Effects of Body Mass Index on Perioperative Outcomes in Patients Undergoing Anterior Cervical Discectomy and Fusion Surgery
Article information
Abstract
Objective
Obesity has become a public health crisis and continues to be on the rise. An elevated body mass index has been linked to higher rates of spinal degenerative disease requiring surgical intervention. Limited studies exist that evaluate the effects of obesity on perioperative complications in patients undergoing anterior cervical discectomy and fusion (ACDF). Our study aims to determine the incidence of obesity in the ACDF population and the effects it may have on postoperative inpatient complications.
Methods
The National Inpatient Sample was evaluated from 2004 to 2014 and discharges with International Classification of Diseases procedure codes indicating ACDF were identified. This cohort was stratified into patients with diagnosis codes indicating obesity. Separate univariable followed by multivariable logistic regression analysis were performed for the likelihood of perioperative inpatient outcomes among the patients with obesity.
Results
From 2004 to 2014, estimated 1,212,475 ACDFs were identified in which 9.2% of the patients were obese. The incidence of obesity amongst ACDF patients has risen dramatically during those years from 5.8% to 13.4%. Obese ACDF patients had higher inpatient likelihood of dysphagia, neurological, respiratory, and hematologic complications as well as pulmonary emboli, and intraoperative durotomy.
Conclusion
Obesity is a well-established modifiable comorbidity that leads to increased perioperative complications in various surgical specialties. We present one of the largest retrospective analyses evaluating the effects of obesity on inpatient complications following ACDF. Our data suggest that the number of obese patients undergoing ACDF is steadily increasing and had a higher inpatient likelihood of developing perioperative complications.
INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) is an effective surgical intervention often used to treat degenerative cervical spine pathology when more conservative methods fail to relieve symptoms [1,2]. During ACDF, an adequate tissue retraction of the longus colli muscles, esophagus, and trachea is required to expose the anterior cervical column. Thus, operating on obese patients with a thick subcutaneous layer and a large corridor to the spine can increase the difficulty of manipulating the tissue. More aggressive and prolonged tissue retraction may be needed, consequently leading to local edema, tissue ischemia, prolonged operative time, and increased blood loss [3-5].
Epidemiological literature has shown that patients with high body mass index (BMI) are amongst the most common populations to develop spine pathology [6-8]. However, studies present mixed results on the impact of obesity on ACDF surgical outcomes. Some have documented that obesity has no effect on patient-reported outcomes [9], complication rates [10,11], and postoperative narcotics requirements following ACDF. Conversely, others report that obesity is associated with longer operative times [3], increased blood loss [3], higher mortality [3,10], longer length of stay [12], worse patient-reported outcomes [5], and higher complication rates [3,12]. Overall, evidence suggests that obesity may not limit the benefit of surgical intervention; although, it may contribute to an increased risk of postoperative complications. These risks have not been thoroughly explored in the literature, with few studies analyzing the impact of obesity on the incidence of common inpatient complications following ACDF procedures.
An increased understanding of the effects of obesity on inpatient complications following ACDF would allow for improved patient selection and counseling and may ultimately lead to the circumvention of preventable perioperative complications. Our study aims to determine the incidence of obesity in the ACDF population and the effects it may have on postoperative inpatient complications.
MATERIALS AND METHODS
1. Data Collection and Associated Indices
The Nationwide Inpatient Sample (NIS) is the largest publicly available, all-payer, inpatient health care database in the United States (US) and is developed by the Healthcare Cost and Utilization Project (HCUP). The database contains a random subsample of 20% of US inpatient hospital records that represent an estimated 35 million annual discharges. The Elixhauser readmission and mortality indices are validated scoring systems that identify variables in the NIS correlated with overall patient health, mortality risk, and 30-day readmission risk [13,14]. The STROBE (Strengthening The Reporting of OBservational Studies in Epidemiology) statement was implemented for this manuscript. Institutional Review Board and patient consent were not required due to the study type.
