Biportal Endoscopic Posterior Thoracic Laminectomy for Thoracic Spondylotic Myelopathy Caused by Ossification of the Ligamentum Flavum: Technical Developments and Outcomes
Article information
Abstract
Objective
Advanced biportal endoscopic surgery techniques can be used to treat thoracic myelopathy secondary to ossification of the ligamentum flavum (OLF). This case series elaborates on a feasible biportal endoscopic technique for thoracic OLF removal and evaluates clinical and radiological outcomes.
Methods
A biportal endoscopic posterior thoracic laminectomy was performed to remove the thoracic OLF. Surgical techniques have evolved from inside-out piecemeal removal methods to outside-in en bloc removal methods. Preoperative computed tomography was performed to analyze dural ossification and OLF types. Intraoperative videos were reviewed to observe dural ossification and to determine the surgical method. Neurological outcomes were assessed using the Japanese Orthopaedic Association (JOA) score.
Results
Clinical symptoms and neurological function improved markedly after surgery (JOA score, preoperative: 12.6 ± 1.0, final follow-up: 15.6 ± 1.2). The mean operation time per segment was not short (106.6 ± 38 minutes). At early experience stages, inside-out piecemeal decompression was used and it caused intraoperative spinal cord injury. However, outside-in en bloc decompression technique did not induce neural complications. Postoperative segmental instability and correlated mechanical back pain were not observed.
Conclusion
The biportal endoscopic posterior thoracic approach is an attractive surgical option to treat thoracic spondylotic myelopathy secondary to OLF. Piecemeal inside-out decompression can induce irreversible spinal cord injury, especially in the early experience stages. Outside-in decompression is more efficient and safer than inside-out pattern procedures by minimizing dural manipulation. Nonetheless, this technique is technically demanding and should only be performed in selected patients after acquiring abundant experience with endoscopic spine surgeries.
INTRODUCTION
Thoracic myelopathy caused by ossification of the ligamentum flavum (OLF) is uncommon. Decompression surgery is required in patients with neurological symptoms of thoracic myelopathy. Traditional surgical techniques for the treatment of thoracic OLF include open microscopic laminectomy. However, these techniques are traumatic to the normal structures of the thoracic vertebrae, and posterior instrumentation is necessary in cases of wide laminectomy [1]. Compared to open laminectomy, minimally invasive surgery reduces perioperative morbidity [2].
Endoscopic spine surgery, including full endoscopy and biportal endoscopy, has evolved from lumbar discectomy to the current treatment of a wide range of degenerative diseases [3-8]. Spinal endoscopic techniques have also been developed to reduce the need for additional instruments [4,9,10]. Full endoscopic thoracic approaches have been used to treat thoracic stenosis and have shown good surgical outcomes [11-15]. Biportal endoscopic surgery has also been described as a surgical technique to treat cervical and thoracic spondylotic myelopathy [16-18].
Additional pressure on a compressed spinal cord can induce irreversible neural injury. Therefore, a novel surgical technique that minimizes dural manipulation is necessary to safely remove thoracic OLF. Biportal endoscopic surgery is suitable for this requirement as it can perform delicate procedures intimated with the dura. A small-diameter endoscope can be used to visualize each corner of the spinal canal through a narrow extra space created by precise drilling.
We have developed a biportal endoscopic OLF removal techniques for treating thoracic myelopathy and analyzed the surgical outcomes according to different approaches.
MATERIALS AND METHODS
1. Study Patients
This prospective study analyzed patients who underwent posterior thoracic laminectomy using a biportal endoscopic system to treat thoracic spondylotic myelopathy due to OLF between January 2020 and December 2021 at 2 spinal centers. A single surgeon with 2 years of experience in biportal endoscopic lumbar spinal surgery performed all procedures. All consecutive patients who met the following inclusion criteria were included in this study.
(1) The presence of myelopathy symptoms in the back and legs for more than 6 weeks failing to respond to conservative treatment.
(2) Thoracic OLF, with or without spinal cord signal changes, confirmed using magnetic resonance imaging (MRI) and computed tomography (CT).
(3) Posterior thoracic OLF removal performed for one or 2 consecutive levels.
Patients were excluded based on following criteria:
(1) More than 3 consecutive levels of decompression surgery were necessary.
(2) Thoracic OLF was accompanied by segmental instability at the operating level.
(3) Thoracic OLF was accompanied by ossification of the posterior longitudinal ligament, involving more than 50% of the spinal canal and prominent disc herniation.
(4) A broad extent of dural ossification was identified on the preoperative CT.
