- Search
| Neurospine > Volume 17(3); 2020 > Article |
|
|
Abstract
Although cervical spinal deformity (CSD) can have a profoundly negative impact on an individual’s quality of life and there have been many advances in surgical treatment of CSD in recent years, there exists no comprehensive classification system of surgical treatment that categorizes anterior and posterior surgery separately according to the grade of surgery. The objective of this study is to introduce the new classification system of various surgical treatments for CSD. We developed a new classification system (SOF system) for CSD surgery that describes the sequence of surgical approach (S), the grade of osteotomy (O), and the information of fixation (F) using alphanumeric codes. This new classification system can provide a consistent description of the various osteotomies performed in CSD surgery. Especially, regarding research, there has been a clear benefit to this classification. Having a standardized classification that allows for common frame for cervical deformity correction surgery, communication between surgeons and the evaluation of the CSD surgeries make it possible to conduct global comparative research about surgical outcome.
There have been increasing evidence demonstrated correlations of cervical spinal parameters with health-related quality of life and the incidence of cervical spondylotic myelopathy (CSM) [1-3].
Recently, understanding of the cervical sagittal alignment and surgical methods have been developed [3-9]. So, surgical treatment of cervical spinal deformity (CSD) become a subject of interest. However, surgical correction of CSD can be challenging not only because it often requires osteotomies to obtain adequate correction especially in the setting of rigid CSD, but also because the target of surgical correction is adjacent to the critical neurovascular structures [8,10-26]. Thus, the postoperative complications have been reported to be relatively high and the number of studies on CSD are far inferior to those of thoracolumbar deformity.
Although there have been recent advances in standardized classification and nomenclature system for osteotomy technique to manage adult thoracolumbar deformity, there have been few classification systems for CSD surgeries that systematically organizes the anterior and posterior cervical osteotomy techniques respectively [3,7,27-29]. Moreover, there is lack of standardization regarding surgical approach and surgical technique for CSD.
So, the purpose of this study was to introduce a new nomenclature system that can briefly describe the surgical approach, the grade of osteotomy, the sequence of CSD surgeries, and the information of fixation.
