Comparative Analysis of Transforaminal Endoscopic Thoracic Discectomy and Microscopic Discectomy for Symptomatic Thoracic Disc Herniation
Article information
Abstract
Objective
To evaluate the clinical outcomes of transforaminal endoscopic thoracic discectomy (TETD) and microscopic discectomy (MD) for the treatment of symptomatic thoracic disc herniation (TDH).
Methods
Seventy-seven patients (mean, 55.9 years; follow-up, 11.2 months) with symptomatic TDH were retrospectively reviewed (39 TETD and 38 MD). Radiological factors and perioperative outcomes were reviewed. Visual analogue scale (VAS), Oswestry Disability Index (ODI), and American Spinal Injury Association impairment scale were used to evaluate clinical and functional outcomes. Patient satisfaction was evaluated using modified MacNab criteria.
Results
The levels of surgery and the location of hernia were evenly distributed in the both groups. The operative time (70.6 minutes vs. 175.7 minutes), estimated blood loss (3.8 mL vs. 357.4 mL), and length of hospital stay (7.0 days vs. 13.0 days) were significantly different between the TETD and MD groups (p<0.05). VAS scores for dorsal back pain and ODI scores were significantly improved in both groups (p<0.05). Patients who underwent TETD tended to be more satisfied with the outcome in terms of the modified MacNab criteria (89.7% vs. 73.0%, p=0.059). Two patients in the MD group underwent revision surgery, whereas one patient in the TETD group underwent MD because of incomplete decompression.
Conclusion
TETD for the symptomatic TDH is a feasible and safe procedure that could be used for a wider range of surgical levels with a shorter operative time and hospital stay and less blood loss. While achieving similar outcomes, TETD achieved better patient satisfaction because of the use of local anesthesia and its minimal invasiveness.
INTRODUCTION
Symptomatic thoracic disc herniation (TDH) is a relatively uncommon condition, accounting for less than 1% of all disc herniations [1,2]. If appropriate conservative treatment, such as epidural steroid injection, physical therapy, and medication, fails to improve patients’ symptoms, surgical treatment is indicated. Progressive myelopathy with a significant neurologic deficit is an absolute surgical indication for TDH. Surgical treatment for TDH has been widely applied according to the location and characteristic of the hernia, clinical presentation, and surgeon’s experience with approaches ranging from the posterior approach (laminectomy) to posterolateral (transpedicular, transfacet), lateral (costotransversectomy, lateral extracavitary), ventrolateral (transthoracic, mini-thoracotomy, thoracoscopy), and ventral (transsternal) approaches. The choice of thoracic disc resection is largely determined by the location and nature of the hernia, the clinical picture, the surgeon's training, clinical experience, and personal preference. Because excessive surgical morbidity can be counterproductive, it is even more important to choose the least morbid surgical approach for thoracic disc resection. The surgical approach to the thoracic spine is often accompanied by approach-related complications that cause instability and neurological deterioration because of the unique susceptibility of the thoracic spinal cord to retraction injury [3]. Clinical symptoms of TDH are often presented as various types of severe, incapacitating pain and any surgical access will cause [4]. This makes the selection of a minimally pathological surgical approach for thoracic disc resection even more important.
The treatment of degenerative spinal disease is continuously evolving because of the progression of minimally invasive spinal surgery. The minimally invasive surgeries for TDH include video-assisted thoracoscopic discectomy, microscopic discectomy (MD), and transforaminal endoscopic thoracic discectomy (TETD). Currently, TETD has been described as a safe procedure with favorable outcomes for TDH [5-10]. In the case of paramedian or foraminal disc herniation, a posterolateral approach or posterior approach is appropriate. MD has consisted with both posterior and posterolateral approach. Laminectomy is mainly attempted to decompress spinal canal stenosis but has limitation of ventral decompression due to spinal cord retraction [11]. Posterolateral approach such as transpedicular [12] or trasnfacetal approach [13] has been reported with good clinical outcome in resecting herniated disc without complications. To the best of our knowledge, no study has compared TETD and MD for TDH. In this study, we compared the clinical outcomes of TETD and MD in patients with symptomatic TDH.
