is the most commonly operated level (n = 55, 43.3%) followed by L5–S1 level (n = 50, 39.37%) (Table 1). The L4–S1 operated levels account for 82.67% of all levels involved in the study.
1. Peri- and Postoperative Outcomes
The mean operating time was 37.3 ± 23.15 minutes for bilateral decompression of 1-level lumbar stenosis. The mean hospital stay was 1.38 ± 2.5 days. The patients’ symptoms improved starting from the immediate postoperative period.
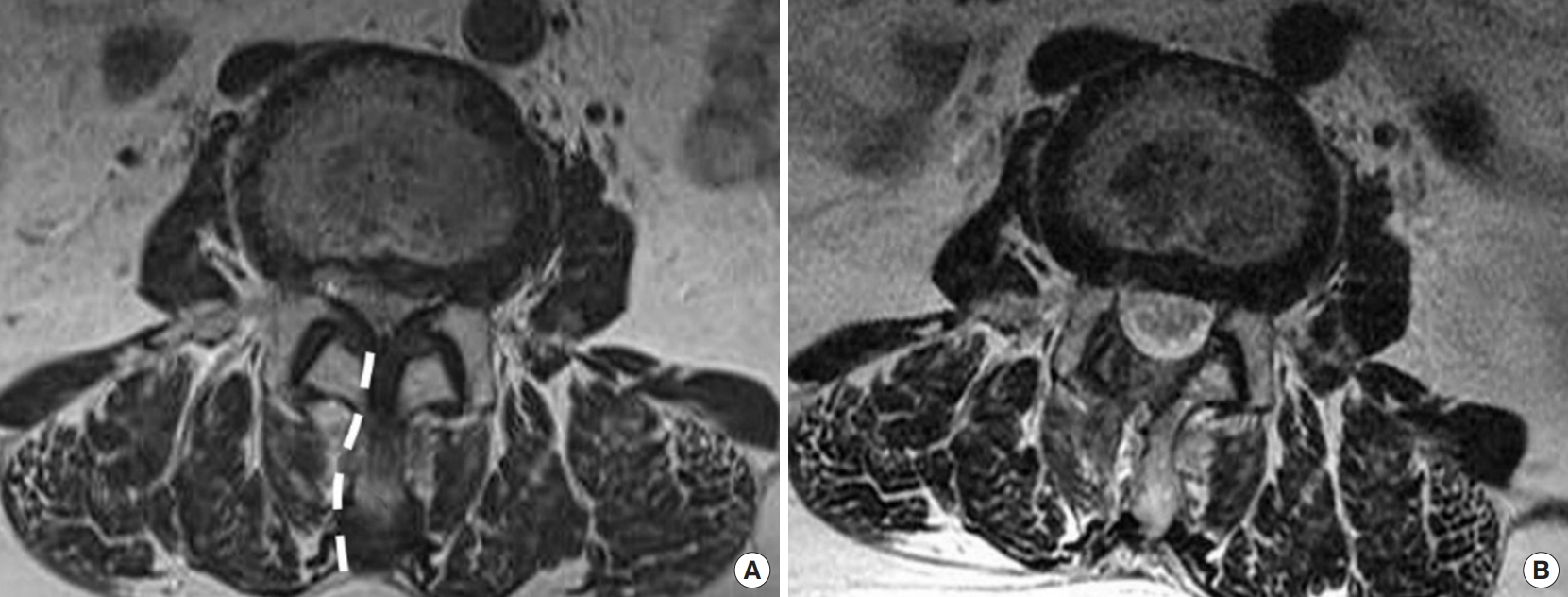
Postoperative MRI showed a statistically significant increase in the cross-sectional area and there was no injury of multifidus muscle, facet joint on postoperative MRI (Fig. 7, Table 2).
