A Predictive Model of Failure to Rescue After Thoracolumbar Fusion
Article information
Abstract
Objective
Although failure to rescue (FTR) has been utilized as a quality-improvement metric in several surgical specialties, its current utilization in spine surgery is limited. Our study aims to identify the patient characteristics that are independent predictors of FTR among thoracolumbar fusion (TLF) patients.
Methods
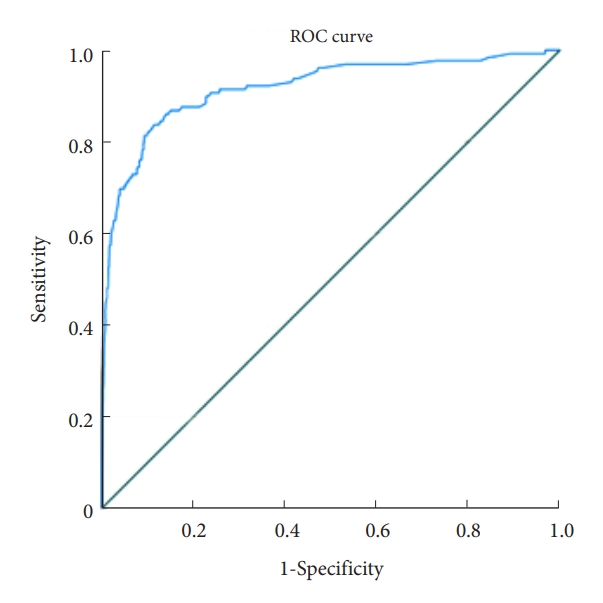
Patients who underwent TLF were identified using relevant diagnostic and procedural codes from the National Surgical Quality Improvement Program (NSQIP) database from 2011–2020. Frailty was assessed using the risk analysis index (RAI). FTR was defined as death, within 30 days, following a major complication. Univariate and multivariable analyses were used to compare baseline characteristics and early postoperative sequelae across FTR and non-FTR cohorts. Receiver operating characteristic (ROC) curve analysis was used to assess the discriminatory accuracy of the frailty-driven predictive model for FTR.
Results
The study cohort (N = 15,749) had a median age of 66 years (interquartile range, 15 years). Increasing frailty, as measured by the RAI, was associated with an increased likelihood of FTR: odds ratio (95% confidence interval [CI]) is RAI 21–25, 1.3 [0.8–2.2]; RAI 26–30, 4.0 [2.4–6.6]; RAI 31–35, 7.0 [3.8–12.7]; RAI 36–40, 10.0 [4.9–20.2]; RAI 41– 45, 21.5 [9.1–50.6]; RAI ≥ 46, 45.8 [14.8–141.5]. The frailty-driven predictive model for FTR demonstrated outstanding discriminatory accuracy (C-statistic = 0.92; CI, 0.89–0.95).
Conclusion
Baseline frailty, as stratified by type of postoperative complication, predicts FTR with outstanding discriminatory accuracy in TLF patients. This frailty-driven model may inform patients and clinicians of FTR risk following TLF and help guide postoperative care after a major complication.
INTRODUCTION
Rates of spinal fusions have more than doubled over the past 2 decades due to an increasingly older population [1]. Patients undergoing spinal fusion are at risk for a multitude of postoperative complications, which may result in death [2,3]. Mortality resulting from a potentially preventable postoperative complication, or failure to rescue (FTR), has been utilized as a patient safety indicator to track hospital performance and is a frequent target for quality improvement [4,5]. Although FTR prediction could improve patient outcomes and reduce healthcare costs, a reliable risk stratification tool has yet to be established [6,7].
Frailty is a measure of baseline physiological reserve [8]. The risk analysis index (RAI) is a frailty index that demonstrates superior discrimination in predicting adverse outcomes in spine surgery when compared to the 5- and 11-factor modified frailty index, as the RAI accounts for multiple domains of frailty [9-12]. Nevertheless, previous frailty studies predicting FTR after complications in spine surgery are sparse [13].