2. Definition of Cases
The NIS was evaluated from 2004 to 2014 and discharges with International Classification of Diseases (ICD-9-CM) procedure codes indicating ACDF were identified (ICD-9-CM 80.51 and 81.02). This cohort was further stratified into patients with ICD9-CM diagnosis codes indicating obesity (278.0×), defined as a BMI of > 30.0kg/m2. Parameters including age, sex, frailty, obesity, weekend admission status, patient income, race, Elixhauser mortality/readmission indices, intraoperative monitoring, and number of fused levels were obtained and analyzed. Frailty, as defined in previous works, refers to patients with inpatient hypoalbuminemia and muscle weakness/fatigue [15]. Patients with diagnosis of infection, inflammatory spondyloarthropathies, neoplasm, pathologic or traumatic fractures, history of trauma, or pregnancy were excluded from the study.
3. Statistical Methods
Aggregate national estimates of yearly discharge frequencies were calculated utilizing weighted observations supplied by HCUP. For the years 2004–2011 and 2012–2014 the adjusted weights (TRENDWT) and normal weights (DISCWT) were utilized, respectively, to adjust for temporal database changes. Statistical analysis was performed with SAS 9.4 (SAS Institute Inc., Cary, NC, USA) utilizing the SURVEYMEANS, SURVEYLOGISTIC, SURVEYFREQ and SUVERYREG procedures that account for NIS stratified-cluster sampling methodology. NIS sampling is clustered by hospital identification (HOSPID) for all years and stratified by hospital region or hospital division for the years 2004–2011 and 2012–2014, respectively.
The normality of continuous variables was assessed graphically and statistically. Continuous variables with yearly nonparametric distributions were represented as yearly weighted median estimates; whereas, those with yearly normal distributions were represented as yearly weighted mean estimates. Comparisons of means/distributions of normally continuous variables were carried out using least squared means analysis; while, nonparametric distributions were compared with a modern extension of the Wilcoxon rank-sum test that adjusts for clustering, stratification, and weights [16]. Categorical variables were presented as an estimated weighted frequency and percent. Statistical analyses of categorical variables were carried out using chi-square and Fisher exact with the Monte Carlo simulation tests, as appropriate [17].
Time trend series plots were created for the yearly incidence of ACDF-obesity patients. To yield a quantitative measurement of yearly distribution trends, yearly means/medians of continuous variables were assessed with univariable logistic regression, with year assessed separately as either a categorical or continuous variable. Separate univariable followed by multivariable logistic regression analysis were performed for the likelihood of the following dependent inpatient outcomes: inpatient mortality, neurological deficit, dysphagia, cardiac, respiratory, hematologic, gastrointestinal, or genitourinary complications, pulmonary embolus, wound infection, hardware failure, or durotomy. All available NIS hospital, patient, Elixhauser, and economic variables were utilized as covariates. Covariates that met a significance level of p < 0.2 in the univariable analysis were included in the multivariable analysis. A backwards multivariable logistic regression was performed and only variables that met significance were included in the final model. Only the results of obesity are displayed. p-values of ≤ 0.05 were considered statistically significant.