2. Surgical Procedures
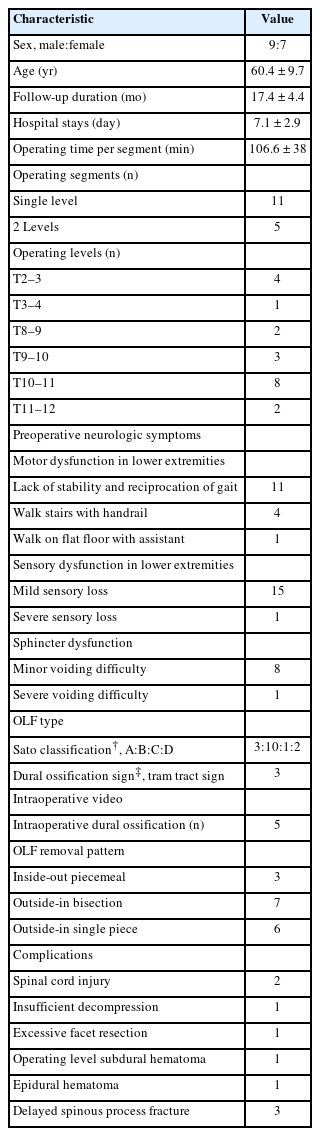
Surgical methods were divided into 3 types: inside-out piecemeal, outside-in en bloc removal as a single flap, and bisection flaps. Inside-out piecemeal removal referred to early exposure of the dura after partial laminotomy and flavectomy. Punches and dissectors were inserted into the space between the dura and the OLF to remove the ossified mass. Serial removal of the lamina and ossified flavum was repeated using a piecemeal removal pattern with a drill and punches. Outside-in decompression involved removing the lamina and ligamentum flavum by layer-by-layer drilling to expose the entire contour of the OLF (Fig. 1). The identified OLF was cut using a diamond drill and extracted with an en bloc pattern as a single piece (Fig. 1A-C) or bisected flaps (Fig. 1D-F). The 2 outside-in en bloc removal techniques consisted in the following steps (Supplementary video clip 1).
Illustrations showing 2 outside-in en bloc removal methods of ossification of the ligamentum flavum (OLF). (A, B) The ossified mass is not divided at the midline, the fused mass of the OLF and the thinned lamina were removed using the “single-piece removal” method. (C) Extracted flap as a single-piece from the T2–3 level. (D, E) Bilateral nonfused ossified masses are exposed after removing the lamina. Two divided flaps are serially removed with the “bisecting removal” technique. Small flaps are easy to manipulate during removal. (F) Removed bisected flaps from the T11–12 level. The ossified masses are cut at the medial part of facet joints (indicated by the asterisks).
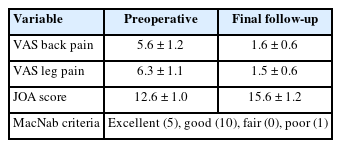
Patients underwent surgery under general anesthesia in the prone position on a chest bar or a radiolucent Wilson frame. The characteristics of the OLF determined the position of the surgeon. Under image intensification, 2 paramedian skin incisions were made at the medial border of the target-level pedicles to access the spinal canal bilaterally (Fig. 2A). A biportal endoscopic system (4 mm, 0° endoscope), a toolkit set, a customized scope retractor, and a working sheath (MD & Company, Seoul, Korea) were used for the procedure [17,19,20]. The working sheath was essential for the smooth insertion of surgical instruments and drainage of irrigation fluid (Fig. 2B).

Surgical steps are described with intraoperative photos and illustrations during the biportal endoscopic posterior thoracic laminectomy at the left T11–12 level. (A) Skin incision sites for the 2 portals on the C-arm image and on the patient’s back (bold white line, endoscopic portal; bold yellow line, working portal, white dotted circles: pedicles). (B) Scope retractor and working sheath are essential for spinal cord decompression surgery. The scope retractor is installed outside of the trocar (red arrow). (C) After ipsilateral laminotomy and spinolaminar junction drilling, the bilateral interlaminar space is widely exposed (upper figures). The medial facet joint is drilled to expose the bilateral superior articular process (SAP) and joint cartilages (right lower). Cranial laminotomy is performed until the tip of SAP (left lower) is identified. (D) Initial circumferential laminotomy is performed broadly over the ossification of the ligamentum flavum (OLF). The ossified mass is fixed to the lamina and SAP. The yellow dotted circle shows the margin of circumferential bony drilling. White asterisk: exposed epidural space. (E) If possible, split the midline ligamentum flavum to confirm the bilateral ossified mass and status of the dural compression (upper left). An extended ossified mass is commonly fused with lamina and is located at the cranial to the capsular part of the OLF (shown as red asterisks). This mass is removed first after marginal detachment (right upper and left lower). (F) The contour of the capsular ossified mass and the SAP are identified (right lower). The bilateral SAP is drilled along the lateral dural border until it appears as a thin paper (upper: ipsilateral, lower: contralateral). Black asterisk: exposed epidural space. (G) The secured OLF flap is detached and floated at the drilled border (right upper). The scope retractor (red arrowhead) elevates the ossified flap, and an epidural dissection is performed using a blunt hook (right upper). The ossified flap is removed after the epidural dissection is completed (left lower). Sufficiently expanded dura is observed, and the bleeding vessel is coagulated using the radiofrequency probe. Black asterisk: exposed epidural space; yellow asterisk: thick epidural. (H) Images from a 72-year-old woman who presented with symptoms of thoracic myelopathy. Preoperative magnetic resonance imaging (MRI) shows prominent OLF compressing the spinal cord at the T11–12 level (red arrowheads, upper figures). A preoperative axial MRI reveals a decompressed spinal cord at the bilateral spinal canal (left lower). Postoperative computed tomography shows laminectomy extent (right lower). The ipsilateral facet joint is preserved (shown as red asterisks). Blue dotted line: midline. S, superior; I, inferior; CL, contralateral; IL: ipsilateral; LF, ligamentum flavum.