This study sought to analyze frailty, as measured by RAI, as a potential predictor of FTR in patients undergoing thoracolumbar fusion (TLF) using the American College of Surgeons National Surgery Quality Improvement Program (ACS-NSQIP) database.
MATERIALS AND METHODS
1. Study Design
The present study was designed as a secondary analysis of a quality-controlled, prospectively collected surgical database.
2. Data Source and Setting
Patient cases were acquired from the ACS-NSQIP (2011–2020), a validated database collected from over 700 participating institutions across 11 countries. The quality and consistency of these cases are optimized by ACS-trained data specialists [14]. This study was completed under our institution’s data user agreement with the ACS and is classified as exempt by our Institutional Review Board.
3. Participants
Thoracolumbar spine fixation cases were derived from the ACS-NSQIP using the following Current Procedure Technology codes: 22325, 22326, 22327, 22558, 22533, 22612, 22630, 22633, 22614, 22532, 22556, 22610, 22634, 22614, 22586, 22522, and 22556. The study cohort included adults (age ≥ 18) who experienced a major complication after TLF surgery. All diseases (degenerative/deformity, trauma, infection and tumor) were included. Cases were excluded if they were missing key case details, such as any variable required to calculate the RAI, length of stay, or discharge information.
4. RAI Revised
The revised RAI is a validated, quantitatively robust, frailty metric that has demonstrated superior discrimination across multiple neurosurgical subspecialties [15-18]. The RAI offers utility with its user-friendly calculation, which can be used at the point of care in clinical applications alongside large database studies. A patient’s RAI score is calculated using numerical values assigned to variables, including sex, age, cancer status, weight loss or low appetite, renal failure or use of dialysis, heart failure, shortness of breath, type of residence, and functional status, with final scores ranging from 0 (robust) to 78 (very frail).
5. Variables
Case variables included demographics (e.g., age, sex, race, and ethnicity), preoperative conditions (e.g., diabetes, hypertension, smoker status, and frailty), and postoperative outcomes (e.g., pneumonia, unplanned intubation, and cardiac arrest). Groups were created for renal complications (consisting of acute renal failure and renal insufficiency), and infections (consisting of deep surgical site infection [SSI], organ space SSI, and sepsis). The primary outcome of interest was FTR, defined as mortality within 30 days of surgery following any initial major complication. Major complications included deep SSI, organ space SSI, wound dehiscence, prolonged ventilation ≥ 48 hours, pulmonary embolism, cerebrovascular accident, renal failure, renal insufficiency, myocardial infarction, cardiac arrest, bleeding requiring transfusion, sepsis, septic shock, pneumonia, and unplanned reintubation.
6. Statistical Analysis
Frequency analysis, univariate regression, and multivariable regression were performed using IBM SPSS Statistics ver. 28.0 (IBM Co., Armonk, NY, USA). Receiver operating characteristic (ROC) analysis was performed using MedCalc ver. 20.114 (MedCalc, Ostend, Belgium). Statistical significance was determined a priori as α= 0.05. Whole cohort, FTR, and non-FTR subgroups were analyzed for frequencies of demographic, preoperative, and postoperative variables. Pearson chi-square test and the Mann-Whitney U-test were used to determine the statistical significance of categorical and continuous variables, respectively. Categorical variables were stated as numerical value (% of group), and continuous variables were stated as median (interquartile range [IQR]). A predictive model was created using a stepwise method where only variables with a p-value ≤ 0.05 in univariate regression were selected; these variables were then combined into a multivariable regression and removed if the p-value was not ≤ 0.1. The predictive ability of this multivariable model on FTR was analyzed using ROC curve analysis. A web application was created for user-friendly risk calculation of FTR: https://nsgyfrailtyoutcomeslab.shinyapps.io/FailureToRescueTLfusion/.
RESULTS
1. Participants
The study cohort included 15,749 adult patients who underwent TLF at NSQIP-participating institutions between 2011 and 2020.