RESULTS
1. Patient Cohort and Characteristics
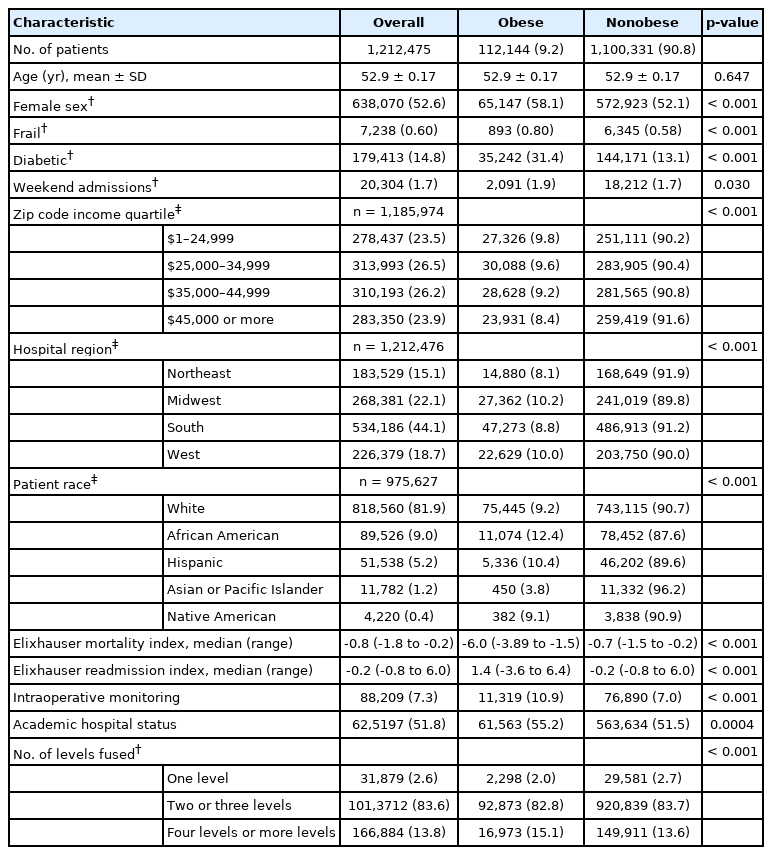
From 2004 to 2014, estimated 1,212,475 ACDFs were identified in the NIS. Of these discharges, 112,144 (9.2%) were obese. Table 1 displays the ACDF cohort characteristics stratified by obesity status. Compared to nonobese patients, obese ACDF patients were more likely to be female, frail, diabetic, and be from the Midwest or Western regions. Socioeconomically, obese patients resided in lower income zip codes and were more likely to be African American or Hispanic. Obese patients had worse baseline health status as indicated by higher Elixhauser readmission and mortality indexes. With regards to operative covariates, obese patients were more likely to receive operation at an academic hospital, have intraoperative neuromonitoring, and require more levels fused.
2. Obesity Incidence
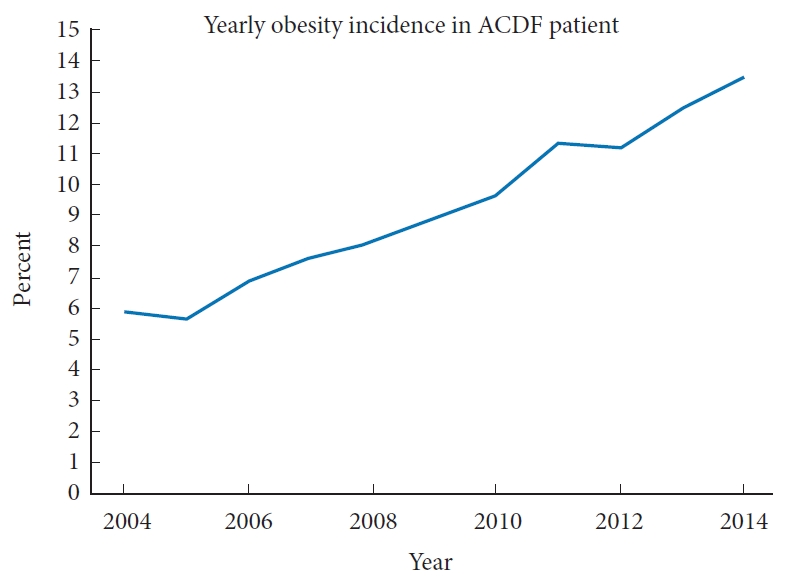
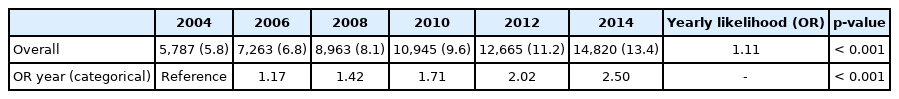
Fig. 1 shows the yearly trend of obesity incidence in patients that underwent ACDF. Additionally, Table 2 displays the univariable logistic regression trends of obesity incidence. The incidence of obesity amongst ACDF patients has risen dramatically from 2004 to 2014 (5.8% to 13.4%). When year is utilized as a continuous variable the yearly likelihood for an ACDF patient to be obese is 1.11 (p < 0.001), indicating that each year the obesity likelihood is 10% greater than that of the previous year. When year is utilized as a categorical variable, ACDF patients in 2014 were 2.5 times more likely to be obese than those in 2004 (p < 0.001).