The ipsilateral target lamina, upper part of the lower-level lamina, facet joint, and the bilateral interlaminar window were exposed after soft tissue dissection using a radiofrequency probe and forceps. An ipsilateral laminotomy, including the spinous process base, was performed using an endoscopic diamond drill to expose the bilateral interlaminar window (Fig. 2C).
Cranial laminotomy was extended until the proximal end of the OLF was exposed through the space created by sublaminar drilling. The cranial end of the laminotomy could be determined by identifying the tip of the superior articular process (SAP) or by confirming the intervertebral foramen under C-arm guidance, as the extended-type OLF is usually located in the foraminal area (Fig. 2C). Subsequently, circumferential bony drilling was performed over the estimated boundary of the OLF, laterally with the bilateral medial facet joints (Fig. 2C, D). The medial region of the SAP should be exposed after the initial bony drilling because the OLF is commonly fused with the SAP.
The midline of the ligamentum flavum was removed to divide the ossified mass into bilateral flaps. We confirmed the extent of OLF and dural ossification (Fig. 2E). After identifying the contour of the OLF, the remaining lamina and the bulky OLF were thinned using a diamond drill for easy manipulation during removal. The extended-type OLF commonly presents another bony ossification attached to the isthmic part, which is separated from the capsular OLF region. The extended part of the OLF was removed first and the capsular part was completely exposed (Fig. 2E). The capsular part of the OLF is fused to the SAP and is usually larger than the extended part. The bulky OLF was thinned using layer-by-layer pattern drilling (Fig. 2F). Subsequently, the medial part of the SAP was drilled bilaterally along the lateral dural border, until the epidural space was exposed (Fig. 2F). The secured OLF flap was removed from the bony edge using a fine dissector. The flap was gradually floated from the dura using a fine hook. Epidural dissection was performed safely using fine dissectors while holding the OLF flap with a scope retractor (Fig. 2G). Subsequently, the detached OLF flap was removed en bloc using forceps. A sufficiently decompressed thecal sac with free dural pulsation was also observed (Fig. 2G). The illustrated case shows the successful removal of bilateral OLF at the T11–12 level while preserving the facet joint (Fig. 2H).
If bisection of the ossified mass was difficult, the OLF and ligamentum could be lifted as a single flap (Fig. 1A–C). At this time, more attention should be paid to epidural dissection to prevent dural tear (Supplementary video clip 1).
A foamy hemostatic agent was used to achieve hemostasis of diffuse epidural bleeding. However, we recommend coagulating the epidural vessel if bleeding is noticeable, to prevent surgical site hematoma (Fig. 2G). The skin wounds were closed by inserting a drainage catheter through the working portal. Blood loss during surgery was minimal, with a total surgical duration of 80 minutes.
3. Data Collection
1) Collection of clinical data
This study was approved by the Ethics Committee of Wiltse Memorial Hospital (IRB No. 2022-W13). Patient characteristics including sex, age, and symptoms were recorded. The level of operation, operating time, and length of hospital stay, as well as any postoperative complications, were also documented. Physicians collected clinical information before, after and at the final follow-up in the ward and at outpatient departments. Visual analogue scale (VAS) for back and leg and MacNab criteria were used to assess clinical improvement. Neurological results were evaluated using the Japanese Orthopaedic Association (JOA) score.