MATERIALS AND METHODS
1. Study Design and Patient Population
After receiving approval from the Institutional Review Board of Wooridul Spine Hospital (WRDIRB-2020-02-006), 84 patients with symptomatic TDH who underwent either TETD or MD between January 2016 and August 2019 at Wooridul Spine Hospital were retrospectively reviewed. Inclusion criteria were (1) diagnosis of paramedian or foraminal soft TDH confirmed by magnetic resonance imaging (MRI) findings corresponding to the patient’s clinical symptoms, (2) dorsal back pain with or without radiating pain, or mild myelopathy (American Spinal Injury Association [ASIA] grade C, D) associated with TDH, and (3) failure of appropriate conservative treatments including medication, physical therapy, and epidural steroid injection. The exclusion criteria were (1) extensive calcified or hard disc herniation, (2) concomitant ossification of the posterior longitudinal ligament (OPLL), (3) central extruded herniation, (4) spinal fracture or instability, (5) infection, and (6) tumor.
2. Assessment of Perioperative Outcomes
Perioperative data were assessed using clinical charts and operative records. Before and after surgery, dorsal back or leg pain was measured using the 10-point visual analogue scale (VAS) (score range 0–10), and function was assessed using the Oswestry Disability Index (ODI) (score range 0–100). To evaluate the neurological level of impairment, we recorded the preoperative and postoperative American Spinal Injury Association impairment scale score. Patient satisfaction was assessed using modified MacNab criteria (excellent, good, fair, or poor). Grades of excellent and good were regarded as satisfying results, whereas grades of fair and poor as nonsatisfying results. All postoperative outcomes were obtained at the last follow-up.
Radiological factors such as the location of the herniation, presence of disc calcification, and combined ossification of the ligamentum flavum (OLF) were evaluated with MRI and computed tomography scans. Axial locations of disc herniation were categorized as paramedian or foraminal.
The levels of surgery were categorized into 3 subgroups: upper (T1–2 to T4–5), middle (T5–6 to T8–9), and lower (T9–10 to T12–L1) thorax. The operative time, estimated blood loss (EBL), hospital stay, and rate of complications were evaluated to assess the outcomes of the surgeries.
3. Operative Procedure
In TETD, surgery was performed using local anesthesia and intravenous sedation with the patient in the prone position. The skin entry point was commonly located approximately 5–6 cm from the midline. After infiltration of local anesthetics, an 18G needle is advanced along the planned trajectory under lateral fluoroscopic view to the lateral aspect of the superior facet. A guidewire was inserted through the needle. Discography was performed by injecting a mixture of radiopaque dye and indigo carmine. Foraminoplasty was performed using a round reamer or bone drill. The 3.1-mm endoscope (TESSYS thx, Joimax GmbH, Karlsruhe, Germany) was introduced through a 5.8-mm outer diameter working cannula. Under the direct visualization, a blue-stained annular surface and herniated disc fragment could be identified. By removing the annulus of the outer layer and the internal layer of the posterior longitudinal ligament (PLL) with a side-firing laser, the blue-stained herniated fragment was released from anchoring. Then the fragment was removed using microforceps The Ho:YAG laser was used to resect the PLL, thickened annulus, and partially calcified hernia. After adequate decompression, the skin was closed, and a sterile dressing was applied (Fig. 1A-H).

Case presentation of a 50-year-old male patient presenting with thoracic back pain and radiating pain in the left chest. Preoperative sagittal (A) and axial (B) magnetic resonance imaging (MRI) scans show paramedian thoracic disc herniation at the T7–8 on the left side. The transforaminal approach is used for endoscopic discectomy. (C, D) The intraoperative fluoroscopic view shows the placement of the working channel. Endoscopic view showing removal of blue-stained disc fragment with endoscopic forceps (E) and full decompressed dural sac (F). (G, H) Postoperative MRI scans show decompression of the spinal cord after discectomy.