SOF system was designed to describe the sequence of surgical approach, the grade of osteotomy, the sequence of CSD surgeries, and the information of fixation techniques using alphanumeric codes. All CSD surgeries using the SOF classification are given an APF (anterior, posterior, fixation) description.
• S describes the sequence of surgical approach - Description sequence of A and P is the order of surgical approach. If the anterior surgery is performed first, A is described first. If posterior surgery is performed first, P is first written.
• O describes the technique and grades of osteotomy. Grades of osteotomies correspond to the extent of bony resection and increasing degree of destabilizing potential.
• A (0, 1, 2, 3, 4): Anterior osteotomies are divided into 4 grades (Table 1). A0 means that anterior approach is not performed for the CSD correction.
• P (0, 1, 2, 3, 4, 5, 6): Posterior osteotomies are divided into 6 grades proposed by Schwab et al. for the treatment of thoracolumbar deformity (Table 2). P0 means that posterior approach is not performed for the CSD correction. Although vertebral column resection (VCR) may not be an appropriate procedure for the cervical spine because of the vertebral artery and functioning nerve roots, sometimes upper thoracic VCR is indicated for the treatment of cervicothoracic deformity. Thus, it was included as grade 6 posterior osteotomy (P6) for CSD.
• F: F stands for fixation technique and describes the level and methods of fixation. Fixation techniques are divided into 3 methods (Table 3).
In situ fixation (IF) could only be indicated if the CSD is reducible with positional change such as neck extension. Depending on the deformity apex location and extent, anterior IF (AIF) or posterior IF (PIF) can be used.
Sometimes osteotomy is needed to realign the spine.
Compressive fixation (CF) could be used when osteotomy is needed to realign the spine.
If posterior CF (PCF) is necessary after posterior column shortening osteotomies (SPO, PSO, and VCR), sequential compression against the screws’ head should be performed.
Distractive fixation (DF) could be useful, especially for focal deformity. Anterior DF (ADF) or posterior DF (PDF) can be used depending on the surgical approach and the apex of the deformity.
A 39-year-old woman presented with chronic neck pain and limited neck motion due to old fracture of C5–6. Imaging studies showed semirigid focal cervical kyphosis with canal impingement. Authors corrected her semirigid focal kyphosis with C56 anterior corpectomy and instrumentation (Fig. 1), it can be expressed as “A2 (C5-6); ADF (C4–7)/P0”
A 79-year-old woman presented with neck pain, severe occipital headache, and abnormal neck tilt. Imaging demonstrated an asymmetrical C1–2 joint mutilation, atlantoaxial rotatory fixation (AARF), and C2 root impingement (Fig. 2).