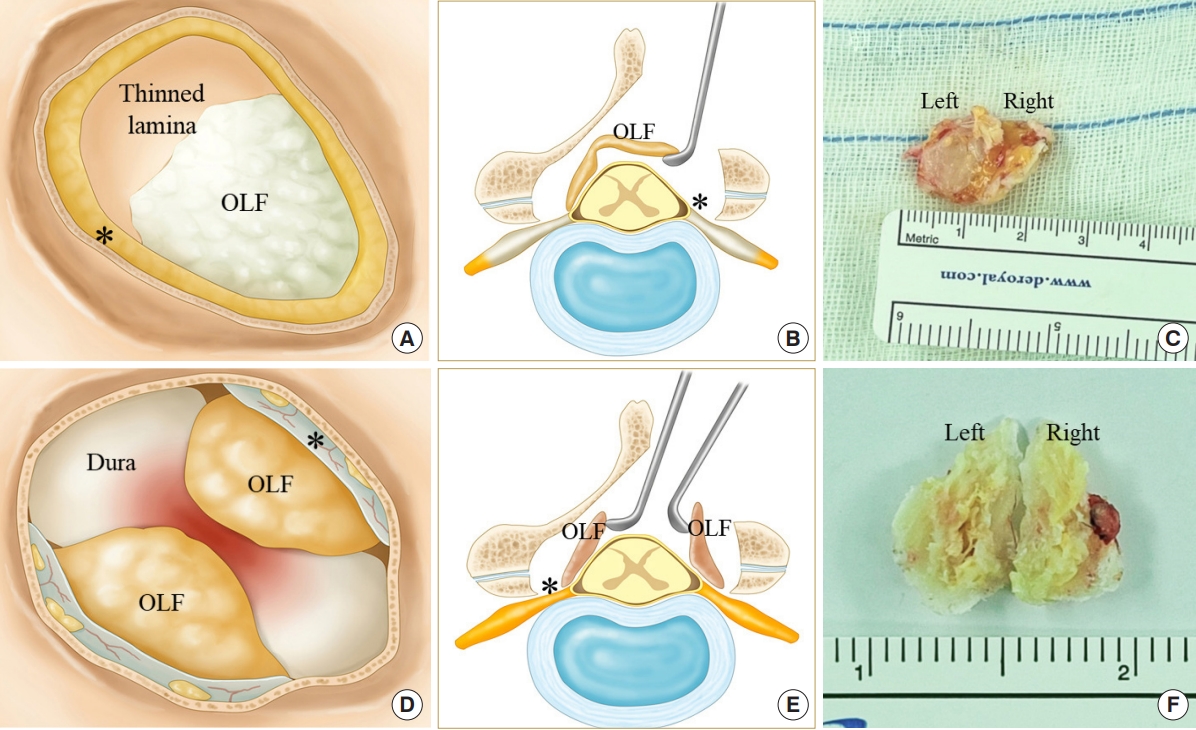
2) Radiologic evaluations
Preoperative CT and MRI were obtained to analyze dural ossification [21] (Fig. 3) and to categorize the Sato classification [22]. On postoperative day 1, MRI was performed to analyze the suitability of neural decompression and complications. The endoscopic operating video was thoroughly reviewed to observe intraoperative dural ossification (Fig. 3) and to determine the OLF removal pattern. In the video, the procedures that caused spinal cord injury were analyzed. Statistical analyses were performed with SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Preoperative and postoperative findings of the dural ossification in 2 cases. Case 1 (A-C) presented a symptomatic ossified ligamentum flavum at the T11–12 level. (A, B) Dural ossification (shown by the red arrowheads) was observed on the preoperative computed tomography (CT) and magnetic resonance imaging (MRI). (C) During the operation of this case, the inner layer is preserved (shown by the asterisk) after removing the outer layer of the ossified dura. A second case (D, E) did not present findings of dural ossification on the preoperative CT and MRI. (F) However, during operation, the dural ossification was observed, and the outer layer of ossified dura was peeled off from the inner layer (shown by the asterisk). The dural laceration did not occur due to the delicate working under magnified endoscopic vision.
RESULTS
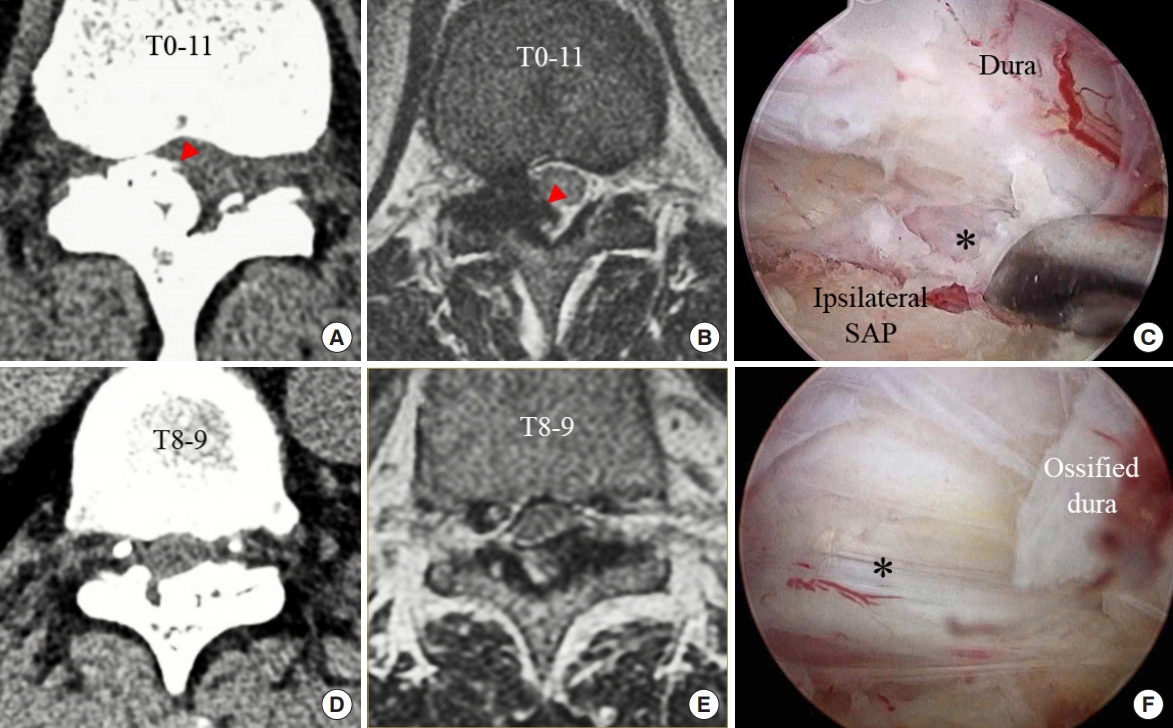
We included 16 patients (9 men and 7 women) who underwent posterior thoracic laminectomy using the biportal endoscopic system. The mean age was 60.4 ± 9.7 years (Table 1). The mean duration of follow-up and hospital stays was 17.4 ± 4.4 months and 7.1 ± 2.9 days, respectively (Table 1). The operating levels are listed in Table 1. Eleven patients underwent single-level decompression and 5 underwent 2-consecutive-level operations. The mean operation time per segment was 106.6 ± 38 minutes (Table 1). All included patients had neurological deficits caused by thoracic spondylotic myelopathy, and the most common symptoms were mild sensory loss in the lower extremities and lack of gait stability (Table 1).