3. ACDF Outcomes and Obesity
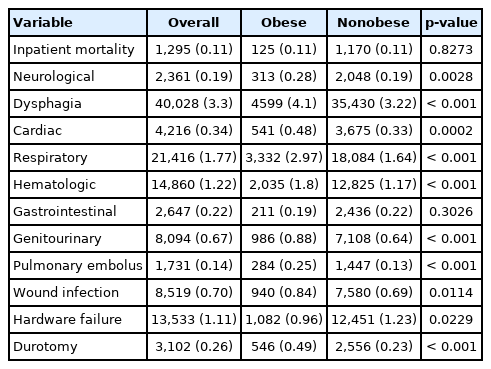
Various ACDF complication rates and outcomes stratified by obesity status are displayed in Table 3. On univariable analysis, there was no difference in inpatient mortality or gastrointestinal complications between obese and nonobese patients. Obese patients had significantly higher rates of dysphagia, neurological, cardiac, respiratory, hematologic, and genitourinary complications, as well as pulmonary emboli, wound infections, and durotomy. Obese patients demonstrated significantly less inpatient hardware failures.
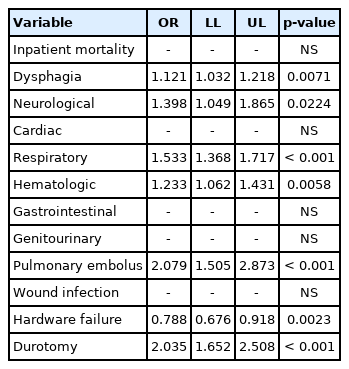
On separate multivariable analyses that adjusted for various patient, hospital, and operative covariates (Table 4), we found that obesity was independently correlated with higher inpatient likelihood of dysphagia, neurological, respiratory, and hematologic complications, pulmonary emboli, and durotomy. Furthermore, obesity was independently correlated with a lower likelihood of inpatient hardware failure.
DISCUSSION
1. Incidence
Obesity is an increasing global public health issue. The mean worldwide BMI has been increasing by 0.4–0.5 kg/m2 per decade since 1980 [18]. In the US, the estimated obesity prevalence is 93.3 million adults, 35% among men and 40.4% among women [19,20]. Over our 10-year study period, we observed a significant increase in obesity incidence among the ACDF population (Fig. 1). This trend is expected as the US elderly and obese population grows, especially since obesity is a known risk factor for intervertebral disc degeneration (DD) [8]. Teraguchi et al. [7] identified obesity (defined as BMI> 27.5 kg/m2) as a risk factor for DD, throughout the entire spine including the cervical region (odds ratio [OR], 1.60; 95% confidence interval [CI], 1.04–2.51). Since the proportion of obese patients undergoing ACDF has expanded in the last decade, the potential negative impact on surgical outcomes in spinal surgery has become increasingly relevant. While studies in the literature established an association between obesity and an increase in mortality, hospitalization costs, comorbidities, and postoperative complications in patients undergoing general and cardiac surgery, these studies are often small single-center cohorts [3,10,12].