Posterior only surgery was performed. Unilateral C1–2 facet joint distraction, AARF reduction, and intra-articular facet fusion were necessary to correct neck tilt caused by the osteoarthritis. Posterior C1–2 instrumentation was performed using Goel-Harms technique. These procedures can be expressed as follows; “A0/P1 (C1–2); PDF (C1–2)”.
A 40-year-old woman presented with chronic neck pain and progressive quadriparesis due to os odontoideum. Imaging studies showed upper cervical kyphosis with canal impingement. Authors corrected her upper cervical kyphosis (Fig. 3) with C1–2 facet joint release and intra-articular fusion. Finally, posterior compressive fixation (PCF) was done for posterior column shortening at C1–2, it can be expressed as “A0/P1 (C1–2); PCF (C1–2)”
A 50-year-old man presented with a history of progressive cervical axial pain, gait disturbance, and bilateral hand clumsiness. He had been diagnosed with rheumatoid arthritis and had been taking medication for 10 years in another hospital. Physical examination evidenced hyperreflexia and painful neck motion limitation of all movements (flexion, extension, and lateral bending). Plain radiographs of the cervical spine showed a cervical malalignment, and atlantoaxial subluxation (Fig. 4). A cervical magnetic resonance imagign was performed, and multilevel CSM was visualized in the subaxial cervical spine.
Single staged A-P surgery was performed. We initially performed multilevel anterior uncovertebral joint resection and fusion from C3 to C7. Then, posterior column osteotomy was performed at C3–7, facet joint release and intra-articular fusion was done at C1–2 level. Finally, PCF was done for posterior column shortening from C1 to C7. The procedure and the extent of osteotomy and the extent of fixation can be described as “A3 (C3–7)/P1 (C1–2); P2 (C3–7); PCF (C1–7)”.
A 37-year-old man presented with a history of progressive cervical axial pain, refractory to analgesics and opioids, difficulty in swallowing, and inability to walk with a horizontal gaze. He had been diagnosed with ankylosing spondylitis (AS) in another hospital. Physical examination evidenced the inability to move his neck, with limitation of all movements.
Plain x-ray showed a fixed cervical kyphosis, with evident bone fusion in the anterior and posterior elements of his spine (Fig. 5).
When C7 pedicle subtraction osteotomy was needed in the case of severe AS, it can be expressed as “A0/P4 (C7); PCF (C2–T3)”
Despite considerable progress in classification and recommended strategies for treatment of thoracolumbar deformities, advances of CSD have lagged comparatively [7,28,29].