The type of OLF was classified using the Sato classification [22] according to the progression of ligamentum flavum ossification. The lateral type refers to the ossification of only the capsular portion of the ligamentum flavum. The extended type refers to the extended ossification of the interlaminar portion. The enlarged type indicates anteromedial thickening and enlargement of the ossification. The fused type refers to fusion of the bilateral ossified masses at the midline. The tuberous type refers to anterior growth of the fused mass of ossification. Three patients had a lateral type; 10 patients had an extended type, 1 had an enlarged type, and 2 had a fused type. The tuberous type was excluded from this study.
Three patents presented a dural ossification “tram tract sign” [21] on the preoperative CT. We analyzed the intraoperative videos and observed 5 cases of dural ossification. Two patients with observed intraoperative dural ossification did not show signs of dural ossification on preoperative CT. We detached the ossified dura from the inner layer of the dura under magnified endoscopic vision but did not observe any dural laceration.
We differentiated the 3 surgical approaches according to the OLF removal pattern. Three patients in the early experience stages underwent OLF removal using the “inside-out piecemeal removal” method. At the middle and late experience stages, “outside-in bisection” and “outside-in single piece” en bloc removal techniques were performed in 7 and 6 patients, respectively. Of the 3 patients who underwent the “inside-out piecemeal removal” method, 2 exhibited spinal cord injury (Fig. 4A) and 1 presented insufficient decompression on the postoperative MRI (Fig. 4B). The 2 spinal cord injury patients could not stand alone without help and required a walking tool on the flat floor postoperatively. However, before surgery, they could walk without assistance even though they lacked gait stability. Of these, one patient recovered quickly from the illness and was able to walk without assistance; however, the other patient did not recover and needed walking assistance at the final follow-up. The patient with insufficient decompression showed marked improvement of myelopathy symptoms, but complained of persistent pain in the legs and back.
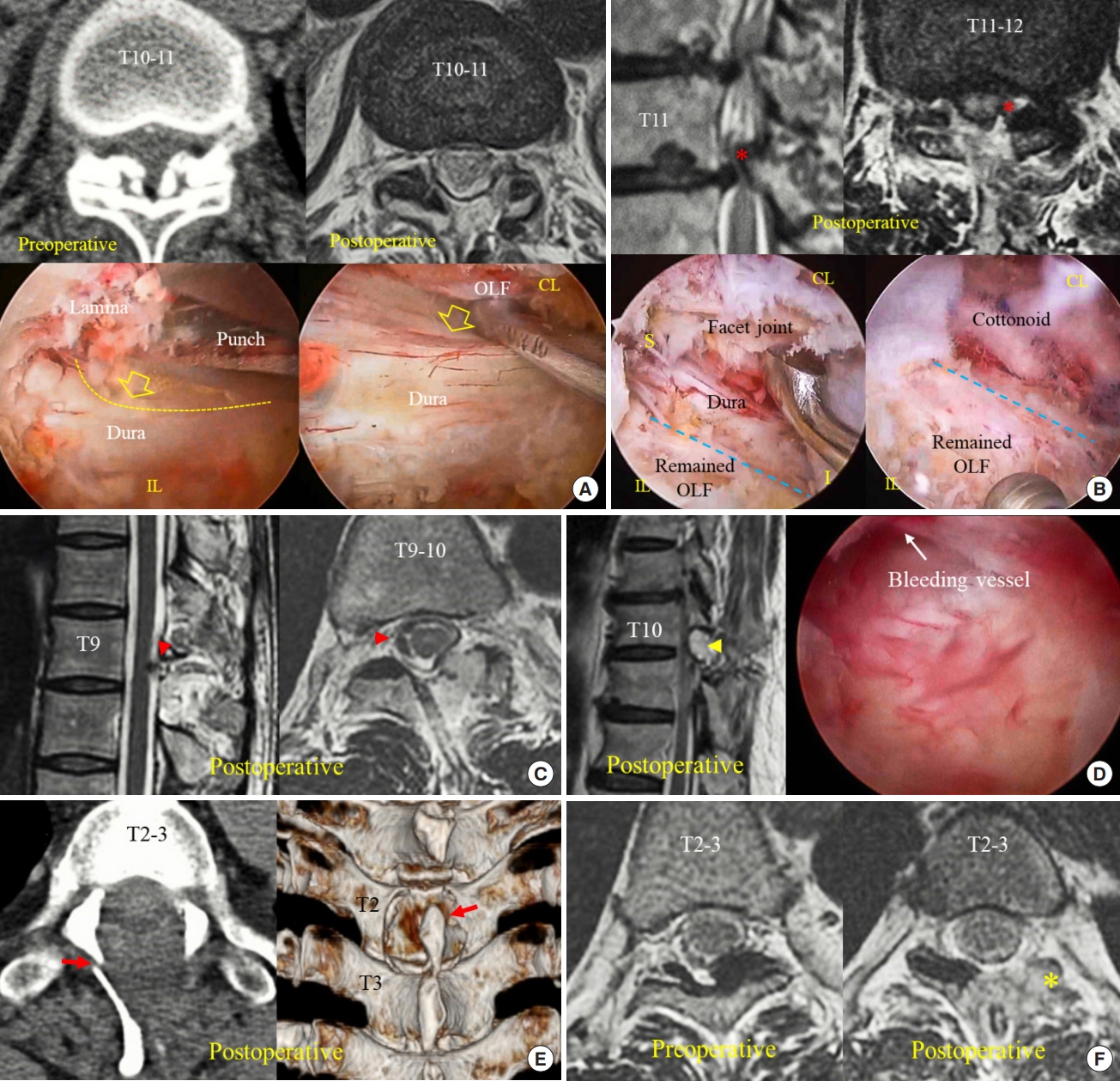
Cases of complications. (A) A 61-year-old woman underwent a biportal endoscopic thoracic laminectomy to remove the bilateral ossification of the ligamentum flavum (OLF). Postoperative magnetic resonance imaging (MRI, right upper) showing the complete removal of OLF, observed on the preoperative computed tomography (CT; left upper). In reviewing the intraoperative video, the punch compressed the dural sac during laminectomy (left lower), and the dissector severely pressed on to the spinal cord during contralateral dissection (right lower). These procedures were performed