In MD, the patient was placed on a Wilson frame in the prone position under general anesthesia. The surgical level was localized utilizing C-arm fluoroscopic guidance. After making a midline incision, subperiosteal dissection was performed to expose the interlaminar space. Using a high-speed drill and a curette, partial hemilaminectomy, medial facetectomy, and flavectomy were performed under microscopic visualization. In case of dural sac is extended laterally, facetectomy is extended or partial pediculotomy was done to avoid dural retraction. Annulotomy was performed with a carbon dioxide (CO2) laser followed by gentle fragmentectomy with a microscopic instrument. We did not retract the dura mater but dissected the ventral epidural space to squeeze the fragment and pull it out of the annulotomy site with a right-angled dissector. After thorough decompression of the neural structure was achieved, closure was performed in a conventional way (Fig. 2A-G).

Case presentation of a 61-year-old female patient presenting with thoracolumbar back pain and left inguinal pain. (A, B) Preoperative magnetic resonance imaging (MRI) scans show left paramedian disc herniation at the T9–10 level. (C) Axial computed tomography scan shows ossification of the ligamentum flavum at the same level. Under the microscopic view, partial hemilaminectomy and medial facetectomy are performed. (D, E) With gentle dissection of the ventral epidural space, the disc space (arrowhead) is exposed followed by fragmentectomy. Note the white disc fragment (arrow). (F, G) Postoperative MRI scan shows satisfactory decompression of the spinal cord.
4. Statistical Analysis
Descriptive statistics for continuous variables are presented as means with standard deviations, and dichotomous variables are presented as frequencies with percentages in parentheses. Collected variables were compared to assess the statistical significance of any differences after the respective operative method (group A vs. group B). We used, where appropriate, Mann-Whitney U-test and t-test for continuous variables, and Pearson chi-square test and Fisher exact test for dichotomous variables, without missing data imputation. All statistical tests were performed using 2-sided tests, and p-values < 0.05 were considered statistically significant. All analyses were performed using the statistical software package SAS 9.4 (SAS Institute, Cary, NC, USA).
RESULTS
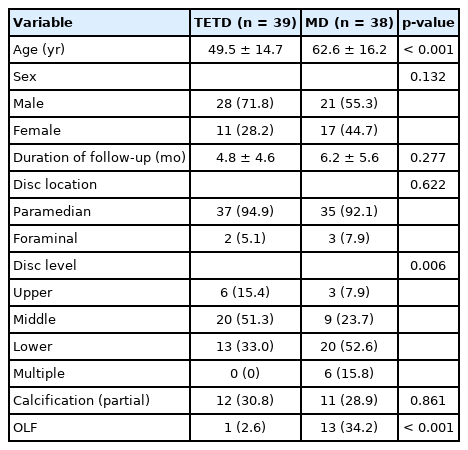
Among 84 patients, 77 patients (mean age, 55.9±16.6 years, 49 men; mean follow-up, 11.2±5.2 months) met the inclusion criteria. TETD was performed in 39 patients (mean age, 49.5±14.7 years), and MD was conducted in 38 patients (mean age, 62.6±16.2 years). The levels of surgery were relatively evenly distributed in the TETD group (15% upper thorax, 51.2% mid thorax, and 33.3% lower thorax) and MD group (7.8% upper thorax, 26.3% mid thorax, and 65.7% lower thorax). Concomitant OLF was more common in the MD group than in the TETD group (34.2% vs. 2.6%, p<0.001). The axial location of disc herniation and calcification of the disc did not have a between-group difference (p=0.622 and p=0.861, respectively). Patient demographics are summarized in Table 1.