It is not only because the pathologies of CSD are more heterogeneous but also surgical strategies and classification of the CSD is not yet fully established. In addition, relatively lower incidence of CSD could be an obstacle to advance the CSD surgery.
In addition, most of thoracolumbar spine deformity can be treated by the posterior only surgery, so it could be simple to express the surgical grade of thoracolumbar deformity. However, CSD surgery has a variety of approaches (anterior approach, posterior approach, simultaneous anteriorposterior approach, and 540° approach) because of the surrounding neurovascular structures, so expressing surgical grade of CSD surgery could be rather complicated [15,19,20,22-24,30].
Recently, a classification system has been developed to standardize the description of cervical osteotomy types [3]. This system is a 7-point scale based on anatomical resections that are graded according to the potential for destabilization. Although it is designed to be comprehensive as to include the wide range of surgical resections that may be performed for cervical deformity correction, this system is too complicated to remember because the anterior and the posterior osteotomy techniques are not separated in this system. Moreover, it is impossible to describe the operation sequence and the fixation details together using this system.
The range of cervical osteotomy can be divided into several grades according to the amount of bony resection and destabilization in each approach. In addition, spinal deformity surgery should be able to express the scope of spinal fixation because it involves the segmental fixation surgery.
Standardized techniques for various surgical options are essential for any disease to obtain consistent surgical result and validate the effectiveness of treatment. Multicenter studies are needed to evaluate the treatment efficacy of diseases that are rare and have relatively short history of surgical treatment such as CSD.
To facilitate communication and effective data analysis among researchers, standardized techniques are needed to systematically express ratings.
Therefore, it is necessary to have a standardized nomenclature system that can facilitate communication among researchers and effective evaluation of the surgical results by simultaneously expressing various surgical techniques of CSDs.
So, authors designed a new nomenclature system that can easily express the most important factors in the technique of cervical deformity surgery, such as the method of osteotomy, surgical approach, operation sequence, and detail of fixation.