during the “inside-out piecemeal removal” method (open arrows: force to dural sac, yellow dotted line: compressed dural sac). (B) The postoperative MRI shows the residual ossified mass (red asterisks) at the left side of the T11–12 level (upper figures). Intraoperative photos reveal the residual ossified mass in the approaching side. Blue dotted line: midline. (C) An asymptomatic subdural hematoma is present on the postoperative MRI (red arrowheads). (D) A surgical site epidural hematoma (yellow arrowhead) is observed on the postoperative MRI (left). The intraoperative video reveals the bleeding epidural vein. An uncontrolled bleeding vessel might cause an epidural hematoma. (E) Spinous process fracture was found on the postoperative CT images (red arrows) after the left-side biportal endoscopic thoracic laminectomy at the T2–3 level. (F) The unilateral ossified mass was removed at the left T2–3 level using the biportal endoscopic posterior approach. Postoperative MRI showing the excessive facet resection at the approaching side (yellow asterisk). S, superior; I, inferior; CL, contralateral; IL, ipsilateral.
One patient who underwent a 2-level operation showed an asymptomatic subdural hematoma. We recommended 3 days of bed rest to prevent progression of the hematoma and the patient did not present any further neurologic symptoms (Fig. 4C). One patient showed an epidural hematoma on postoperative MRI and was treated with conservative treatment. An uncontrolled epidural bleeding vessel was observed on the intraoperative video, which might cause the epidural hematoma (Fig. 4D). Three patients with T2–3 and T3–4 level decompression had spinous process fractures on postoperative CT (Fig. 4E). One patient in the T2–3 level operation had an entirely removed facet joint (Fig. 4F). The upper thoracic vertebrae have smaller facet joints, lamina, and spinous processes. Therefore, preserving the midline bony structures was technically demanding, and excessive facet resection was inevitable for complete OLF removal. However, the patient did not complain of mechanical back pain during the follow-up period. Furthermore, none of the included patients showed any postoperative segmental instability on lateral flexion-extension x-ray images. Infused water-related complications were not observed, such as epidural fluid collection and increased intracranial pressure.
VAS scores for back and leg pain improved significantly after surgery (Table 2). Pain at the operating site was not noticeable because of the well-preserved muscle ligament structures. Neurological function of thoracic myelopathy was improved and confirmed with an increase in the JOA score (preoperative JOA score:12.6 ± 1.0, final follow-up:15.6 ± 1.2; Table 2). The results of the MacNab criteria showed satisfaction with the surgery (8 excellent, 10 good, 1 poor). The patient with a severe spinal cord injury showed poor response.