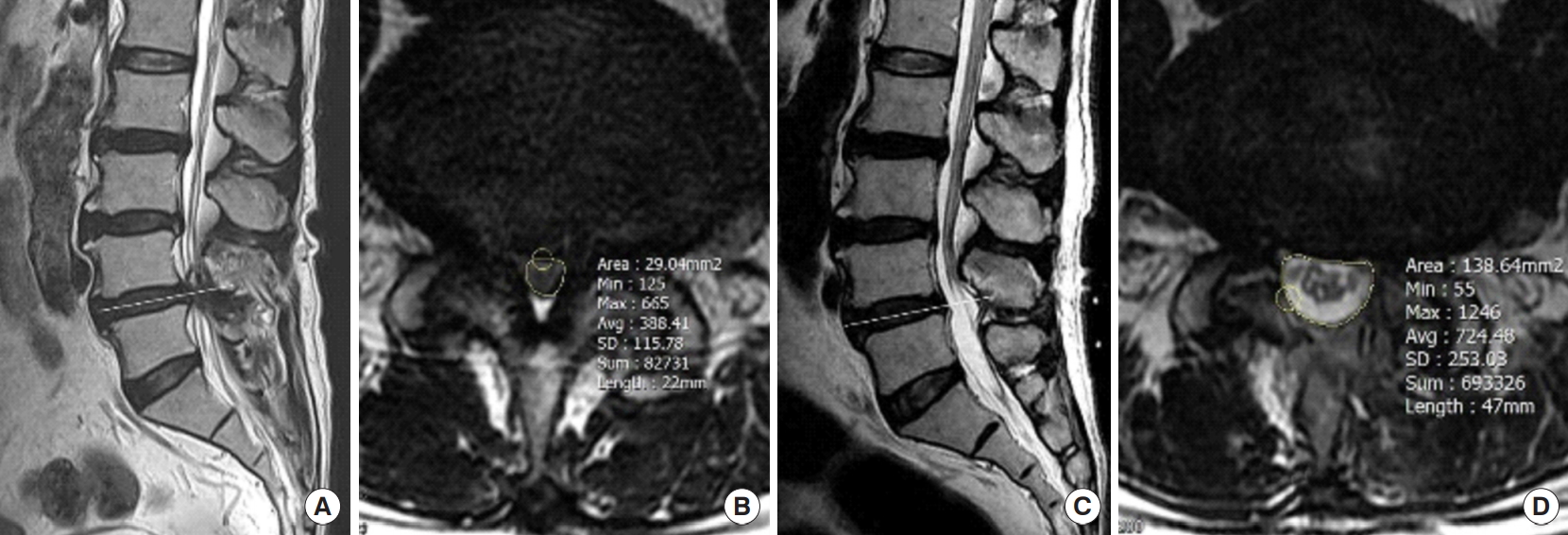
Representative case: the cross-sectional area of the spinal canal in preoperative magnetic resonance imaging (MRI) (A, B) and postoperative MRI (C, D) at middle disc level (solid line at L45) showed significant enlargement.
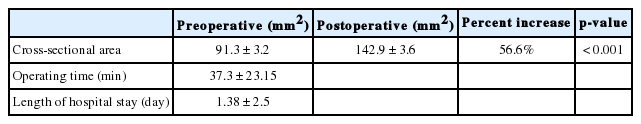
Pre- and postoperative changes in cross-sectional area at the middle disc level with the mean±standard deviation of the length of operating time and hospital stay
The VAS back and leg pain decreased from 6.70 ± 2.40 to 2.51 ± 3.38 and 7.05 ± 2.61 to 2.34 ± 7.12 respectively and the ODI improved by 35.1 scores 12 months after the surgery. The clinical data shows a statistically significant improvement in VAS of back pain and leg pain during their follow-up (p < 0.001). The mean ODI value shows considerable improvement also (p < 0.001) (Table 3).
2. Surgical Complications and Reoperation
We observed 9 surgical related complications (7.1%). The most common is incidental dural tear which happened in 3.9% (n = 5) of cases followed by epidural hematoma in 3.1% (n = 4) for which 1 case required endoscopic evacuation (Table 4).
There was no case of significant neurologic deficit from nerve root injury and there was no intraoperative seizure nor a postoperative headache related to continuous water irrigation noted. There was no a case of postoperative infection.
DISCUSSION
Many studies have reported on comparable short and long-term favorable clinical outcomes between open facet sparing laminectomy and minimally invasive ULBD in lumbar central and lateral recess stenosis [29-31]. The benefit extends even to lumbar stenosis cases with spondylolisthesis [32]. Additionally, there are also several studies describing similar favorable results between microsurgical or tubular techniques of ULBD and endoscopic lumbar decompression in the setting of lumbar stenosis, with shorter hospital stay and less collateral tissue injury [33,34]. It may be reasonable to infer from these reports that endoscopic stenosis decompression can also deliver adequate decompression comparable to ULBD and open laminectomy.
1. Rationale of the Inside-Out Approach
There are 2 approaches of performing endoscopic decompression of stenosis, one is the inside-out approach LE-ULBD or PSLD [27] which can address single or multiple level central and lateral stenosis with one incision. The other one is paraspinal approach (Para-PSLD) [28] which is a solution for foraminal and extraforaminal lesions. The term inside-out approach LE-ULBD can also be considered a translaminar approach in this study. Translaminar endoscopic approach was first described by De Antoni et al. [35]. In inside-out LE-ULBD, access to the spinal canal was via the laminotomy of the cranial medial hemilamina and not through the interlaminar area. The main principle behind this approach was early access to the spinal canal, visualization and protection of ipsilateral dura and traversing spinal root, using the visualized edges of the ipsilateral traversing root as a guide and gauge for bone resection and decompression especially of the medial facet. The ligamentum flavum is resected piecemeal and no effort is made to remove it en bloc. The contralateral decompression and endpoints are similar with other endoscopic stenosis decompression surgery techniques. Table 5 summarized the key points and rationale of the insideout approach.