This new classification system (SOF system) for CSD surgeries is devised to be like the TNM staging system for the tumor evaluation. Before TNM classification, there were myriads of systems of staging of cancer. Nowadays, the staging system has somewhat been standardized to the use of 3 elemental parameters, the tumor (T), the node (N), and the distant metastasis or spread (M), constituting the so-called TNM staging system [31-33]. The TNM classification has been accepted as a global standard to ensure that adequate treatment can be planned, then an accurate prognosis can be given, and that there is a uniform system to evaluate the results of treatment [34-37].
Fundamentally, proposed SOF system for CSD surgeries consists of 3 elements (S, O, F).
S, O, and F indicate the sequence of surgical approach (S), technique and grade of osteotomy (O), and fixation techniques (F).
SOF classification system is not designed to describe the surgical indication, efficacy, prognosis, or optimal surgical approach for each different type of CSD.
Instead, this new osteotomy classification is an anatomical and technical description system to understand the sequence of the surgical correction, the grade of osteotomy, and the fixation techniques in detail.
SOF system can be used as a standard classification system on all kinds of CSD surgery because its basic principles are; (1) applicability to all anatomic sites; (2) the capability to describe the surgical approach (anterior or posterior) and the sequence of surgical treatment (single anterior, single posterior, combined approach or 540° surgery; A-P-A, P-A-P); (3) the capability to describe the different osteotomy grade, level, and method of fixation; (4) facilitate the exchange of information not only between surgeons but also between treatment centers; (5) contribute to the continuing investigation of CSD.
Although several modifiers may need to be added, this new classification system allows independent communication between other researchers. Also, it will enable assessment and validation by other groups and through other databases.
However, in order for SOF classification to be recognized as a standard classification and widely used, it is necessary to study the reliability of whether consistent description among surgeons is possible. The investigation of the inter- and intraobserver agreement will be the subject of the next study.
We proposed a new nomenclature system (SOF system) which designed to systematically describe the sequence of the surgical correction, the grade of osteotomy, and detail of the fixation techniques of the CSD surgery.
SOF system can be a valuable tool to provide a consistent description of the various osteotomies performed in CSD surgery. Having a standardized classification that allows for common frame for CSD surgery, communication between surgeons and the evaluation of the CSD surgeries make it possible to conduct global comparative research about surgical outcome. However, further multicenter study is necessary to confirm whether the classification system is consistent and effective.