2. Adverse Outcomes and Mortality
Prior studies have examined the association between BMI and outcomes in thoracic and lumbar spinal surgery [3,4,12,21-24]. However, the availability of data regarding ACDF is limited and conflicting. Our analysis of 1,212,475 patients showed that obesity is associated with several postoperative complications (Table 4). This is consistent with a meta-analysis published by Jiang et al. [3] which analyzed 32 studies involving 97,326 patients in order to assess the relationship between obesity and surgery in all regions of the spine. They showed that obesity is a significant risk factor for wound infections, venous thromboembolism, mortality, revision rate, operating time, and blood loss. Similarly, Kalanithi et al. [12] conducted a retrospective cross-sectional study of 84,607 patients which demonstrated that morbid obesity increases hospital costs ($108,604 vs. $84,861, p < 0.001), mortality (0.41 vs. 0.13, p < 0.01), length of stay (4.8 days vs. 3.5 days, p < 0.001), and complication rates (13.6% vs. 6.9%) after anterior cervical and posterior lumbar procedures. The rate of adverse outcomes was more pronounced in ACDF (OR, 2.2), accounted for by pulmonary (3.9% increase; OR, 3.1) and wound complications (2.6% increase; OR, 1.8). However, their study only examined morbid obesity, excluding those with a BMI between 30 and 39.9 kg/m2. We found that obese patients had an increased risk of developing neurologic (OR, 1.4; 95% CI, 1.05–1.29; p = 0.02) and respiratory complications (OR, 1.5; 95% CI, 1.37–1.72; p < 0.001), as well as pulmonary embolus (OR, 2.08; 95% CI, 1.51–2.87; p < 0.001). These results suggest that the initialization of a preoperative weight loss program may mitigate the risk of complications in elective ACDF. However, large prospective trials must confirm this.
Some authors argue that obesity does not impact surgical outcomes. Buerba et al. [11] found no association between obesity and an increased complication rates, length of stay, and mortality during the first 30 postoperative days in a cohort of 3,671 and 400 anterior or posterior cervical surgeries, respectively. Furthermore, several other studies have found no difference in early postoperative complications [10]. While our study also failed to find an association with increased in-hospital mortality rates, we did find a change in postoperative complication rates. Limited data availability, small sample size, short postoperative follow-up, and differences in study design may account for the inconsistency found in the literature regarding the impact of obesity in ACDF as opposed to the better-established association found on lumbar surgery.
3. Surgical Site Infections
We found no statistically significant difference in surgical site infections (SSI) between obese and nonobese patients (Table 4). BMI may not be the only risk factor to consider in obese patients. The role of weight distribution was examined by Mehta et al. [4]. which identified the thickness of subcutaneous fat (30.2 mm vs. 23.9 mm, p = 0.035) and the distance of the lamina from the skin surface at the level of L4 (74.8 mm vs. 67.4 mm, p = 0.046) as significant and independent risk factors for the development of SSI in 298 patients who underwent lumbar spine fusion surgeries when compared to the control group. They performed a similar study regarding posterior cervical surgery in 213 patients and reported the thickness of subcutaneous fat was a significant risk factor for the development of a SSI (27.0± 2.5 mm vs. 21.4± 0.88 mm, p = 0.042). The mean overall distance from the lamina of C5 to the skin surface and the mean thickness of the paraspinal muscles were not significant (p = 0.85) [25]. We believe SSI is less likely to occur in anterior cervical procedures as the amount of adipose tissue that needs to be dissected, retracted, and manipulated is significantly less than that of the posterior lumbar and cervical spine procedures [11].