Preoperatively, the VAS score was significantly lower in the TETD group (7.5±0.6) than in the MD group (7.9±0.8) (p=0.014). No significant difference in the preoperative ODI score was observed between the groups (p=0.095). The distribution of the preoperative ASIA impairment scale score was significantly different between the groups (p=0.009). The MD group had a higher percentage of neurologically impaired patients than the TETD group. There were no significant differences in postoperative outcome measurements, including VAS, ODI, and ASIA impairment scale scores between the groups (p=0.082, p=0.121, and p=0.080, respectively). Patients who underwent TETD tended to be more satisfied with the outcome in terms of MacNab criteria than those who underwent MD (89% vs. 71%, p=0.059). The mean operative time, EBL, and hospital stay were significantly different between the groups. The TETD group had a significantly shorter operative time (70.6±25.4 minutes vs. 175.7±54.8 minutes, p=0.002), less EBL (3.8±17.7 mL vs. 357.4±239.8 mL, p<0.001), and shorter hospital stay (7.0±8.6 days vs. 13.0±7.50 days, p=0.002) than the MD group. One patient in the TETD group underwent MD because of incomplete decompression. Two patients in the MD group underwent revision surgery because of incomplete decompression and the presence of a postoperative hematoma on the next day after surgery (Table 2).
DISCUSSION
The management of TDH is evolving continuously because of the progression of minimally invasive spinal surgery. Mack et al. [14] and Horowitz et al. [15] were among the first to describe minimally invasive endoscopic approaches to the thoracic spine by the technique of video-assisted thoracic surgery. Advances in minimally invasive spinal surgery have allowed for the endoscopic removal of TDH. Jho described the technique of endoscopic transpedicular thoracic discectomy with 0° and 70° 4-mm endoscopes that requires a relatively small 2-cm incision and minimal tissue dissection [16]. This approach avoids the need for a separate skin incision in the chest wall, which is required for thoracoscopic approaches, and the need for postoperative chest drainage. Several publications on outcomes of endoscopic thoracic discectomy have confirmed the efficacy and safety of the procedure [9,10,17-20]. Cho et al. [21] reported oblique paraspinal approach which made skin incision on 5–6 cm lateral from midline to place tubular retractor on the facet joint then drilling it to expose exiting root and lateral portion of dural sac. As a modification of transfacetal approach, it avoids necessity of dural retraction as well as provides good microscopic visualization on the ventral dural space. In the present study, authors’ MD technique included partial facet resection with or without pediclotomy, which is also modification of transfacetal or transpedicular approach. With the usage of CO2 laser, a safe and delicate resection of hernia was possible without aggressive facet or pedicle resection.
The present study showed that TETD and MD are effective treatments for symptomatic TDH. In terms of demographics, there were significant difference in terms of age and presence of OLF between the groups. MD group was older (49.5 years vs. 62.6 years) and concomitant OLF (2.6% vs. 34.2%). High prevalence of OLF is reason of older patient population in MD. Due to high prevalence of OLF in the lower thoracic level, MD groups tended to have more lower thoracic level surgery. However, this difference did not affect the clinical and functional outcomes between groups. This implies importance of preferred indication of each surgical approach according to concomitant degenerative pathology at the index level. Patients from both groups reported lower postoperative ODI and VAS scores than preoperative scores, with satisfaction. There were no significant differences in the clinical outcome measures, such as the postoperative VAS, ODI, and ASIA impairment scale scores, between the groups. TETD had a significant advantage in terms of awake anesthesia, less blood loss, and short operative time and hospital stay. For these reasons, patients who underwent TETD tended to be more satisfied with the outcome in terms of modified MacNab criteria than those who underwent MD. This result is concordant with recent systemic review that reported as excellent or good outcomes were achieved for full endoscopic procedures in a mean of 81% of patients (range, 46%–100%) with a complication rate of 8% (range, 0%–15%), comparing favorably with rates reported after open discectomy (anterior, posterolateral, and thoracoscopic) or by endoscopic tubular assisted approaches [22].
In addition to less EBL and a short operative time and hospital stay, TETD has more benefits. Endoscopic discectomies generally do not require laminectomy or facetectomy, which induces postoperative spinal instability. Less traction on the neural structure can reduce nerve edema, and minimal neural tissue exposure reduces postoperative neural adhesion and prevents scar tissue formation, which can help improve surgical outcomes. Besides, TETD is associated with less possibility of postoperative morbidity due to local anesthesia, less blood loss, and short operative time and hospital stay, which makes both surgeons and patients comfortable with the selection. Moreover, the technique is associated with less approach-related muscle damage than conventional open surgeries, which carry a higher possibility of postoperative back pain. From this aspect, TETD may be more applicable to patients with intractable chronic dorsal back pain rather than motor weakness. Although one patient in our study had undergone MD because of incomplete decompression after TETD, there was no morbidity related to the revision surgery. Considering everything, TETD may be a primary surgical option for paramedian soft TDH with dominant dorsal back pain.