Fig. 1.
Intraoperative photograph shows correction procedure of focal cervical kyphosis with C56 anterior corpectomy, it can be expressed as “A2 (C5–6); ADF (C4–7)/P0”.
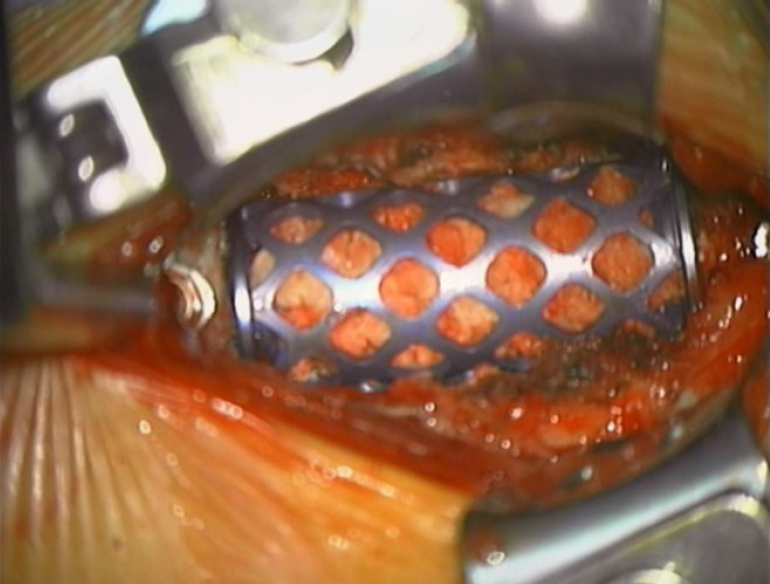
Fig. 2.
(A) Preoperative computed tomography reconstruction image demonstrating severe joint mutilation causing atlantoaxial rotatory fixation at right side C1–2 joint (white arrow). (B) Intraoperative photograph showing intra-articular cage insertion at right C1–2 joint space. It can be expressed as “A0/P1 (C1–2); PDF (C1–2)”. PDF, posterior distractive fixation.
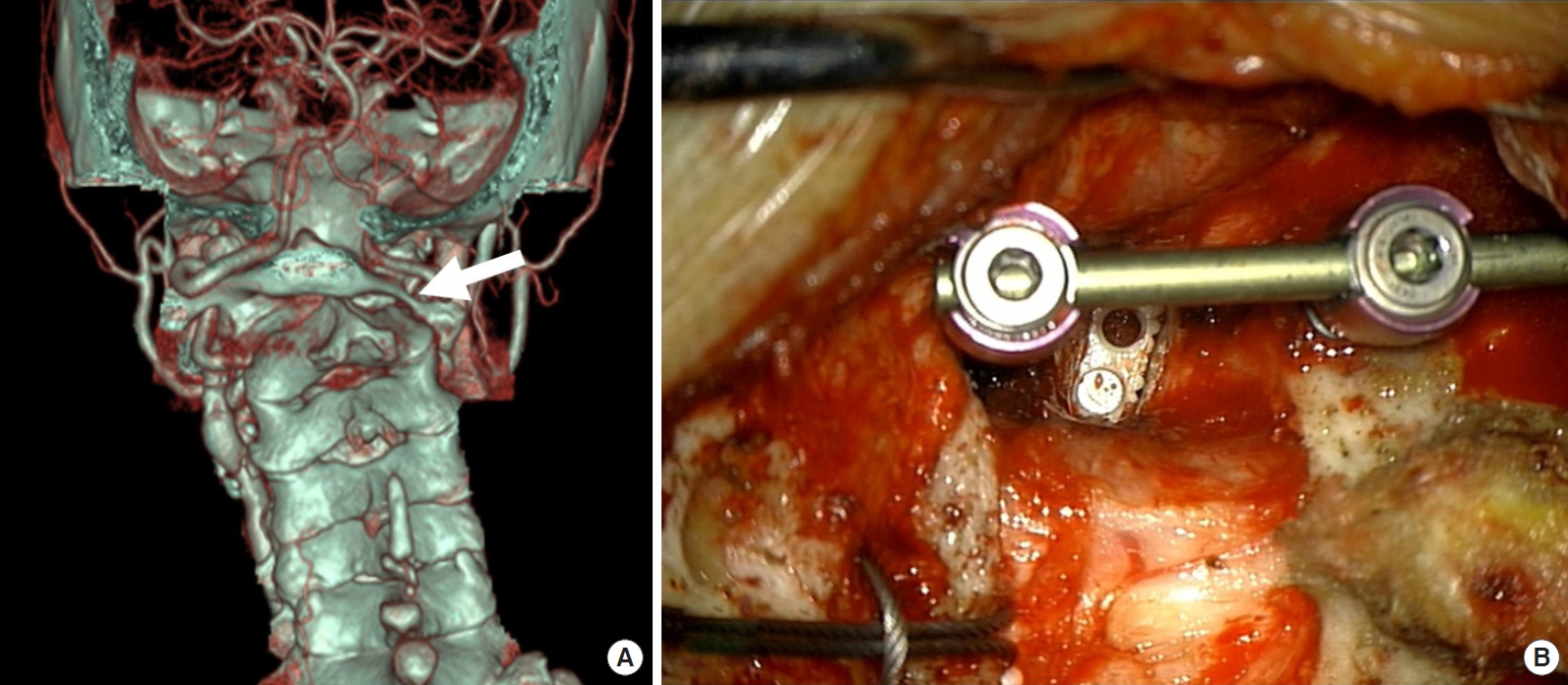
Fig. 3.
(A) Preoperative radiograph shows upper cervical kyphosis due to os odontoideum. (B) Preoperative computed tomography sagittal reconstruction image demonstrating os odontoideum and subluxated dens compressed spinal canal. (C) Preoperative T2-weighted sagittal magnetic resonance (MR) image demonstrating severe cord compression and cord signal change at C1–2 level. (D) Postoperative radiograph showing C1–2 intra-articular graft insertion (arrow) and lordotic correction of upper cervical alignment. It can be expressed as “A0/P1 (C1–2); PCF (C1–2)”. (E) Postoperative T2-weighted sagittal MR image demonstrating good reduction of C1–2 subluxation and cord decompression at C1–2 level. PCF, posterior compressive fixation.
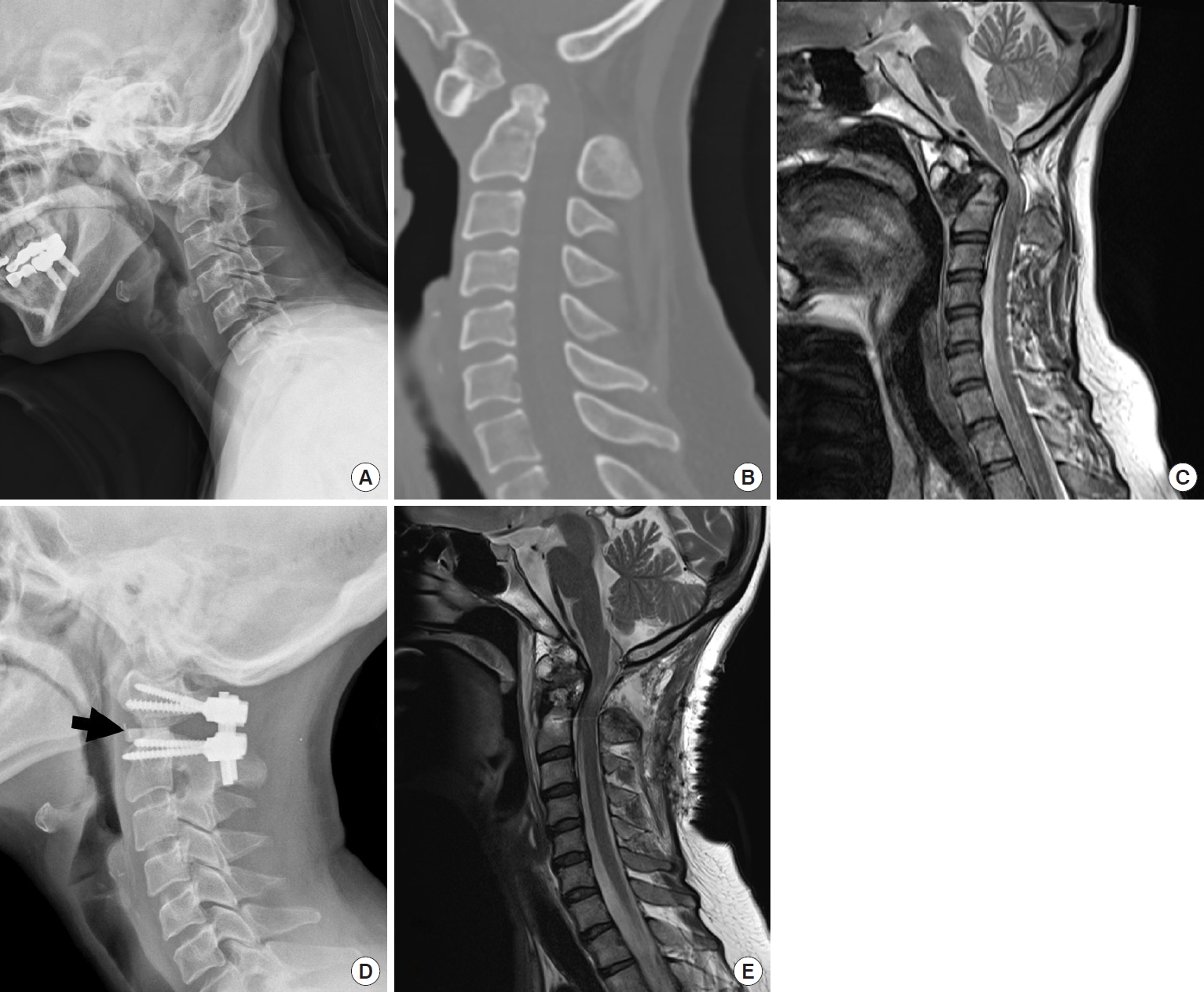
Fig. 4.
(A) Lateral preoperative radiograph demonstrating atlantoaxial subluxation and subaxal cervical kyphosis. (B) Preoperative computed tomography (CT) sagittal reconstruction image demonstrating occipitocervical collision (black arrow) caused by rheumatoid basilar invagination. (C) Preoperative T2-weighted sagittal magnetic resonance image demonstrating multilevel cord compression and cord signal change from C1 to C7. (D) Lateral postoperative radiograph demonstrating anterior buttress plate fixation and improved sagittal balance of the neck after the surgery. The procedure and the extent of osteotomy and the extent of fixation can be described as “A3 (C3–7)/P1 (C1–2); P2 (C3–7); PCF (C1–7)”. (E) Preoperative CT sagittal reconstruction image demonstrating sound interbody fusion in the subaxial cervical spine and reduction of basilar invagination. PCF, posterior
compressive fixation.
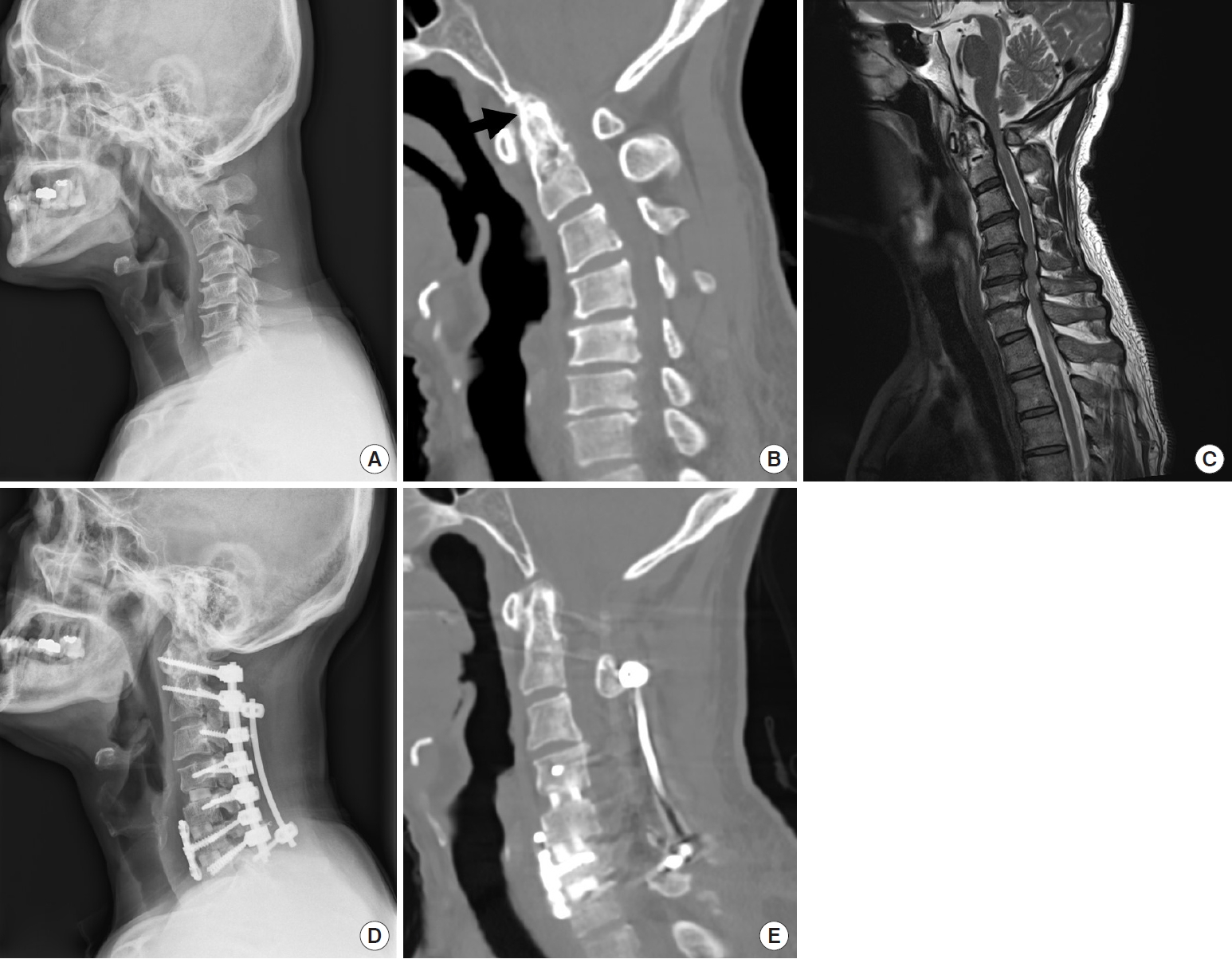
Fig. 5.
(A) Lateral preoperative radiograph demonstrating fixed sagittal imbalance and ankylosing spondylitis in cervical spine. (B) Postoperative radiograph shows C7 PSO (arrow), deformity correction, and instrumentation. Pedicle subtraction osteotomy at C7 level and PCF from C2–T3 can be expressed as “A0/P4 (C7); PCF (C2–T3)”. PSO, pedicle subtraction osteotomy; PCF, posterior compressive fixation.