DISCUSSION
In patients with cervical or thoracic spondylotic myelopathy, the compressed spinal cord is vulnerable to intraoperative injury even with slight pressure exerted by the surgical instruments. If piecemeal removal procedures are used in patients with myelopathy, repetitive insertion of instruments between the dura and the ligamentum flavum can cause irreversible spinal cord injury. In this study, 2 patients who underwent OLF removal using the “inside-out piecemeal removal” method experienced intraoperative spinal cord injuries (Supplementary video clip 2). In reviewing the operating videos, punches repeatedly pressed on the spinal cord during laminectomy and the dissectors pushed onto the dural sac during contralateral sublaminar dissection (Fig. 4A). Furthermore, early dural exposure limited the free use of instruments and may have induced insufficient decompression. One patient who underwent inside-out decompression showed a noticeable residual mass, which prevented the improvement of symptoms (Fig. 4B). Therefore, the surgical techniques commonly used in lumbar decompression surgery may not be suitable for thoracic decompression surgery.
Novel techniques that minimize dural manipulation are necessary for the safe removal of OLF. Recently, Kim et al. [16,17] described biportal endoscopic en bloc removal techniques for treating cervical spondylotic myelopathy and cervical epidural cysts without complications. The key procedures of this technique include over-the-top decompression using layer-by-layer drilling and en bloc lesion removal; this technique was considered safe and efficient for removing thoracic OLF while minimizing dural manipulation. Full endoscopic surgery has also been used as an en bloc removal technique to treat thoracic OLF and has shown favorable surgical outcomes [13]. In this study, no neurological complications occurred after using the outside-in decompression method.
Before thinning and completing marginal drilling of the OLF, any inserted instruments between the OLF and dura have a high risk of spinal cord compression. It is impossible to completely control the punch not to hit the dura while punching the hard bone (Supplementary video clip 2). Incidental pressing on the dura can induce irreversible spinal cord injury, even if only once. Therefore, we should try to eliminate the risk of spinal cord injury during OLF removal procedures, and outside-in en bloc removal can decrease the chance of spinal cord compression.
Outside-in decompression and en bloc OLF removal can be technically demanding and attention should be paid to critical surgical steps. First, in the initial laminotomy step, the circumferential drilling boundary contains the ossified mass. The cranial and lateral endpoints of bone drilling should be determined prior to bone work. As the capsular part of the ligamentum flavum is ossified, the ossified mass fuses with the SAP. Therefore, the medial aspect of the SAP should be exposed after drilling the facet joint. The SAP can be differentiated from the ossified mass by confirming joint cartilage (Fig. 5). If the joint cartilage is not visible during lateral laminotomy, drilling may be directed to the OLF and spinal cord. An ossified mass commonly extends to the neuroforaminal area as the foraminal extended ligamentum flavum becomes ossified (Fig. 2E). Therefore, cranial drilling must be extended to the foraminal level. The foraminal location can be confirmed by identifying the SAP tip (Fig. 2C) or by using an intraoperative x-ray image.
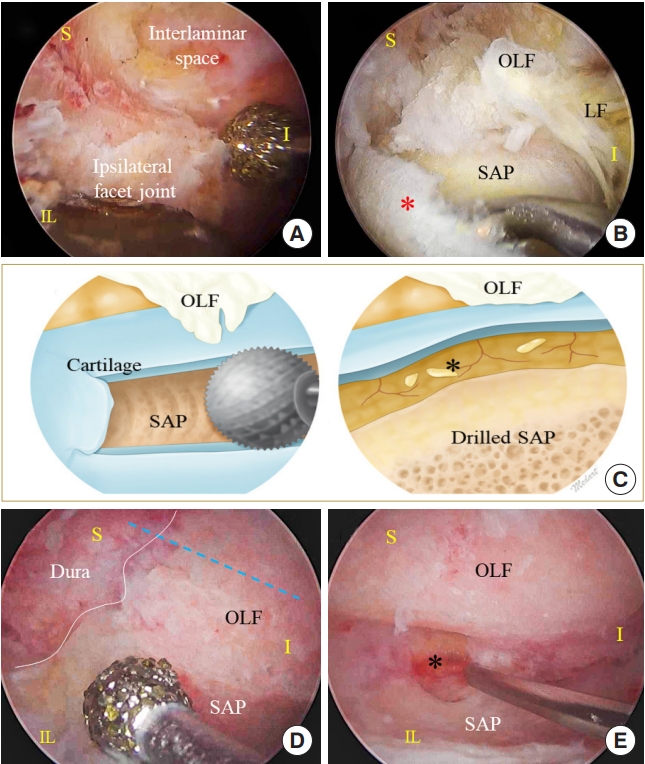
Essential steps for resection of the ossification of the ligamentum flavum (OLF). (A) The medial part of the facet joint is drilled to obtain the space necessary to access the lateral end of OLF. (B) Facet joint cartilage (shown by the red asterisk) should be exposed. The OLF is commonly fused with the medial border of the superior articular process (SAP). (C) Shown is the marginal cutting of the OLF. SAP drilling is performed along the lateral border of the dural sac until the epidural fat is observed. (D, E) Intraoperative image of SAP drilling and OLF cutting. Black asterisk: epidural fat, blue dotted line: midline. S, superior; I, inferior; CL, contralateral; IL, ipsilateral.