2. Preoperative Demographic and Clinical Characteristics
The study cohort had a median age of 66 years (IQR, 15 years), was 57.4% female, and 4.7% Hispanic ethnicity. The racial distribution included 80.5% White, 9.3% Black, 1.8% Asian, and 8.4% all other groups (including Native Hawaiian or Other Pacific Islander, American Indian or Alaska Native, and unspecified race). The most prevalent comorbidities within the study cohort were hypertension (65.2%), diabetes mellitus (22.3%), current smoker status (16.9%), and chronic steroid use (6.7%). The FTR cohort was significantly older, more frail, and consisted of a great proportion of male patients. The entire cohort of FTR, and non-FTR subgroups with preoperative demographics and clinical characteristics, are summarized in Table 1.
3. Surgical Outcomes
A small proportion of the study cohort (n= 129, 0.8%) experienced FTR. The most common postoperative complications were bleeding requiring transfusion (80.5%), septic shock (15.2%), sepsis (5.7%), and pneumonia (5.6%). Compared to the non-FTR subgroup, the FTR subgroup experienced significantly greater proportions of poor postoperative outcomes, including renal complications, thrombosis/embolism complications, pneumonia, unplanned intubation, intubation greater than 48 hours, cardiac arrest, myocardial infarction, and septic shock. The postoperative outcomes of the entire cohort, and both FTR and non-FTR subgroups, are summarized in Table 2.
4. Predictors of FTR
In univariate regression, several preoperative and postoperative variables were significantly associated with FTR, including nonelective surgery status (odds ratio [OR], 4.46; 95% confidence interval [CI], 3.11–6.38), RAI (1.13; 1.11–1.15), chronic steroid use (2.26; 1.37–3.74), bleeding disorders (2.24; 1.13–4.43), renal complications (6.32; 3.60–11.15), thrombosis/embolism complications (2.67; 1.60–4.48), pneumonia (4.35; 2.81–6.72), septic shock (8.76; 4.95–15.51), unplanned intubation (28.03; 19.33–40.65), on ventilator ≥ 48 hours (8.17; 4.84–13.79), cardiac arrest (130.61; 84.64–201.56), and myocardial infarction (6.11; 3.68–10.15). It was observed that each stepwise increase in frailty corresponded with an increasing likelihood of FTR. The results of the univariate regression analysis are displayed in Table 2. A frailty-driven multivariable predictive model was created using RAI alongside chronic steroid use, nonelective surgery status, renal complications, unplanned reintubation, cardiac arrest, and bleeding requiring transfusion (Table 3). On ROC curve analysis, this model demonstrated excellent predictive ability for the primary outcome of FTR, with an area under the ROC (AUROC) of 0.918 (95% CI, 0.888–0.947) (Fig. 1).

Multivariable risk factors for failure to rescue (vs. rescued) in patients who experienced a major complication after undergoing thoracolumbar fusion, ACS-NSQIP 2011–2020
DISCUSSION
1. Key Results
In the analysis of 15,749 TLF patients from a prospective international surgical database, increasing frailty, as measured by the RAI, was associated with an increased likelihood of FTR, or 30-day mortality following a major complication. For example, very frail patients, with an RAI score of ≥ 46, had 45-fold increased odds of FTR when compared to patients with RAI 0–20. A multivariable predictive model was created that predicts FTR with an excellent discriminative ability (AUROC, 0.918).
2. Interpretation
The avoidance of 30-day mortality following a major complication, or FTR, is a hospital quality of care metric [19-21]. Nevertheless, the ability to assess healthcare performance based on FTR has been questioned due to wide variance and inconsistency in FTR rates per individual patient characteristics [22]. A NSQIP analysis of FTR in patients who underwent inpatient general, vascular, thoracic, cardiac, and orthopedic surgery found that patients with an RAI score > 40 had a 44-fold increased odds of FTR [23]. Risk-adjusted FTR metrics in patients undergoing cardiac surgery have demonstrated varying FTR rates according to primary complication type, after adjusting for intraoperative characteristics and individual patient predictors of FTR [24]. The wide variance in FTR rates necessitates that the primary care teams implement individualized protocols according to each complication type [25]. Although escalating care after certain complications has reduced mortality, the association between FTR and type of complication challenges its role as a quality metric [26]. Our results support the need for a similar risk-adjusted metric with respect to frailty in patients undergoing TLF [24].