Table 1.
Anterior osteotomy classification
Table 2.
Posterior osteotomy classification
REFERENCES
1. Koller H, Ames C, Mehdian H, et al. Characteristics of deformity surgery in patients with severe and rigid cervical kyphosis (CK): results of the CSRS-Europe multi-centre study project. Eur Spine J 2019 28:324-44.



2. Cho SK, Safir S, Lombardi JM, et al. Cervical spine deformity: indications, considerations, and surgical outcomes. J Am Acad Orthop Surg 2019 27:e555-67.


3. Ames CP, Smith JS, Scheer JK, et al. A standardized nomenclature for cervical spine soft-tissue release and osteotomy for deformity correction: clinical article. J Neurosurg Spine 2013 19:269-78.


4. Xiaolong S, Xuhui Z, Jian C, et al. Weakness of the neck extensors, possible causes and relation to adolescent idiopathic cervical kyphosis. Med Hypotheses 2011 77:456-9.


5. Lamartina C, Berjano P. Classification of sagittal imbalance based on spinal alignment and compensatory mechanisms. Eur Spine J 2014 23:1177-89.



6. Smith JS, Lafage V, Schwab FJ, et al. Prevalence and type of cervical deformity among 470 adults with thoracolumbar deformity. Spine (Phila Pa 1976) 2014 39:E1001-9.


7. Ames CP, Smith JS, Eastlack R, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine 2015 23:673-83.


8. Tan LA, Riew KD, Traynelis VC. Cervical spine deformity-Part 1: biomechanics, radiographic parameters, and classification. Neurosurgery 2017 81:197-203.



9. Diebo BG, Shah NV, Solow M, et al. Adult cervical deformity: radiographic and osteotomy classifications. Orthopade 2018 47:496-504.



10. Lee JS, Son DW, Lee SH, et al. The Predictable factors of the postoperative kyphotic change of sagittal alignment of the cervical spine after the laminoplasty. J Korean Neurosurg Soc 2017 60:577-83.




11. Passias PG, Horn SR, Jalai CM, et al. Comparative analysis of perioperative complications between a multicenter prospective cervical deformity database and the Nationwide Inpatient Sample database. Spine J 2017 17:1633-40.


12. Smith JS, Shaffrey CI, Bess S, et al. Recent and emerging advances in spinal deformity. Neurosurgery 2017 80:S70-85.



13. Park JH, Lee JB, Kim IS, et al. Transdiscal C7 pedicle subtraction osteotomy with a strut graft and the correction of sagittal and coronal imbalance of the cervical spine. Oper Neurosurg (Hagerstown) 2020 18:271-7.



14. Hong JT, Oh JS, Lee DH, et al. Association between the severity of dysphagia and various parameters of the cervical spine; videofluoroscopic analysis in neutral and retraction position of the normal volunteers. Spine (Phila Pa 1976) 2020 45:103-8.


15. Hong JT, Espinoza Orías AA, An HS. Anatomical study of the ventral neurovascular structures and hypoglossal canal for the surgery of the upper cervical spine. J Clin Neurosci 2020 71:245-9.