Second, the bulky OLF mass consists of hypertrophied SAP and an ossified ligamentum flavum. A diamond drill can slide along the outer surface layer of the OLF and can be peeled off in a layer-by-layer pattern. The thinned OLF is easy to manipulate and minimizes the risk of additional neural compression during the removal procedure (Fig. 1B, E). The thinned OLF can be cut into the SAP, which is covered by joint cartilage along the lateral border of the dural sac. This cutting location is critical for removing the OLF without any residual ossified mass, and the cutting tract is determined by an imaginary line of the dural lateral edge (Fig. 5).
Third, the half-and-half removal technique may be safer than the single-piece removal method for bilateral nonfused OLF. Smaller halved OLFs offer easier manipulation and reduce the risk of spinal cord compression. However, the midline portion of the OLF is fused to the lamina. Inserting the instruments into the epidural space to halve the ossified mass also exerts pressure on the vulnerable spinal cord. In this case, the single-piece removal technique could be a better surgical option than the half-and-half removal, although a more careful epidural dissection is necessary to prevent dural laceration (Fig. 1). If the OLF is elevated at the lateral border, the contralateral part of the OLF compresses the spinal cord due to the “seesaw phenomenon.” Resected OLF flap should be pulled outward from the medial edge using angled hooks or dissectors (Fig. 2G). Remained attachments between the OLF and bony structures can induce the “seesaw phenomenon” while manipulating the OLF. Therefore, we should remove the OLF flap after completely detaching it from surrounding bony structures.
Fourth, if the thinned OLF severely adheres to the dura, the endoscope moves more medially to visualize the dissecting plane, and careful dissection is performed between the ossified outer dural layer and intact inner dural layer using the sharp hook or dissectors. This technique should be performed under clear, magnified endoscopic vision to prevent dural laceration. However, in the case of whole-layer dural ossification, the OLF should not be excessively separated from the dura but should be floated and left on the dura.
Two customized surgical instruments and an endoscopic diamond drill were essential for a successful operation (Fig. 2B). The working sheath maintained good saline outflow and kept the epidural water pressure low. A low epidural water pressure allows safer long-time surgery at the thoracic spinal level. The scope retractor was installed on the endoscopic trocar. It acts as a neural tissue protector during bony drilling and retracts the ossified mass while detaching it from the dura.
The upper thoracic vertebrae, such as the cervical vertebrae, have smaller laminae, facet joints, and short spinous processes. Therefore, during the removal of bilateral OLF from the unilateral side of the upper thoracic level, the preservation of the spinous process and the contralateral lamina may be technically more challenging than at the lower thoracic level. In this study, excessive facet resection and delayed spinous process fracture occurred at levels T2–3 and T3–4 levels; however, these complications did not induce noticeable surgical site pain. Biportal endoscopic surgery preserves muscle ligament structures and may maintain segmental stability.
Although this technique has remarkable advantages, biportal endoscopic removal of OLF from the thoracic vertebrae should be considered in selected patients after gaining significant experience with endoscopic spinal surgery. Open surgery with wide laminectomy should be considered first in patients with severe signs of dural ossification [21] and Sato classification of tuberous type [22] on the preoperative CT scan. Continuous high-pressure saline infusion may increase epidural pressure and induce spinal cord injury [23]. The patency of the saline outflow should be monitored carefully and a saline infusion pressure below 30 mmHg is recommended. If incidental durotomy occurs during surgery, the hole should be repaired using a fibrin-sealant patch. However, if the endoscopic repair fails, open microscopic surgery should be performed to achieve complete dural repair [24]. Intraoperative electrophysiological monitoring is necessary to prevent iatrogenic spinal cord during surgery.
CONCLUSION
The biportal endoscopic posterior thoracic approach is an attractive surgical option for treating thoracic spondylotic myelopathy secondary to ossified ligamentum flavum. Inside-out piecemeal decompression in the early experienced stages can induce irreversible spinal cord injury. Outside-in en bloc removal with bisected flaps or single piece is safer than inside-out piecemeal removal because it minimizes dural manipulation. However, this technique is technically demanding and should be performed in selected patients after obtaining significant experience with endoscopic spine surgeries.
SUPPLEMENTARY MATERIALS
Supplementary video clips 1-2 can be found via https://doi.org/10.14245/ns.2346060.030.
Biportal endoscopic posterior thoracic laminectomy at the left T10–11 level using the “outside-in single-piece removal” technique. SAP, superior articular process; OLF, ossification of the ligamentum flavum.
Procedures causing spinal cord injury. Biportal endoscopic posterior thoracic laminectomy at the left T10–11 level using the “inside-out piecemeal removal” technique.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: JYK, JSH, CKL, DCL, SYC, CKP; Data curation: JYK, JSH, HJH; Formal analysis: JYK, JSH, CKL, HJH; Methodology: JYK, JSH, CKL, DCL; Project administration: JS Ha, CKL, DCL, SYC, CKP; Visualization: JY Kim, CKL, SY Choi, CKP; Writing - original draft: JYK, JSH; Writing - review & editing: JYK, JSH, CKL, DCL, HJH, SYC.