4. Dysphagia
Incidence rates of dysphagia after ACDF vary in the literature from 1% to 79% [26-28]. A large database study with 2,723 patients conducted by Chung et al. [29] reported an incidence of 2.3%, with patients over 70 years old having higher risk. In our study, dysphagia was the most common complication of ACDF with a 3.3% incidence rate and obesity was significantly associated with the development of swallowing difficulties (4.1% vs. 3.22%; OR, 1.121; 95% CI, 1.032–1.218; p = 0.0071). In a retrospective multicenter study of 2,827 ACDFs, Wang et al. [30] also found that patients who developed immediate postoperative dysphagia had a higher BMI than those who did not (27.3 vs. 24.6 kg/m2, p ≤ 0.001). Liu et al. [27] reported a similar result during the first to second postoperative days. Our results agree with these studies, that obesity is associated with early postoperative dysphagia. This dysphagia may be caused by the increased thickness of the prevertebral tissue in obese patients, which leads to excessive esophageal retraction. Soft tissue edema, direct laceration of the esophagus, local ischemia due to increased intraesophageal pressure, pharyngeal plexus denervation by retractors, superior laryngeal nerve injury, or recurrent laryngeal nerve stretch injury during the lateralization of the larynx are possible etiologies for the development of dysphagia [26]. In contrast, Rihn et al. [28] and Siska et al. [31] compared the degree of dysphagia with a control cohort of posterior surgery cases and found no correlation with BMI. However, both studies had small ACDF sample sizes (n = 18 and 38, respectively).
5. Durotomy
Our study found that obesity portends an increased rate of durotomy during an ACDF procedure (0.49% vs. 0.23%; OR, 2.035; 95% CI, 1.652–2.508; p ≤ 0.0001). This is likely due to the increased thickness of the prevertebral tissue in obese patients that makes the approach and surgical manipulation more challenging. In a retrospective study of lumbar spine procedures, Burks et al. [32] observed that obesity and the complexity of the procedure independently increased the rate of incidental durotomy. On the contrary, Desai et al. [33] reported a lower BMI in the durotomy cohort compared to the nondurotomy group (29.6 kg/m2 vs. 27.1 kg/m2, p = 0.021) in patients who received lumbar surgery. In the cervical region, Baker et al. [34] reported obesity was not a risk factor, although elevated surgical invasiveness was associated.
6. Hardware Failure
Screw/plate loosening and nonunion are rare but known complications in ACDF. Several factors may predispose patients to hardware failure, such as osteoporosis and multilevel fixation [35]. We observed a lower likelihood of hardware failure in obese patients (OR, 0.788; 95% CI, 0.676–0.918; p = 0.0023). Some authors have reported that BMI does not affect the rates of arthrodesis and the need for reoperation in cervical and lumbar procedures [36], and although Jiang et al. [3] found higher revision rates in obese patients, the majority were the result of recurrent disc herniation. We are not certain why obese patients would experience less hardware malfunction however it may be secondary to the fact that they are less likely to develop osteopenia/osteoporosis or perhaps, it is because nonobese patients are quicker to mobilize, leaving them more susceptible to hardware malfunction. Other large database studies identified younger age, being male, and suffering psychiatric disorders as independent risk factors for reoperations [37] and patients discharged early had higher readmission rates, especially amongst older adults [38].
7. Limitations
This study has several imitations. Firstly, the data from the NIS is dependent on proper ICD-9 coding which can have errors and consequently alter patient selection. To that end, it has been observed that the NIS underreports obesity [39]. The database does not include adverse events after discharge, which prevents any evaluation of follow-up data, although the objective of this study is to report perioperative complications. Campbell et al. investigated ICD-9 based assessments and found that it is linked to underreporting of surgical complications in retrospective studies [40]. Secondly, we did not further stratify patients into obesity subgroups, which may limit the applicability of the results to these specific cohorts, especially, morbidly obese patients, for which an association has been suggested [12].
In conclusion, obesity is a well-established modifiable comorbidity that leads to increased perioperative complications in various surgical specialties. We present one of the largest retrospective analyses evaluating the effects of obesity on inpatient complications following ACDF. The incidence of obesity amongst ACDF patients has risen dramatically. Obese ACDF patients had higher inpatient likelihood of dysphagia, neurological, respiratory, and hematologic complications as well as pulmonary emboli, and intraoperative durotomy.
Notes
The authors have nothing to disclose.