16. Lee CH, Hong JT, Kang DH, et al. Epidemiology of iatrogenic vertebral artery injury in cervical spine surgery: 21 multicenter studies. World Neurosurg 2019 126:e1050-4.


17. Park JH, Lee JB, Lee HJ, et al. Accuracy evaluation of placements of three different alternative C2 screws using the freehand technique in patients with high riding vertebral artery. Medicine (Baltimore) 2019 98:e17891.



18. Kim HS, Lee JB, Park JH, et al. Risk factor analysis of postoperative kyphotic change in subaxial cervical alignment after upper cervical fixation. J Neurosurg Spine 2019 Apr 26 1. -6. https;//doi.org/10.3171/2019.2.SPINE18982. [Epub].

19. Lee JJ, Hong JT, Kim IS, et al. Significance of multimodal intraoperative monitoring during surgery in patients with craniovertebral junction pathology. World Neurosurg 2018 118:e887-94.


20. Lee HJ, Kim JH, Kim IS, et al. Anatomical evaluation of the vertebral artery (V2) and its influence in cervical spine surgery. Clin Neurol Neurosurg 2018 174:80-5.


21. Park WB, Hong JT, Lee SW, et al. Clinical and radiological comparison between ipsilateral and contralateral side canal decompression using an unilateral laminotomy approach. Korean J Spine 2016 13:41-6.




22. Hong JT, Kim IS, Kim JY, et al. Risk factor analysis and decision-making of surgical strategy for V3 segment anomaly: significance of preoperative CT angiography for posterior C1 instrumentation. Spine J 2016 16:1055-61.


23. Lee HJ, Kim IS, Sung JH, et al. Significance of multimodal intraoperative monitoring for the posterior cervical spine surgery. Clin Neurol Neurosurg 2016 143:9-14.


24. Kwon JY, Kim IS, Hong JT, et al. Intramuscular myxoma of the lumbar paravertebral muscle. Spine J 2016 16:e451-2.


25. Lee HJ, Lee JJ, Hong JT, et al. Quantification of pediatric cervical growth: anatomical changes in the sub-axial spine. J Korean Neurosurg Soc 2015 57:185-91.




26. Kim IS, Hong JT, Jang WY, et al. Surgical treatment of os odontoideum. J Clin Neurosci 2011 18:481-4.


27. Bakouny Z, Khalil N, Otayek J, et al. Are the sagittal cervical radiographic modifiers of the Ames-ISSG classification specific to adult cervical deformity? J Neurosurg Spine 2018 29:483-90.


28. Schwab F, Blondel B, Chay E, et al. The comprehensive anatomical spinal osteotomy classification. Neurosurgery 2014 74:112. -20. discussion 20.



29. Rajasekaran S, Kanna RM, Shetty AP. Management of thoracolumbar spine trauma: an overview. Indian J Orthop 2015 49:72-82.



30. Dru AB, Lockney DT, Vaziri S, et al. Cervical spine deformity correction techniques. Neurospine 2019 16:470-82.




31. Miyazawa M, Shiina T, Kurai M, et al. Assessment of the new TNM classification for resected lung cancer. Kyobu Geka 2000 53:915-8.

32. Oda M, Kanamori T, Marukawa Y, et al. Evaluation of new TNM classification for lung cancer, especially T3N0M0, stage IIIA, stage IIIB, and pm. Kyobu Geka 2000 53:905-9.

33. Saito Y, Yamakawa Y, Kiriyama M, et al. Evaluation of new TNM lung cancer classification. Jpn J Thorac Cardiovasc Surg 2000 48:499-505.



34. Sakata S, Kawashima O, Ibe T, et al. Evaluation of TNM classification for lung carcinoma with satellite nodules in the same lobe as the primary. Kyobu Geka 2000 53:926-8.

35. Marsh JW, Dvorchik I, Bonham CA, et al. Is the pathologic TNM staging system for patients with hepatoma predictive of outcome? Cancer 2000 88:538-43.



- TOOLS
-
METRICS

-
- 0 Crossref
- Scopus
- 4,638 View
- 172 Download
-
Journal Impact Factor 3.8
SURGERY: Q1
CLINICAL NEUROLOGY: Q1





