The risk of significant ionizing radiation exposure is a real concern for patients, surgeons, and operating room staff during spine surgery [36]. This is especially true in endoscopic spine surgery [37] where exact placement of instruments into targeted landing points requires fluoroscopic guidance. This was highly considered in inside-out procedure. To mitigate this risk, we decided to use only lateral projection views aside from using general strategies in reducing radiation exposure. Familiarization of lateral spine radiologic anatomy is part of learning inside-out approach. With this strategy, we believe that we were also able to minimize operation time aside from lowering radiation exposure.
The mean (standard deviation) operation time in this study was 37.3 ± 23.25 minutes. This was in the lower border of the endoscopic stenosis decompression times per level of 68.9 ± 10.0 minutes as reported by Huang et al. [38], of 67.65 minutes by Lee et al. [25] and a meta-analysis by Lee et al. [25] reported a mean operation time ranging 68.9 to 122.5 minutes. The factors that may be able to account for the shorter mean operation time in our study were: (1) Inside-out approach utilized the endoscopic Kerison for bone resection more than the endoscopic drill resulting to faster decompression; (2) The 5.7-mm working channel of the stenoscope can fit bigger sizes of endoscopic Kerrison punches; (3) Limiting fluoroscopy to lateral projection only; and (4) In using the visualized edges of the ipsilateral traversing root as a guide and gauge for bone resection may lessen time doing unnecessary bone work. The short length of hospital stay reflects the unique ability of most endoscopic spine procedures for early recovery and discharge.
The study showed statistically significant improvement ODI and VAS pain scores for leg and back pain postoperatively compared to that before surgery. These were a constant finding in published literature after endoscopic stenosis decompression either for PSLD [27] or any endoscopic decompressive techniques.
The discussion about complications in endoscopic spine surgery is an integral part of the informed consent before the procedure. The general rate of complications in endoscopic spine surgery was reported to be within the range of 2.9% to 13.75%. Dura injuries occur in literature with rates ranging from 0% to around 5%, and nerve injuries occur at rates from 0% to around 2.5% [26]. Sairyo et al. [39] reported their single center experience of 138 patients, their incidence of surgery related complications was 8.6%. In our study, we observed 9 surgical related complications (7.1%), 5 cases of incidental dural tear 3.9%, and 4 cases of epidural hematoma (3.1%). The incidental dural tear was all observed durotomies. The dural injuries were noted when performing the resection of ligament flavum at the midline and under the contralateral SAP due to presence of adhesion between dura and ligament flavum. Incidental dural tear is a common complication of general spine surgery. It can present as cerebrospinal fluid leaks, wound infections, epidural hematoma, and pseudomeningocele and can impact negatively on the outcome [40]. However it has a low incidence in endoscopic decompression. Lim et al. [27] reported 1.9% (7 of 450 cases). They were managed accordingly with double layer TachoSil, haemostatic dura-sealant packing [28]. With this method, no reoperation was required for management of cerebrospinal fluid leak or root herniation. The 4 cases epidural hematoma were noted on the postoperative MRI and were followed clinically. Three cases were asymptomatic and improved clinically despite the MRI finding of epidural hematoma in the postoperative site. One patient with epidural hematoma complained of severe back and leg pain and weakness of dorsiflexion of left foot which all resolved after endoscopic evacuation of the epidural hematoma. Epidural hematoma can happen during any spine surgical procedure and can cause compression and irritation symptoms in postoperative patients and can have dire consequences. To prevent this, we require bleeding parameter study and review and we always inquire for a history of anticoagulant intake prior to scheduling for surgery. Vigilant hemostasis intraoperatively must be a standard and careful inspection of the raw bone edges and epidural space must be done under low irrigation pressure prior to ending PSLD. We routinely applied Fr. 7 closed suction drain to postoperative site for 12 hours.
This study has some limitations. It is a retrospective study with a small number of patients and relatively short follow-up period. Secondly, there was no control group. It may merit to compare the clinical and radiological results between endoscopic and microscopic decompression. Fourth, this study was limited to patients undergoing single-level stenosis the results may be different from the results of multilevel stenosis.
CONCLUSION
This study demonstrated that inside-out approach LE-ULBD can provide adequate decompression evident on the statistically significant increase in the cross-sectional area of spinal canal postoperatively, with minimum bone work in the setting of central and lateral recess lumbar spinal stenosis without leading to serious complications during operation. The increase in the spinal canal diameter was translated to a statistically significant improvement in the ODI and VAS pain scores of back and leg of the study population and these improvements were maintained throughout the 1-year follow-up period.
Early small ipsilateral laminectomy to enter the epidural space, splitting and piecemeal resection of ligament flavum (inside-out approach), visualization and protection of the ipsilateral root before full bone and ligamentum flavum removal is a safe and effective way of performing spinal stenosis decompression with good reproducible outcomes.
Notes
The authors have nothing to disclose.
SUPPLEMENTARY MATERIALS
Supplementary video clip 1 can be found via https://doi.org/10.14245/ns.2040196.098.v.1.