Previous literature has identified patient predictors of FTR in spine surgery [27]. In a study of 10,841 patients undergoing surgery for cervical spine trauma, patients with chronic liver disease had a 2.86-fold higher odds of FTR [28]. Similarly, in patients undergoing resection of metastatic spine tumors, frailty, measured using the New England Spinal Metastasis Score (NESMS), was utilized to develop a predictive model of FTR [13]. Subsequent model performance characteristics revealed a c-statistic of 0.66. In comparison, our model demonstrated a c-statistic of 0.918. Potential reasons for this wide variation could include differences in frailty indexes that were utilized in both studies. The NESMS measures frailty using 3 components—functional dependence, preoperative albumin levels and cancer burden. Unlike NESMS, RAI is a weighted frailty index that considers comorbid conditions in addition to characteristics such as age and functional dependence.
Our study builds on other surgical specialties’ work by identifying frailty and type of complication as predictors of FTR [23,29,30]. The 45-fold increased odds of FTR in patients with RAI > 46 after TLF surgery demonstrates that these patients are predisposed to FTR, or failure to recover following a major complication due to poor baseline physiological reserve. Our multivariate model showed higher rates of FTR following cardiac arrest or renal failure. These findings have been utilized to create a risk-adjusted metric made available in the form of a user-friendly online calculator: https://nsgyfrailtyoutcomeslab.shinyapps.io/FailureToRescueTLfusion.
3. Clinical Implications
Our results suggest that frailty’s impact on FTR can be used to guide perioperative decision-making. In the preoperative setting, prehabilitation before surgery may help reduce the impact of frailty status on adverse events [31]. When patients develop postoperative complications, the likelihood of 30-day mortality from FTR can be estimated with this model. While the results of our study do not intend to withhold surgical treatment or life-saving interventions in the event of a complication, it can be used to guide goals of care discussions by giving patients and their families a better idea of recovery expectations [32]. The ease of calculating RAI scores allows for it to be utilized as a bedside tool to estimate frailty, and subsequent FTR. Further validation of RAI as a predictor of FTR in patients undergoing TLF prior to its incorporation in clinical decision-making.
4. Generalizability
The present study utilized a large, multinational database with over 700 participating institutions across 11 countries, imparting generalizability across hospital system, geographic, and cultural variability. The excellent discriminatory accuracy of the FTR predictive model (AUROC, 0.918) allows for further reliability and clinical utility of these findings.
5. Limitations
Our study is subject to several limitations. While the NSQIP is a widely used and validated database, reporting, and coding bias may occur. This dataset only captures case data for 30 days following surgery, limiting analysis of long-term outcomes, and the RAI was specifically designed to capture mortality rates at 1 year. Granular, specific, surgical case details, including severity and chronicity of disease, operative details, extent of blood loss, and specific infectious pathogens are not available within the NSQIP. While not analyzed, these factors may have affected rates of FTR [33]. NSQIP-participating institutions are typically large, high-volume hospitals associated with lower FTR rates, which may have resulted in an underestimation of these outcomes within the study cohort [5]. Despite the high AUROC in our predictive model, it is to be noted that we did not control for confounders or perform subsequent internal validation of our model.
CONCLUSION
Knowledge of baseline frailty and the likelihood of FTR following the development of a specific complication may provide patients and clinicians with a more informed prognosis during the decision-making process. This has been incorporated in the form of an open-access, online calculator to facilitate informed decision-making in the event of a complication after TLF surgery: https://nsgyfrailtyoutcomeslab.shinyapps.io/FailureToRescueTLfusion/.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: JMR; Data curation: ASC, KR; Formal analysis: ASC, KR; Methodology: ASC, KR; Project administration: JMR, CAB; Visualization: CAB; Writing - original draft: JMR, GPS; Writing - review & editing: JMR, ASC, GPS, KR, MMC, CAB.