Although calcified herniation is considered to be challenging [10], partially calcified discs can be resected with a special endoscopic instrument, such as a high-speed drill and side-firing Ho:YAG laser [23,24]. In the present study, we treated 12 patients with partial calcification of the disc. Only one of them did not improve and was not satisfied postoperatively, so this patient underwent MD for wide decompression. The other 12 patients with calcified lesions had a relatively favorable outcome. Paolini et al. [25] reported 2 cases of successful resection of calcified TDH using an endoscope-assisted posterior approach. Under experienced surgeons, calcified herniation can be treated with a careful surgical approach and proper patient selection. It is necessary to consider open surgery for patients with concomitant OLF, OPLL, and hard disc. Favorable surgical outcomes using the CO2 laser in microscopic surgery for calcified lesions have been reported [26,27].
It is important to select an appropriate patient for TETD to avoid reoperation, conversion to open surgery, and surgical complications. Regarding multilevel TDH, MD may be more applicable than TETD because the operation time including the preparation is long and the radiation exposure to the patient and the surgeon becomes higher. In our cases, the TETD group had no multilevel TDH, whereas the MD group had multilevel TDHs in 5.3% of cases. Moreover, patients with severe neurologic deficits are not yet appropriate candidates for TETD. If a patient with TDH has a progressive motor weakness, MD with wide decompression or the transthoracic approach should be considered. Concomitant OLF compressing the spinal cord in addition to TDH causing myelopathy is another important factor in deciding the surgical approach. MD is superior in simultaneous 360° decompression of OLF and TDH causing severe myelopathy. In addition to microscopic decompression, posterior stabilization can be performed according to postoperative instability.
Despite some advantages of TETD, it still has many limitations as a standard treatment for TDH. TETD has a steeper learning curve. The specific endoscopic instrumentation, 2-dimensional endoscopic images, and operation through a small opening to reach the spine at a longer distance and greater angle are unique to endoscopy, and may not be intuitive to surgeons who are accustomed to only open procedures. This unfamiliarity may inevitably be related to postoperative complications or incomplete decompression. TETD should be performed by a spinal surgeon who is not only experienced in open surgery but also familiar with endoscopic spinal procedures, with a thorough surgical plan.
Despite the strength that the present study is the first to compare the clinical outcomes of TETD and MD, it has some limitations. First, this retrospective review relied on existing medical records for the collection of clinical and operative data. Second, our study had selection bias. The differences in patient characteristics may have affected the results. Patients in the MD group were significantly older, neurologically impaired, and had more combined OLF than those in the TETD group. However, this difference reveals different indications of TETD and MD in treating symptomatic TDH. Prospective, randomized trials are necessary to provide conclusive results.
CONCLUSION
TETD for the symptomatic thoracic spine is a feasible and safe procedure that could be used for a wider range of surgical levels with a shorter operative time and hospital stay and less blood loss. Although TETD and MD achieve similar clinical and functional outcomes, TETD achieved better patient satisfaction than MD because of the use of local anesthesia and its minimally invasive approach. In case the patient’s pain and neurological status is similar, MD is more applicable to patients with severe neurologic deficits and combined OLF.
Notes
Conflict of Interest
JB is a consultant for Joimax GmbH. SHL is a consultant for Joimax GmbH. JSK is a consultant of Richard Wolf, GmbH, and Elliquence, LLC. Except for that, no potential conflict of interest relevant to this article was reported.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: JB, SL, JK; Data curation: JK; Project administration: JB, JK; Writing - original draft: JB, JK; Writing - review & editing: JB.